Causes of diarrhea
The most common causes of diarrhea include:
- bacterial infections (Escherichia coli, Shigella, Salmonella, Campylobacter, spread through contaminated food or water);
- viral infections (adenovirus, norovirus, rotavirus, coronavirus);
- parasitic infections (giardia, histolytic amoeba, cryptosporidium);
- inflammatory and functional bowel diseases (irritable bowel syndrome, Crohn's disease, ulcerative colitis, bacterial overgrowth syndrome);
- food allergies, food intolerance (lactose, fructose intolerance, celiac disease);
- diabetes mellitus (severe form, difficult to control);
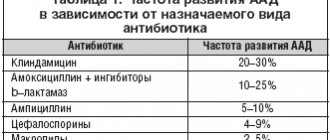
- side effect of taking medications (antibacterial and some anticancer drugs, antacids containing magnesium);
- consumption of low-quality, incompatible products, fatty and spicy foods, alcohol;
- surgical intervention (surgery on the stomach, intestines, gall bladder);
- intestinal ischemia;
- malignant neoplasms (pancreatic cancer, colon cancer);
- radiation therapy.
The most common cause of acute diarrhea in children is rotavirus infection.
Diarrhea in infants is most often associated with a viral infection (no treatment required), bacterial or parasitic infection. Diarrhea in young children can also be caused by changes in the diet of the child or mother (during breastfeeding), or the use of antibiotics by the child or mother (during breastfeeding).
Diarrhea and microflora of mucous membranes
Back to list Previous article Next article
06.04.2013
Tags:
diarrhea
5/5 — (2 votes)
At different periods of his life, every person has experienced an unpleasant condition associated with changes in intestinal function, stool disorders - diarrhea (diarrhea).
Stools become more frequent from 2-3 to 10 times a day, the urge to defecate appears, sometimes immediately after eating, and general well-being is disturbed. Often this occurs unexpectedly, disrupting the usual rhythm of life and health. Diarrhea is a syndrome that appears with a variety of dysfunctions of the digestive organs, both in acute diseases and in long-term disorders in the gastrointestinal tract.
If you know and remember about the factors and reasons that can provoke instability of the intestines and cause diarrhea, you can protect yourself from unforeseen conditions and maintain an active, healthy state of health every day.
Normally, the eaten food, in the form of a processed food bolus, moves further from the stomach through the intestines. Here food substances are broken down into easily digestible forms of proteins, fats, carbohydrates necessary for the cells of the body’s tissues. With the active participation of beneficial microflora of the intestinal mucosa, nutrients are processed and “transmitted” through the intestinal wall into the blood, where they are involved in all types of metabolism. Bacteria produce B vitamins and also regulate electrolyte and water metabolism. This supports osmotic and transport processes in the intestines. Metabolites of beneficial normal flora are involved in the synthesis of neurotransmitters, improve the conduction of nerve impulses and gastrointestinal motility.
For the daily effective functioning of the intestines, certain conditions are necessary:
1. Depending on the quantity and quality of food and water, there should be a sufficient amount of secretion of food juices and enzymes of the stomach, pancreas, small intestine, and bile secretion in the liver. Reactive enzymatic disorders can occur: with peptic ulcers, gastroduodenitis, cholecystitis, pancreatitis, enterocolitis, ulcerative colitis, celiac disease, lactase deficiency, food allergies, hepatitis, diabetes mellitus, cancer, and accompanying dysbacteriosis.
When the intestinal mucosa changes, the absorption of digested substances and the absorption of water from the food substrate deteriorate. Excessive flow of bile into the intestines after removal of the gallbladder can lead to irritation of the mucous membrane and impaired absorption of nutrients and water. “Under-oxidized large wastes” accumulated in the intestinal cavity change the state of the intestinal mucosa and can cause a “paradoxical” increase in peristalsis in different areas. For pathogenic bacteria, undigested food substances provide a rich nutrient medium. Pathogenic putrefactive flora, aggressively multiplying, releases its toxins and enhances fermentation, gas-forming processes, and flatulence. Osmotic disturbances cause the secretion of electrolytes and water, their flow from the blood into the intestinal cavity. The formation of feces and their liquefaction are disrupted. This will manifest itself as frequent, loose stools with undigested intestinal contents.
Drinking large volumes of liquid per day - teas, pure water, coffee, juices, and other liquids - can increase intestinal motility and frequent bowel movements. Excess of undigested fructose, lactose, vitamin C, magnesium can cause osmotic diarrhea. A lot of fatty, carbohydrate, fiber-rich foods will require more enzymes and food juices to break down and process them.
If you are not a supporter of separate meals, you like fatty, meat dishes, baked, rich delicacies, eat a lot of different fresh vegetables and fruits without thinking about their compatibility, then a violation of the frequency, character of stool, or diarrhea may remind you of intestinal overload. Diarrhea can be especially disturbing in cases of food excess, in diseases of the intestines, pancreas, liver, and periodically with the onset of functional disorders in these organs. You should think about fractional and separate meals, reasonable fluid intake and the compatibility of a variety of plant foods.
2. To promote the food substrate and cleanse the intestines, fairly active motility is needed throughout the gastrointestinal tract. This is accomplished by: regulation of intestinal motility by the nervous system, adequate vegetative reactions and preserved smooth muscle apparatus in the wall of the digestive organs. These reactions can worsen or be disrupted by: pathogenic toxins, various intoxications (viral, bacterial, alcoholic), metabolic changes, psycho-emotional overload, stress. You need to remove toxins from the body, and protect your nervous system from disturbing situations, overloads and give it positivity.
3. It is vitally important to preserve and function on the intestinal mucous membranes a biofilm from microcolonies of beneficial lactobifidobacteria and other normal flora, which can protect against pathogenic bacteria and their toxins, and actively participate in the processes of digestion, metabolism and immunity. To do this, it is advisable to conduct restorative courses 3-4 times a year with probiotics, prebiotics or functional nutrition with bacteria, helping your own microflora of the mucous membranes.
The development of diarrhea most often involves violations of all these mechanisms. But depending on the severity of the manifestations, they distinguish: infectious, secretory, osmotic, motor diarrhea.
You need to pay special attention to the first symptoms of increased frequency and relaxation of stool, and do not let the situation get worse. If diarrhea lasts more than 2 days, this is a serious disorder of the digestive system, which can lead to complications. Indeed, with prolonged or frequent diarrhea, the body loses vitamins, microelements, proteins, beneficial microflora, microcirculation, immunity, and metabolism are disrupted. All functions of the digestive organs become unstable, which can lead to inflammatory processes and structural changes in organs and tissues. The whole body suffers, not only the enzyme, but also the hormonal and nervous systems are disrupted.
Most often, diarrhea occurs with acute intestinal infections, intestinal dysbiosis and chronic diseases of the gastrointestinal tract. When diarrhea lasts from several days to two weeks, it is an acute course of intestinal dysfunction. If diarrhea persists for more than 2 weeks, it is a chronic disorder associated with severe disturbances in the structure of the digestive organs.
After ARVI, diarrhea is the most common reason for visiting a doctor or seeking medical help. The most severe course of diarrhea is observed in children of the first year of life and in the elderly, especially those who are often ill. In children, against the background of diarrhea, symptoms of dehydration and manifestations of inflammatory processes very quickly develop. This requires hospital treatment and medical supervision. Do not self-medicate in cases of acute or severe diarrhea.
Manifestations of diarrhea are associated with loss of fluid, electrolytes, intoxication: frequent urge to defecate, bloating, less commonly, cramps or pain in the mid-lower abdominal cavity, nausea or vomiting, lack of appetite, headaches, weakness, frequent, up to 5-10 times and looser or looser stools.
The appearance of watery or foul-smelling stools, with mucus or blood, more than 10 times a day, fever - requires an urgent call to the doctor and hospitalization.
Acute diarrhea can be caused by viruses: rotoviruses, noroviruses, herpes virus, viral hepatitis; and bacteria: campylobacteria, shigella, salmonella, lamblia, E. coli, with altered enzymatic function. When traveler's diarrhea develops, these microorganisms most often come from food or water, or through contact with patients or weakened immunity.
In children, the cause of an acute disorder and increased frequency of stools may be the aggressive reproduction in the intestines of Clostridium or Klebsiella, Proteus, Staphylococcus, in cases of insufficient quantities of protective lactobacilli and bifidobacteria on the mucous membranes. Against the background of dysbiosis in the intestines, harmful bacteria uncontrollably invade the mucous membranes, secrete their toxins, and disrupt the absorption of nutrients, water, and vitamins. This can also cause the development of an inflammatory process in the digestive system, intoxication, weakening of the baby’s immunity, and developmental delays. It is imperative to restore beneficial, protective lactobifidobacteria to the intestinal mucosa.
Diarrhea can become chronic in cases of untreated or undetected chronic diseases of the digestive system: colitis, hepatitis, pancreatitis, peptic ulcers, irritable bowel syndrome, celiac disease, which are almost always accompanied by dysbiotic disorders in the intestines.
Diarrhea can also be caused by some medications - primarily most antibiotics, an overdose of laxatives, especially osmotic, magnesium, or prebiotics, some antiarrhythmic, hypotensive and antacid drugs. Rarely, loose stools can also occur due to a lack of vitamins - B2, F, niacin.
When the first signs of diarrhea appear, you need to:
- Eliminate the cause that caused the disorder of stool and intestinal function. Stop the intake of food or liquid, medications, or contact with the patient, other factors that caused these disturbances in the intestines.
- Take measures to prevent the development of complications. Be sure to drink large amounts of liquid, 2-3 liters, but in small portions, 30-50 ml, every 30-45 minutes and after each bowel movement. Do not eat fatty or rough foods, foods and dishes that require active work of the stomach, liver, and intestines. You can, in the absence of nausea and vomiting, drink rice water or weak chicken broth. Decoctions of herbs - chamomile, St. John's wort, yarrow. Drink clean or still mineral water in small portions. Do not take antibiotics if there is no fever, signs of inflammation and without a doctor's prescription. In case of severe diarrhea, you can drink intestinal antiseptics - Intetrix, Ersefuril, Enterol, Bactisubtil, because under these conditions, pathogenic microflora begins to grow in any case. Taking antidiarrheal drugs – imodium, loperamide – is highly undesirable. If the cause of diarrhea is viruses or bacteria, then they are “locked” and are not removed from the intestines, and intoxication and diarrhea will increase. It is better to take liquid forms with bifidobacteria 3-4 times a day, 10-14 days.
- Restore water-electrolyte and vitamin metabolism in the body, the composition of beneficial microorganisms on the mucous membranes of the intestines. Use for severe loss of fluid, signs of intoxication - rehydron, enterodes, electrolyte - powders for the preparation of glucose-saline solutions. Be sure to take complex vitamins, preferably liquid forms, because fresh or canned juices can cause loose stools again. It is good to restore and improve the condition of blood vessels by drinking more compotes or fruit drinks with cranberries, currants, and chokeberries. Be sure to take proven and effective probiotic products, with live beneficial bacteria and their metabolic products.
For diarrhea, the synbiotic biocomplexes Normoflorins have confirmed their reliability, safety and effectiveness in restoring digestive processes, normalizing intestinal function, the state of vitamin-electrolyte, water metabolism and the composition of microflora on the intestinal mucosa.
Back to list Previous article Next article
When should you see a doctor for diarrhea?
You should consult a doctor if you have diarrhea lasting more than two days, fever up to 38.8˚C or more, frequent vomiting, six or more episodes of bowel dysfunction during the day, severe abdominal pain, blood or pus in the stool, tarry stools , symptoms of dehydration (extreme thirst, rare urination with a small volume of urine, dark urine color change, severe general weakness, lethargy, dry mouth, decreased blood pressure; crying without tears in babies, sunken eyes, fontanel). It is especially important for older people and people with weakened immune systems to get timely help.
The need to seek medical help for diarrhea can be clarified here.
Based on your individual situation, symptoms, general health, diagnostic results, the doctor will prescribe the necessary treatment. It may include means for rehydration, restoration of electrolyte balance; medications aimed at eliminating symptoms (enterosorbents, drugs for regulating intestinal motility) or the underlying disease causing diarrhea; treatment of infection (antibiotics, antiparasitic drugs); nutritional recommendations.
Partial protection against diarrhea caused by rotavirus infection in early childhood is provided by the appropriate vaccine. Methods to prevent traveler's diarrhea include hand washing, careful food selection, and using bottled or purified water for drinking, brushing teeth, and making ice.
Frequently asked questions about diarrhea
To create a menu, you can refer to the list below.
Monday
Breakfast: semolina porridge with half-and-half milk, biscuit crackers, tea drink.
Snack: a handful of blueberries with dry cookies.
Lunch: chicken broth with small pasta and small meatballs. Veal dumplings with a side dish of boiled rice. Cherry compote.
Afternoon snack: rosehip broth with a toasted (or in a toaster) piece of white bread with blueberry jam.
Dinner: half a boiled chicken breast with boiled buckwheat porridge, tomato salad, bird cherry and black currant drink.
At night: jelly.
Tuesday
Breakfast: omelette, 5 gr. butter. Cottage cheese with blueberry jam, green tea.
Snack: 1 pear without peel.
Lunch: rice cereal soup with pieces of vegetables. Fish cutlet cooked in a steamer, boiled rice. Kissel.
Afternoon snack: jelly from seasonal berries, dry cookies.
Dinner: non-dry cottage cheese casserole with cherry jam.
At night: mineral water without gases.
Wednesday
Breakfast: rice porridge on water with a piece of butter, black coffee on water, without milk and sugar.
Snack: baked apple with cottage cheese.
Lunch: pureed pumpkin soup with chicken and herbs. Mashed potatoes with a steamer cutlet. Unsweetened black tea. Yesterday's bread.
Afternoon snack: quince compote, crackers.
Dinner: stewed vegetables with beef meatballs.
For the night: fermented baked milk.
Thursday
Breakfast: soft-boiled egg. Sandwich on day-old bread with butter and mild cheese. The coffee is not strong.
Snack: 100 grams of seasonal or frozen berries.
Lunch: cereal soup. Vermicelli with chicken and vegetables. Diluted unsweetened juice. Yesterday's bread.
Afternoon snack: toast with marmalade, berry drink.
Dinner: stewed vegetables without fat with boiled fish.
At night: jelly.
Friday
Breakfast: oatmeal porridge with half-and-half milk (as tolerated) with small pieces of apple and pear without peel. Toast. Green tea.
Snack: cottage cheese with a small amount of fresh, non-sour sour cream.
Lunch: beef broth with meatballs and potatoes. Toast stuffed with boiled meat and a slice of tomato. Vegetable puree with steamed chicken cutlet. Strawberry compote.
Afternoon snack: jelly, toast.
Dinner: cauliflower with béchamel sauce. Drink of choice.
At night: baked apple.
Saturday
Breakfast: semolina porridge in water with a piece of butter, cocoa in diluted milk (as tolerated).
Snack: white omelette.
Lunch: fish soup with pieces of boiled white fish. Vegetable casserole with steamed quenelles. Bird cherry jelly. Yesterday's bread.
Afternoon snack: toast with jam, tea.
Dinner: spider web pasta with steamed cutlets, carrot salad with a teaspoon of sour cream.
For the night: fermented baked milk.
Sunday
Breakfast: scrambled eggs with a piece of butter. Toast with jam, tea.
Snack: cottage cheese casserole with fresh fruit.
Lunch: rice soup with chicken. Buckwheat with stewed rabbit. Tea, yesterday's bread.
Afternoon snack: toast with a piece of mild cheese, jelly.
Dinner: semolina pudding with jam sauce. Tea or jelly.
At night: fresh juice.