Almost 2 billion people have hepatitis B markers, more than 350 million are carriers of the virus. Every year, 1 million people die from hepatitis and its consequences.
These data refute the belief of many that hepatitis B is a rare infection. In fact, the disease is very common and can affect anyone. Vaccination against hepatitis B minimizes the risk of infection, but even if infection occurs, the disease is much easier to tolerate and does not pose dangerous consequences. Since 2002, vaccination against hepatitis B has been included in the Russian compulsory vaccination calendar. Vaccination against hepatitis A for children is recommended.
In the PreAmbula network of clinics, when vaccinating against hepatitis A and B, only high-quality vaccines from reliable manufacturers are used. Before vaccination, a doctor’s examination is required, and a specialist only gives permission for vaccination to a healthy child.
Hepatitis A and B – similarities and differences
Both forms of hepatitis are viral in nature. Infection with hepatitis A usually occurs through household means; it is not for nothing that the disease is called “the disease of unwashed hands.” Hepatitis B is transmitted only through human blood and other body fluids.
Hepatitis A, the well-known jaundice or Botkin's disease, does not cause complications, responds well to therapy and is considered a relatively safe disease. The danger of hepatitis B lies in the formidable complications that threaten not only health, but also human life - liver cancer, liver failure, cirrhosis.
Goals of vaccination
The consequences of this disease are dramatic, as more than 800,000 people die from hepatitis B every year. Vaccination is not just the main and important means of preventing viral hepatitis, but also the possibility of protection against liver cancer. The basis for preventing this disease is a vaccine. According to the recommendations of the World Health Organization, all babies should be vaccinated on the first day of their life.
It is important to understand that after vaccination, more than 95 percent of infants, children of other ages and young adults develop protective levels of antibodies that last for twenty years, and for some, a lifetime.
Hepatitis vaccination schedule
Hepatitis B vaccines are recombinant - they contain artificial antigens (unlike the hepatitis A vaccine based on a live virus). The artificial origin of the vaccine is a guarantee of complete safety and long-term immunity to hepatitis B. But at the same time, recombinant vaccines are not as effective as vaccines based on the live virus. Therefore, if a single vaccination is sufficient to develop stable immunity against jaundice, three-time administration of the vaccine is necessary to form high-quality immunity against hepatitis B.
Vaccine effectiveness
The hepatitis B vaccine is safe and effective and has been used since 1982. Since then, more than 1,000,000,000 doses of vaccine against this disease have been administered worldwide.
Statistics show that vaccination has had an impact on reducing rates of chronic hepatitis among immunized people.
A course of immunization produces immunity in 90% of those vaccinated. Vaccinations can reduce the incidence of hepatitis by 30 times and prevent many deaths that occur due to hepatitis B. In addition, the risk of the disease in those born to infected mothers is reduced by 20 times.
Most researchers call the hepatitis B vaccine the "cancer vaccine." This is because it prevents the spread of infection, which can ultimately lead to the development of carcinoma.
Three hepatitis B vaccination schedules
- Basic (standard): 0-1-6 months
Hepatitis vaccination for a newborn child (in the absence of contraindications), then when the baby reaches 1 month of age, and the third vaccination at 6 months. - Alternative (fast): 0-1-6-12 months
Prescribed for vaccination of children with an increased risk of contracting the virus. - Emergency: 0-7-21 days – 12 months
In case of probable contact with the hepatitis B virus.
What to do if the scheme is broken?
If the newborn has not been vaccinated against hepatitis B, immunization can begin at any age (the main requirement is a healthy child). The time interval between the first and second vaccination should not exceed 4 months, and the third vaccination is carried out 4-18 months after the second.
It is not always possible to accurately follow the vaccine administration schedule due to the child’s illness or other reasons, so there is an acceptable interval during which the vaccine can be given.
For a standard schedule, the second vaccination should be done with a delay of up to 4 months, and the third - no earlier than 4 months and no more than 18 months after the second. If more than 4 months have passed and the second vaccination has not been done, the regimen is started again. If the third vaccination is missed, they resort to option 0-2 (vaccination is carried out, and after 2 months it is repeated). If immunization was started several times and the vaccine was eventually administered 3 times, the course is considered complete - long-term immunity to hepatitis B has been formed.
There is no vaccination schedule for hepatitis A, but doctors recommend it for all children starting at one year of age. And especially if:
- there is an infected person in your immediate environment;
- you will be traveling to a country with a socially low level;
- liver pathology was diagnosed.
In the latter case, vaccination is mandatory.
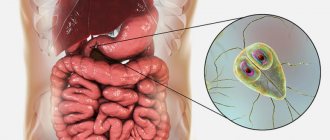
Hepatitis
is a diffuse inflammatory disease of the liver, the cause of which can be either infectious or non-infectious in nature.
Among infectious hepatitis, the most common are those with a viral nature of the lesion. There are 8 known hepatotropic viruses.
Viral hepatitis A, E, F, with fecal-oral transmission. After an infection, immunity remains stable and lifelong.
Viral hepatitis B, C, D, G, TTV, SAN, with parenteral transmission (through a needle, medical procedures, using non-sterile, reusable instruments, tattoos, transfusion of infected blood), with sexual transmission, vertical transmission (from mother to child) may become chronic.
To protect yourself and your loved ones, specific prevention (administration of vaccines) is required.
Vaccines are sterile suspensions of inactivated viral particles grown in human cell culture, concentrated and adsorbed on aluminum hydroxide.
Hepatitis A
List of vaccines against hepatitis A
in the Russian Federation:
- GEP-A-in-VAK, Algavak (RF);
- Harvix (Belgium);
- Avaxim (France);
- Waqta (USA).
Who needs vaccination?
For those who are or will be at risk of infection:
- People traveling (military personnel, travelers, etc.) to areas with high incidence rates (most countries of the Asian, African and South American continents);
- Contact with patients;
- People at occupational risk of infection: medical personnel and caregivers; employees of child care institutions; sewer and water supply workers; food industry and catering personnel;
- People from special risk groups (patients with chronic liver diseases, patients with immunodeficiency, including HIV infection).
Before traveling to an endemic region, the vaccine should be administered at least 2-4 weeks before travel. A vaccination course that provides long-term protection consists of two vaccinations given at intervals of 6-12 months. Before routine vaccination, it is recommended to monitor the protective antibody titer!
Persons aged 18 years and older - 1 ml, intramuscularly.
Contraindications:
- allergic reactions to any component of the vaccine;
- acute infectious and non-infectious diseases, exacerbations of chronic diseases. The vaccination is carried out no earlier than 2-4 weeks after recovery.
- pregnancy (there is no sufficient data on the use of the vaccine in humans during pregnancy).
Adverse events:
In some cases, vaccinated individuals may experience malaise, headache, and low-grade fever. Sometimes there is pain at the injection site, as well as redness or swelling, which most often disappears after 1-2 days.
Hepatitis E
Currently, the only hepatitis E vaccine licensed for use is from China. The vaccine is sold under the trade name HEV 239 or Hecolin. It is used in people aged 16-65 years who have a high risk of HEV infection due to their profession or lifestyle, and can also be used to stop outbreaks of the disease.
The Hecolin vaccine contains 30 μg of recombinant protein synthesized with HEV and adsorbed on aluminum hydroxide.
The drug is administered 3 times according to the following scheme: 0, 1 and 6 months.
Already after the second administration of the drug, sufficient production of antibodies for protection is achieved.
Contraindications are the same as for most inactivated vaccines.
Currently, no significant adverse events have been identified.
Hepatitis B
In Russia, modern, recombinant vaccines are used that contain the surface antigen (HBsAg or Australian antigen) of the virus produced by yeast cells. A section of the virus gene is inserted into the DNA of the yeast cell, and the vaccine, in turn, is produced precisely from a culture of a recombinant yeast strain.
List of hepatitis B vaccines
in the Russian Federation:
- Combiotech (RF);
- Regevak V (RF);
- Euvax B (Korea);
For whom it is especially important to get vaccinated:
— People who come into contact with HBsAg-positive people, both intimately and in everyday life;
— Sexually active people, with frequent changes of sexual partners;
— People with sexually transmitted diseases;
— People with HIV infection;
— People with viral hepatitis C;
— People with chronic liver diseases;
— Medical and social workers, people of various professions (firefighters, landscapers, law enforcement officials, etc.), especially those in contact with blood and biological fluids;
- People on hemodialysis;
— Travelers traveling to regions where there is a high level of infection;
— Men who have sex with men (MSM);
— Injecting drug users;
— People undergoing interventions related to violation of the integrity of the skin and mucous membranes (tattoos, piercings, acupuncture, surgeries, etc.);
— Patients undergoing frequent invasive methods of examination and treatment (endoscopic, gynecological examinations);
Accordingly, we can conclude that EVERYONE should be vaccinated!
An absolute contraindication is allergic reactions to the components of the vaccine, especially to products containing baker's yeast (bread, beer, kvass, confectionery, etc.) and to a previously administered vaccine;
In case of an acute infectious disease, it is worth postponing vaccination for 2-4 weeks;
Routine immunization for a patient with a chronic disease is carried out upon the onset of remission - complete or maximum achievable, against the background of maintenance treatment;
The decision to immunize is made by the doctor based on an assessment of the patient's condition.
Regimen and dosage:
Before vaccination, an antibody titer test (Anti-HBsAg) is required to determine the presence of the Australian antigen.
— For people who have not previously been vaccinated or who have no data on vaccination, the standard regimen of 0-1-6 months is recommended;
— If antibodies to HBsAg are less than 100, a single injection of the vaccine is required, less than 10 – standard administration;
— A single dose is 1.0 ml (20 mcg HBsAg);
— For patients in hemodialysis departments, the vaccine is administered in a double dose of 2 ml (40 mcg HBsAg), four times according to the scheme 0-1-2-6 months.
— The vaccine is administered intramuscularly, subcutaneous administration is undesirable due to a decrease in the immunization effect;
— Vaccination of previously unvaccinated persons who have had contact with infected material (as early as possible, up to 72 hours) is carried out according to the scheme 0-1-2-12 months.
Undesirable effects
Recombinant vaccines have low reactogenicity and are well tolerated.
There may be minor local reactions (redness, swelling and pain at the injection site), weakness, aching joints, a slight increase in temperature, which disappear after 2-3 days.
Hepatitis C
Currently, there is no vaccine for hepatitis C, for several reasons, and has been the subject of debate for many years among leading experts in the world.
Firstly, this is the heterogeneity of the virus. There are 6 main genotypes of the virus and about 500 subtypes. The set of virus variants in each infected patient may differ and change during the course of the disease due to errors during virus propagation. Therefore, the virus represents a complex, time-varying target for the immune system of a sick person. Another problem in creating reliable protection is the lack of stable immunity, that is, re-infection with either the same subtype of the virus or another is possible.
Prevention includes:
1. Reducing the risk of infection:
- testing of donor blood;
- training of medical and cosmetology personnel (hand hygiene, use of gloves, proper handling of medical instruments, safe handling of sharp objects and their proper disposal);
- using condoms;
- drug addiction treatment;
2. Early diagnosis (mass screening of the population) and treatment of patients aimed at the complete destruction of the virus.
Accordingly, the main method of control is antiviral therapy.
WHO recommends treatment for all persons with chronic HCV infection.
Thanks to new, modern drugs with direct antiviral action, it is possible to achieve a complete virological response, thereby stopping the progression of the disease, reducing the incidence of liver cancer and stopping the transmission of the virus.
Hepatitis G
Another type of blood-contact virus that has been little studied.
It often occurs as a co-infection when it joins viral hepatitis B, C.
A vaccine against Hepatitis G has not yet been developed. Most likely due to rare isolated detection and low incidence compared to other hepatitis.
Treatment involves the use of interferon therapy.
Experienced infectious disease doctors see ID-Clinic; if you have questions about vaccine prevention of any diseases, you can sign up for a consultation
Author: Monakhov Nikita Eduardovich
Possible side effects from vaccination
Due to the high effectiveness of the vaccine, leading manufacturers are reducing dosages and completely eliminating preservatives from its composition. This further minimizes the occurrence of adverse reactions. However, each child’s body is individual and may respond to the hepatitis A and B vaccine in the following ways:
- slight malaise and weakness;
- increased sweating;
- redness and itching at the injection site;
- increased body temperature;
- diarrhea.
Parents should know that such manifestations are observed in only 5% of cases and are considered normal. After some time (1-2 days), the child’s condition stabilizes.
After vaccination, the injection site should be protected from contact with water. If water does get on the graft, there is no need to panic - carefully blot the injection site.
Post-vaccination complications
Post-vaccination complications are very rare. On average, with a frequency of 1 in several hundred thousand children who received the vaccine. Severe complications – 1 in several million.
Complications after vaccination are divided into several large groups:
- Reaction to vaccine components. Such reactions include:
- development of an acute allergic reaction: Quincke's edema, urticaria, anaphylactic shock. Most often, these conditions occur without consequences, provided that assistance is provided in a timely and correct manner;
- a piercing scream. Occurs more often after DPT. 2-8 hours after vaccination, the child cries loudly, turning to squealing, for about 3 hours. This is a very unpleasant complication for parents, but it does not threaten the baby in any way.
- severe muscle weakness that goes away on its own. Occurs approximately 1-3 hours after vaccination.
- Reactions due to the quality of the vaccine. This includes changes that arise as a result of violations of the conditions of production, storage, and transportation of vaccines. When using such vaccinations, the following may occur:
— loss of vaccine activity (immunity is not formed);
- increased risk of severe local reactions;
- acute inflammatory changes (abscesses or phlegmon). This happens when the sterility of the drug is violated.
- Reactions caused by violation of the rules of drug administration. This reaction is typical for the BCG vaccine. If it is administered incorrectly intramuscularly, or subcutaneously, and not intradermally, an abscess may develop. When the vaccine is administered into the gluteal muscle, instead of the tibialis or deltoid, the risk of injury to the sciatic nerve and the development of inflammation of the subcutaneous fatty tissue increases. If antiseptic rules are violated, acute local or general inflammation may develop. It happens that vaccines intended for oral administration are administered by injection. This threatens with pronounced local or general reactions.
- Diseases caused by vaccination. Such complications, most likely, would have developed in the baby later, regardless of the vaccination, caused by other factors. For example, a past infection.
These include: arthritis, thrombocytopenic purpura, autoimmune diseases, immunodeficiency conditions. Separately, it is worth saying that in children with immunodeficiencies, the introduction of a vaccine can provoke the development of severe conditions: vaccine-associated poliomyelitis, BCG osteomyelitis, the development of a generalized BCG infection, vaccine-associated encephalitis, meningitis. However, all these complications are rare, even in children with immunodeficiencies. You need to understand that in this group of children, any infectious disease will have much more pronounced consequences than vaccination against them. Therefore, for children with immunodeficiencies, vaccinations are not completely canceled, but are carried out with caution, according to an individual calendar and taking into account the child’s condition.
Contraindications to the use of the vaccine
The medicine may be dangerous if the patient has the following problems.
- The patient cannot tolerate baker's yeast. In this case, he becomes ill after eating bread, buns and other rich foods.
- After the first injection, the patient’s temperature rises significantly, chills and severe weakness appear, and signs of a cold and intoxication may appear.
- Antibodies are not administered for viral and bacterial infections, including colds. In this case, the disease may reduce the effectiveness of treatment or provoke unwanted side effects.
- The vaccine is not administered for six months if the person being vaccinated has previously suffered from meningitis. In this case, you need to give the body time to recover so as not to provoke an allergic reaction.
The drug is never reintroduced after the patient has completed the full treatment regimen for 5 years. If you ignore this rule, you can significantly reduce immunity and cause multiple side effects, including the development of hepatitis B.
Tips and tricks
Despite the frightening list of possible adverse reactions and complications from vaccines, the main thing to remember is that severe consequences are extremely rare and they know how to deal with them, and local and general reactions are not so frequent, mild and not dangerous to health.
However, for several days or weeks after vaccination (how long depends on the specific vaccine), you should carefully monitor your child's well-being:
- High fever for 3 or more days, shortness of breath, convulsions, frequent vomiting, severe headache and other noticeable and persistent deviations from normal health are a reason to call a doctor.
- The administration of a vaccine is always an additional burden on the body, sometimes quite significant, so in the first days after vaccination you should rest more and avoid noticeable physical and emotional stress.
- When the temperature rises above 38°, antipyretic drugs are used in combination with physical methods - cold compresses, wiping with a damp sponge. It is especially important to reduce the temperature in children prone to seizures and with hypertensive-hydrocephalic syndrome.
- Carefully monitor the condition of the body if a vaccinated child, especially a child, has a high risk of allergic reactions.
- During the first 2 weeks before and after vaccination, it is better to avoid foods that are obligate allergens: seafood, honey and chocolate, eggs, strawberries, raspberries, citrus fruits.
- In the first 7-10 days, try to avoid contact with other people to reduce the risk of colds. This is especially true for people with reduced immunity and chronic diseases.
- It is recommended to do a general urine test 3 to 4 weeks after vaccination to identify possible kidney complications: this is especially important for children with diseases of the urinary organs. The analysis will also allow timely detection of deviations and take the necessary measures.