People often confuse the concepts of “stomach pain” and “abdominal pain,” although from a doctor’s point of view these are different areas and the reasons for the discomfort also vary greatly, as does the degree of danger to health and life.
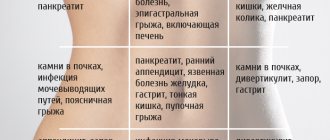
Stomach pain (sometimes referred to as discomfort in the pit of the stomach) is a sensation that is localized under the ribs, behind the sternum and upper abdomen, the so-called epigastric zone. Anything that hurts below this area, near the navel, on the sides and lower abdomen, does not apply to this complaint. In this case, they talk about pain in the abdomen or abdominal cavity.
Pain in the stomach occurs quite often, and it is typically associated with food intake. Pain may occur before eating (on an empty stomach), immediately after eating, or 2 to 3 hours later. Based on this description, the doctor may already suspect certain problems. If nausea, belching or heartburn occurs, this describes the condition even more accurately.
Often, if pain of this localization occurs, the problem is usually associated with the esophagus or stomach, the initial part of the vomit (duodenum or duodenum). In addition, pain in the stomach can simulate damage to the pancreas and gallbladder (but not the liver, which has no pain receptors).
The best pills for stomach pain
Of course, the first and completely justified desire of a person, if stomach pain occurs, is to take medications that will alleviate the condition. But this is not always acceptable and justified; in some cases, pain is a signal that immediate help is needed, including surgical help, and pills will only delay its receipt, causing complications.
Therefore, any sudden, acute, sharp pain with fever, cold sweat, loss of consciousness, pallor, nausea or vomiting (especially with blood) is a reason to immediately call an ambulance and hospitalization. It is important to exclude bleeding from an ulcer, gastric perforation, acute poisoning and other life-threatening conditions.
If you have been suffering from esophagitis, gastritis or peptic ulcers, duodenitis for a long time, then you are familiar with stomach pain. They usually occur after certain foods (sour, spicy or sweet foods), against the background of heartburn, overeating, stress or smoking. In this case, the cause may be muscle spasm, irritation of the mucous membrane of the esophagus or stomach, inflammation, circulatory disorders (ischemia). After a complete examination and diagnosis, the doctor may prescribe you pills for stomach pain. They will need to be taken either continuously, in courses, or as needed, against the background of exacerbation or pain.
Causes of stomach pain
Functional stomach disorders
The most common cause of stomach pain in young and middle-aged people. It occurs 2 times more often in men than in women. Characterized by unpleasant aching sensations in the epigastric area, which can turn into sharp pain. The pain syndrome is variable and appears periodically. Accompanied by belching, nausea, heartburn. Symptoms are provoked by eating spicy food, fast food, and dry food.
Intestinal infections
Stomach damage is more typical for food toxic infections and staphylococcal infections. A few hours after eating stale food, severe pain in the epigastric region, nausea and repeated vomiting begin. Symptoms are often associated with watery diarrhea. Pain throughout the abdomen, including in the stomach, occurs with salmonellosis and escherichiosis.
Gastritis
The nature of the pain depends on the type of inflammation. Intense pain on an empty stomach is specific for hyperacid gastritis. They resemble an attack of peptic ulcer, accompanied by heartburn and sour belching. With hypoacid gastritis, dull pain occurs after eating. It is aggravated by nausea, heaviness in the stomach, and loss of appetite.
Peptic ulcer
An ulcerative defect of the gastric mucosa is characterized by epigastric pain. With damage to the antrum and body of the stomach, pain is observed to the left of the center line of the body, and with a defect in the pylorus - to the right. Pain sensations often radiate to the shoulder blade, spine, or to the left side of the chest, simulating pain in the heart.
With a stomach ulcer, pain typically appears 30-60 minutes after eating. The higher the defect is localized, the earlier the pain is felt. When the duodenum is involved in the pathological process, “hungry” and night pains predominate. They decrease at the end of the meal. The patient's condition improves after vomiting and when a heating pad is applied to the stomach area.
With a complicated course of peptic ulcer disease, the nature of the symptoms changes. Perforation of the ulcer is indicated by severe “dagger” pain in the stomach, which sometimes causes fainting due to painful shock. If the perforation is accompanied by bleeding, the pain decreases. General symptoms are steadily increasing: protective tension of the abdominal muscles, severe weakness, pallor, and tachycardia are noted.
Pyloric stenosis
In the compensated stage of pyloric stenosis, a dull pain in the abdomen is observed, which worsens after eating. Typically, patients find relief from vomiting. Decompensation of the process is manifested by severity, expressed pain in the epigastrium. After each meal, vomiting begins; the vomit often contains foods eaten many hours ago. Patients quickly lose weight and complain of constant weakness and drowsiness.
Diaphragmatic hernia
With this disease, pain is most often localized behind the sternum, but can be located in the projection of the stomach. The pain is very intense, typically radiating to the interscapular area. The pain occurs after eating, physical activity, and when bending the body forward. Symptoms decrease after taking a deep breath and drinking water. The second specific symptom of a diaphragmatic hernia is dysphagia, which most often occurs when eating liquid or semi-liquid food.
Neoplasms
For benign gastric polyps, mild pain is typical, which is usually rare. Most people don't give them any importance. The clinical picture is complemented by discomfort after eating and belching. If the formation on the leg is infringed by the pylorus, acute cramping pain appears. At first they are localized in the epigastrium, then spread throughout the entire abdominal cavity.
Gastric cancer is characterized by constant moderate pain in the epigastric zone. Discomfort intensifies after finishing a meal. Heaviness in the abdomen, decreased appetite and weight loss are also observed. A pathognomonic symptom is a sudden change in taste preferences, an aversion to meat food. As the process progresses, the pain becomes very strong and cannot be relieved by standard analgesics.
Foreign bodies
Unpleasant sensations are caused by both swallowed objects (buttons, bone fragments, dentures) and stones formed in the body (gallstones, gastric bezoars). With a large foreign body, the patient experiences constant aching or dull pain in the stomach. Symptoms intensify after eating: a disturbing feeling of heaviness and fullness in the epigastrium.
Diseases of other digestive organs
Pain in the stomach area is often caused by diseases of adjacent organs - the liver and gallbladder, pancreas, and intestines. For cholecystitis, localization of pain in the epigastrium and right hypochondrium, nausea and vomiting after eating fatty foods are typical. With pancreatitis, girdle pain occurs in the upper abdomen, which usually radiates to the back.
Myocardial infarction
Pain in the epigastrium is felt with the abdominal form of a heart attack. A person complains of sudden, severe pain with frequent irradiation to the arm and left half of the body. The attack resembles an exacerbation of a peptic ulcer or pancreatitis. Nausea and reflex vomiting are observed. Stomach pain is aggravated by severe weakness and increased heart rate. The skin becomes covered with cold sweat.
Complications of pharmacotherapy
Most often, pain occurs due to uncontrolled use of anti-inflammatory drugs, leading to the development of NSAID gastropathy. It is characterized by moderate pain that occurs at night or on an empty stomach. The symptom is combined with heaviness in the abdomen, nausea, and flatulence. The pathology is dangerous because in 50% of people it is asymptomatic, and then can manifest as gastric bleeding. In addition to NSAIDs, stomach discomfort is provoked by glucocorticoids and antihypertensive drugs.
Rare causes
- Poisoning
: poisonous mushrooms and plants, pesticides, salts of heavy metals. - Motor dysfunction
: achalasia of the cardiac sphincter, cardia insufficiency, pylorospasm. - Abnormalities of the stomach
: Ménétrier's disease, congenital diverticula, complete duplication of the organ. - Neurological problems
: neurasthenia, masked depression.
Prevention
Paying attention to your health and following the following recommendations will help you avoid the feeling of heaviness in your stomach. So, preventive measures include:
Follow the recommendations and stay healthy.
Related services: Family doctor consultation Videogastroduodenoscopy
Diagnostics
At the initial appointment, the gastroenterologist collects complaints and anamnesis of the disease, conducts a physical examination of the digestive system: superficial and deep palpation of the abdomen, checking for peritoneal symptoms. The diagnostic search is aimed at finding out the causes of stomach pain. For this purpose, laboratory and instrumental diagnostic methods are prescribed:
- Ultrasound of the abdominal cavity.
Sonography is a screening study that detects gastrointestinal motility disorders and inflammatory changes in the stomach wall. The technique does not require special preparation and is carried out to make a preliminary diagnosis. - EFGDS.
Endoscopic examination of the mucous membrane of the esophagus, stomach, and duodenum is the most informative method. The doctor identifies erosions and ulcerative defects, signs of dysfunction of the gastric sphincters. If suspicious tumors are detected, a biopsy is performed for histological analysis of the material. - Radiography.
X-ray examination with barium allows you to visualize all parts of the gastrointestinal tract. Damage to the stomach is indicated by filling defects, “niche symptoms,” and deformation of the organ’s contours. To clarify the diagnosis, a CT scan of the abdominal cavity is necessary. - Intragastric pH-metry.
The level of stomach acidity is studied within 24 hours. According to this analysis, the functioning of the exocrine cells of the organ is determined and the type of gastritis is established. When pathology is detected, intraesophageal pH-metry and measurement of gastrin concentration in the blood are indicated. - Laboratory methods
. For stomach pain, the results of a coprogram are usually indicative, in which the level of lipids, undigested muscle fibers, and starch is assessed. A blood test is used to identify the inflammatory process. In chronic gastritis, megaloblastic anemia is often diagnosed.
Nota bene!
When a client asks for a remedy for abdominal pain, it is necessary to exclude urgent situations in order to send the sufferer to a doctor in time. These include:
- Severe pain that prevents you from sleeping or doing anything, lasts longer than 1-2 hours.
- Severe abdominal pain is accompanied by vomiting.
- Severe pain is accompanied by elevated body temperature - 38.5°C and above.
- Severe pain is accompanied by loss of consciousness.
- Severe abdominal pain in a pregnant woman.
- The abdominal muscles are tense and the stomach is as hard as a board.
- Diarrhea mixed with bright red blood.
- The stool is dark and tarry.
- Vomiting blood.
- Abdominal pain is accompanied by vomiting, diarrhea and severe dehydration.
Treatment
Help before diagnosis
For moderate stomach pain, non-drug treatment is indicated. To reduce the load on the digestive tract, fried, spicy, and fatty foods are excluded from the diet. To reduce irritation of the mucous membranes, you should avoid strong coffee, spices, and carbonated drinks. You need to eat small portions 5 times a day, chew each piece thoroughly.
In case of acute gastritis caused by poisoning, it is necessary to rinse the stomach as soon as possible. To bind and remove remaining toxins, sorbents based on activated carbon, silicon dioxide, and silica gel are used. If a person has very severe pain, vomiting with blood streaks, or tarry stools, you should immediately consult a doctor.
Conservative therapy
Most cases of pain in the stomach are associated with organic pathology, which requires individually selected etiotropic and pathogenetic therapy. In case of drug-induced lesions of the gastric mucosa, it is necessary to discontinue the drug causing unpleasant symptoms. For the treatment of the underlying disease and relief of symptoms, the following is prescribed:
- Antisecretory agents
. Proton pump inhibitors and histamine H2 receptor blockers are the main drugs for the treatment of hyperacidity. They inhibit the formation of hydrochloric acid and eliminate its irritating effect on the damaged mucous membrane. - Antacids
. The action of the medications is aimed at quickly neutralizing the acidity of gastric juice. They eliminate pain from gastritis and peptic ulcers. Non-absorbable antacids, which have a long-lasting effect, are preferred. - Antispasmodics
. Medicines quickly relieve pain by normalizing the tone of muscle fibers and sphincters. They are used as symptomatic therapy to relieve severe pain that is not eliminated by other drugs. - Prokinetics
. They are taken to eliminate pathological spasm or atony of the muscular lining of the stomach and its sphincter apparatus. They accelerate the movement of food through the gastrointestinal tract and stimulate active intestinal motility. - Enzymes
. Replacement therapy is recommended for concomitant diseases of other digestive organs. Pancreatic enzymes speed up the digestion of food and prevent the processes of fermentation and putrefaction in the intestines. - Gastroprotectors.
They protect the gastric wall from damaging influences and promote the regeneration of the mucous membrane. For this purpose, enveloping drugs, group E prostaglandins, are prescribed, which increase the level of protective factors in the stomach.
If pain in the stomach is not caused by gastrointestinal pathology, the patient is treated by doctors of relevant specialties - a cardiologist, a neurologist, a psychiatrist. Taking into account the disease, such patients are advised to take antianginal and antiarrhythmic drugs, sedatives, and antidepressants.
Therapeutic measures
Therapy is prescribed by a doctor after a comprehensive examination of the patient and is carried out under his strict supervision. During the treatment process, the specialist can make adjustments, taking into account the condition and individual characteristics of the patient. General recommendations in this matter are as follows: avoiding fatty and spicy foods, normalizing your diet and limiting alcoholic and carbonated drinks. You should eat fractionally and in small portions. Fast food and quick snacks on the go are not recommended. You should also pay attention to the psychological state. If you have difficulty breathing due to heaviness in your stomach, seek help from a specialist and under no circumstances self-medicate!
Where to go?
The doctors of the 5th Clinical Hospital have extensive experience in performing laparoscopic operations and hernioplasty in Minsk.
In addition to accepting patients who are citizens of Belarus, the 5th City Hospital of Minsk also accepts foreign citizens (on a paid basis). Each of them can undergo comprehensive diagnostics and treatment at the surgical and therapeutic departments.
The hospital has its own clinical diagnostic laboratory, X-ray department, X-ray CT and MRI rooms. The physiotherapy department has all the conditions for conducting rehabilitation programs.
M-anticholinergics
M-anticholinergics are one of the oldest groups of drugs.
Atropine has been used in medicinal herbs since the 4th century BC. e. Thus, the ancient Greek naturalist Theophrastus described mandrake as a remedy for treating wounds, gout and insomnia, and also as a “love potion.” The ancient Greek military physician Dioscorides (1st century AD) described mandrake wine as an anesthetic to treat pain or insomnia, to be given before surgery or cauterization. M-anticholinergics most effectively affect the upper gastrointestinal tract. The use of non-selective M-anticholinergics (atropine, platyphylline, metacin) is limited by their prescription, as well as by the fact that they have a systemic effect and have a number of side effects, such as intestinal atony and obstruction.
One of the relatively oldest selective M-anticholinergics is hyoscine butyl bromide (first registered in Germany in 1951). It acts on the M1 and M3 subtypes of receptors, localized mainly in the walls of the upper gastrointestinal tract, gallbladder and biliary ducts. Hyoscine butyl bromide does not penetrate the blood-brain barrier and has a weak systemic effect, unlike atropine. However, it is contraindicated in people with glaucoma, benign prostatic hyperplasia, as well as organic stenosis of the gastrointestinal tract and tachyarrhythmias. Hyoscine butyl bromide accumulates in the smooth muscles of the gastrointestinal tract and is excreted unchanged by the kidneys. The drug is successfully used for sphincter of Oddi dysfunction, biliary dyskinesia and pyloric spasm.
The severity of the effect of hyoscine butylbromide also depends on the patient’s individual sensitivity to this drug. Unfortunately, the antispasmodic effect of hyoscine butyl bromide on the small intestine (except the duodenum) and large intestine can be realized when taking a dose 2–10 times higher than the therapeutic dose, so its use is useless for spasms in the lower abdomen. A large number of restrictions and risks when taking this drug require medical supervision, which is why the M-anticholinergics known to us are currently used less and less abroad. However, hyoscine butyl bromide is still available without a prescription.
Cellular mechanism of pain
Smooth muscle cells are mainly found in the large intestine. There are significantly fewer of them in the small intestine. The mechanism of cell contraction depends on the concentration of calcium ions in the cytoplasm. The sources of calcium are the extracellular space, connected to the cytoplasm through calcium (slow) membrane channels, as well as the intracellular depot. The release of calcium causes the muscle cell to contract. The contraction of muscle cells forms a spasm and the person feels pain.
The process of muscle contraction is most often triggered by the mediator acetylcholine, binding to muscarinic cholinergic receptors (M-cholinergic receptors). Thus, blockade of M-cholinergic receptors leads to a decrease in tone and relaxation of smooth muscles (and therefore helps relieve abdominal pain). This, in particular, is the basis for the mechanism of action of a group of drugs called M-anticholinergics.
The interaction of calcium with calmodulin leads to the interaction of actin with myosin and cell contraction. CAMP (cyclic adenosine monophosphate) and cGMP (cyclic guanosine monophosphate) weaken the interaction of calcium with calmodulin and also impede the entry of calcium ions into the cell. The level of cAMP and cGMP is controlled by phosphodiesterase (PDE), which destroys excess of these nucleotides. Thus, if you reduce the activity of PDE, the concentration of calcium ions in the cytoplasm will decrease and the tone of the muscle cell will decrease.
Based on the described mechanisms for regulating the calcium concentration inside the muscle cell, which are disrupted under pathological conditions and lead to spasm, the main groups of antispasmodics have been created:
- M-anticholinergics (atropine, hyoscine butyl bromide).
- PDE IV inhibitors (drotaverine).
- Blockers of calcium release from intracellular stores or sodium channel blockers (mebeverine).
- Calcium channel blockers.