Causes of the disease
Kidney doubling occurs even in the intrauterine state of the embryo and is associated with the impact of teratogenic factors on the body and the transmission of pathology from parents at the gene level.
Teratogenic factors include the use of hormonal drugs during pregnancy by the expectant mother, ionizing radiation during the same period, vitamin deficiency and a lack of important mineral components and compounds necessary for the development of the fetus. All these factors disrupt the gene apparatus, the structure of chromosomes and the process of cell division, and directly lead to the development of such an anomaly as kidney duplication (right or left).
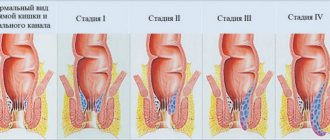
Kidney duplication is the most common developmental anomaly of the urinary system. With this anomaly, one of the kidneys is doubled. Such a kidney has dimensions significantly larger than normal, sometimes it is divided into lobules. Usually it is possible to distinguish the upper and lower buds, which are separated by a groove. The upper bud is almost always smaller than the lower one. Each kidney has its own renal artery. A complete doubling of the kidney is possible, when each of the kidneys has its own pelvis and, usually, the pelvis of the upper kidney is underdeveloped. Each kidney has its own ureter. The ureters run separately and each end at a separate opening in the bladder. Sometimes one of the ureters may empty into the other. Thus there are two separate buds. With incomplete doubling of the kidney, the pyelocaliceal system is one for the larger kidney.
Symptoms and course of the disease
The manifestations of this disease do not have any characteristic features. Incomplete duplication of the left or right kidney often does not produce any symptoms, and the patient lives his entire life without knowing about this anomaly. With complete doubling, the clinic is associated with insufficient emptying of the pelvis of the “underdeveloped” organ.
Complications with their inherent symptoms will be the following:
- inflammatory changes;
- reverse flow of urine from the ureters;
- hydronephrosis - retention and accumulation of urine in the pelvis.
For example, with complete doubling of the left kidney, the patient may feel pain in the lower back mainly on the left; Pasternatsky’s symptom will also be positive on the same side. In addition to pain, general symptoms appear (weakness, swelling, fever). A person may suffer from frequent renal colic, symptomatic increased blood pressure, and painful urination.
This anomaly in a healthy form does not pose any threat. But, more often than not, she is susceptible to various kidney diseases:
- Pyelonephritis (24% of all cases);
- Urolithiasis (21%);
- Hydronephrosis (14%);
- Tuberculosis (36%);
- Nephroptosis (3%);
- Kidney tumor (2%).
Thus, double kidney syndrome is a serious prerequisite for childhood diseases.
Treatment of the disease
Treatment of kidney duplication is required only in cases of the development of hydronephrosis, kidney tumors, and urolithiasis. Surgical treatment of kidney duplication is carried out in the presence of complications. It is aimed at correcting the cause of the complication. Various endoscopic and open surgical interventions are performed. They always try to save the kidney. A kidney is removed (nephrectomy) only if its function is almost completely lost. Sometimes a heminephrectomy is performed - removal of half or part of the kidney.
If a child has a double kidney and is in good health, conservative treatment is carried out aimed at preventing and relieving complications that arise, and regular monitoring by a specialist doctor of the condition of the kidney and the general health of the child is carried out.
In case of development of pyelonephritis against the background of kidney duplication, antibiotics are prescribed. With the development of an acute form of nephrolithiasis, treatment is aimed at dilating blood vessels by warming the kidneys and ureters and relieving spasms. A diet must be prescribed, which is based on foods that can destroy formed kidney stones.
Kidney duplication - what is it?
Modern medicine recognizes kidney duplication as a congenital pathology in which there is a complete or partial duplication of the renal system. The anomaly accounts for more than 10% of all defects of the urinary system, occurs in approximately 150 cases of post-mortem autopsy, and in newborns - in 1 case out of 140 children born. Unilateral doubling accounts for 88% of all registered pathologies, doubling of both kidneys accounts for 12%. The ICD-10 code is Q63.8 (Other congenital anomalies of the kidney).
When doubling, the kidney visually looks like two organs fused at the poles, each with its own blood supply.
The abnormal kidney, of course, is significantly larger than the normal one. The double kidney itself does not cause physical problems or serious impairment of the system’s function, but it contributes to the development of a number of diseases throughout life.
Diagnosis of the disease
Excretory urography helps diagnose kidney duplication, identify an increase in the size of the kidney, the third pelvis and ureter. However, the most difficult task is determining complete or incomplete doubling. The use of magnetic resonance urography and MSCT greatly simplifies this problem, but does not solve it completely. The presence of ureterocele is a factor that complicates the diagnosis of complete or incomplete renal duplication. Cystoscopy (finds the third orifice of the ureter instead of two) in the vast majority of cases helps establish the diagnosis.
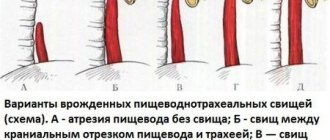
Kidney duplication does not manifest itself in any way and does not require treatment in itself. However, in an abnormally developed kidney, especially with complete doubling, some diseases often develop. Most often, urolithiasis occurs in one of the halves of a double kidney, hydronephrosis, and pyelonephritis. Sometimes complete doubling of the kidney is accompanied by ectopic ureter. In this case, the ureter does not flow into the bladder, but into another organ. The orifice of the ureter can empty into the rectum, cervix, vagina, or urethra. In this case, constant leakage of urine from the ureter is possible.
Introduction
Duplication of the kidneys and ureters is one of the most common congenital anomalies of the urinary tract, the proportion of which among all malformations is 0.8% [1]. Most double (duplex) renal systems do not require surgery. However, in the case of the addition of symptoms such as ureteral obstruction and the development of hydronephrosis, most often in the upper pole, which is associated with megaureter and ureterocele, as well as vesicorenal reflux (VRR), most often in the lower pole, or urinary incontinence due to ectopic upper polar ureter, surgical intervention becomes necessary. Children with double kidneys are subject to significant morbidity, including recurrent urinary infections that lead to loss of kidney function. Historically, maldeveloped and nonfunctioning renal fragments carry the risk of developing hypertension and malignancy [2, 3]. Some studies have described histopathological changes in distant segments, such as the formation of metaplastic islands or areas of nephroblastomatosis [4]. At the end of the 20th century, a conservative approach to the treatment of duplex kidneys was widespread, consisting of monitoring the abnormally developed kidney until pain or urinary infection appears [5, 6]. Another mini-aggressive strategy, which consists of restoring normal urodynamics by incision of the ureterocele or injection of gel, led to a decrease in dilatation of the nonfunctional fragment [7]. Some authors have provided data on the maturation of dysfunctional fragments after dissection of the ureterocele, which they confirmed by scanning the kidneys [8, 9]. However, these studies were based on approximate and imprecise calculations of areas of radiotracer accumulation in radionuclide scans of the kidneys, rather than on more accurate methods such as functional magnetic resonance imaging. There is still no reliable evidence of maturation of the dysplastic part of the duplicated kidney, since the function of the affected segment may remain stable or deteriorate, while the overall kidney function may improve due to the maturation of the intact part [10].
Surgical treatment for kidney duplication is recommended in case of disease with clinical manifestations. Currently, indications for partial nephrectomy include a non-functioning kidney fragment with recurrent urinary tract infections (UTIs), urinary incontinence due to ectopic ureter or VUR with the development of lower pole hydronephrosis [11]. Following the long-term dominance of the open approach for performing partial nephrectomy [12, 13], minimally invasive approaches have become increasingly common and are considered by some in this movement as the “gold standard” of treatment for this disease.
Alternative treatment methods, such as laparoscopic ligation of the upper pole ureter [14], pyeloureteral anastomosis and distal ureteroureterostomy [15, 16], have been well described previously, but require special conditions for their implementation, such as the absence of reflux into the lower segment of the kidney.
Types of minimally invasive surgeries.
Heminephrectomy (HNE) is the gold standard treatment for clinically manifested renal duplication. Other surgical interventions, such as ureteropyelostomy, ureteroureterostomy, require an elective approach and are unsafe for the healthy segment of the kidney.
Laparoscopic technology has recently become very widely used in urology and pediatric surgery. The first laparoscopic nephrectomy in an adult patient was performed in 1991 by R. Clayman [17]. In children, nephrectomy and nephroureterectomy were performed for the first time in 1993 [18]. In the same year, G. Jordan and B. Winslow [19] successfully performed the world's first laparoscopic GNE in a child. Laparoscopic GNE has made its way into the world of surgical techniques with great potential to improve postoperative recovery of patients and improve cosmetic characteristics, establishing the progress of pediatric endosurgery. Since the first report of laparoscopic HNE, the minimally invasive approach has become widespread and has replaced open surgery for the surgical treatment of patients with urinary tract anomalies in some large modern surgical centers [20]. The advantages and disadvantages of this method are regularly the subject of much debate. Undoubtedly, high costs, as well as a more complex technique compared to the classical open technique, are cited as disadvantages of laparoscopic GNE. Among the advantages of the method are a reduction in the period of hospital stay, a decrease in the duration of postoperative pain, a better cosmetic effect and a quick return to full physical activity of the child.
Another type of minimally invasive intervention designed to remove a segment of the kidney is represented by retroperitoneoscopy. The retroperitoneal approach has advantages that avoid mobilization of the colon, the risk of injury to internal organs and the formation of adhesions [21]. Problems with this approach include difficulty in reversing the kidneys (position of the vascular pedicle of the organ) compared to the transperitoneal approach and limited working space. The surgeon must also be alert to possible anatomical variations. In some cases, the polar vessels will be clearly visible, and in others they will be represented by short, scattered vessels extending from the main renal vessel [22]. M. Leclair et al. [23] published data on conversion to open surgery in 10 (21%) of 48 patients undergoing retroperitoneoscopic GNE. The authors reported difficulties in parenchymal dissection using bipolar diathermy at the beginning of the study, while these problems were resolved with the acquisition of a harmonic scalpel.
More modern minimally invasive treatment methods for kidney duplication are represented by robot-assisted and single-port surgery [24, 25]. Robotic HNE has demonstrated benefits such as increased mobility and dexterity with instruments inside the human body, less need for blood transfusion, shorter hospitalization, and reduced postoperative pain [26, 27]. Single-port surgery has also recently been implemented in pediatric practice [28, 29]. This technique has provided the ability to perform complex renal fragment removal using a single skin and fascial incision hidden in the umbilicus, providing the potential for superior cosmetic results. However, technical innovations related to the creation of technologically complex devices tend to promote the “surgical euphoria” of owning such innovations to a greater extent and do not allow for a focus on exploring the benefits of these newer methods.
In 2008, G. Lowe et al. [30] reported the use of new laparoscopic procedures designed to treat duplex renal anomalies. Procedures performed included pyeloureterostomy for incomplete duplication and lower ureteroureterostomy along with distal total ureterectomy for obstructive upper segment ureterocele. These procedures must be considered challenging in terms of technical execution as well as the absolute success of the operation in order to keep both segments of the renal duplex system functioning. Only a few studies [30, 31] have provided evidence that laparoscopic upper tract surgery can be successfully applied to a diverse range of procedures. There remains a relative lack of evidence in the literature regarding the safety and effectiveness of these procedures in children.
Technical features of minimally invasive operations.
Experience in minimally invasive surgery is always considered one of the most important factors in achieving successful results in laparoscopy. Laparoscopic HNE is a difficult procedure with a steep learning curve [23, 32, 33]. This operation is considered complex from a technical point of view and requires the use of special devices designed for ligation of renal vessels and dissection of its parenchyma, so it is relatively unpopular among pediatric surgeons and urologists [34].
However, the use of modern means of hemostasis (endoscopic clip applicators) and electroligation devices designed for resection of parenchymal tissues has made it possible to control bleeding and, consequently, laparoscopic resection has become more widely used among surgeons [34].
Vessel control was previously achieved by placing conventional sutures on the renal vascular pedicle. Modern methods of vascular ligation include the application of clips, the use of electroligation or a harmonic scalpel, or the use of currently available electroligation devices with a diameter of 3 mm, which provide the ability to seal the renal vessels in children with one hand without changing instruments [35].
The key point of the operation is clear identification of the renal blood supply to the upper and lower poles of the kidney. This identification must be made before the remaining normal portion of the kidney can be safely separated. Vascular control is required before dividing the parenchyma of the diseased and healthy parts of the kidney. After clipping the vessels, there is a clear demarcation of the tissue of the fragment intended for resection. It becomes recognizable due to the color change of the avascular tissues, which facilitates the determination of the correct plane of dissection of the renal parenchyma. Bloodless separation can be performed using bipolar electrocoagulation, electroligation, or a harmonic scalpel using ultrasound energy.
An alternative to electroligating devices is the endoloop method. It consists of placing a loop made of Vicryl Endoloop material around the kidney at the level of the vascular demarcation that has arisen after clipping or ligation of the feeding vessels [21]. After this, the renal parenchyma is divided with scissors. Any residual bleeding can be controlled using conventional mono- or bipolar coagulation.
Another important issue in the minimally invasive treatment of renal duplication concerns the method of processing the ureteral stump of the removed renal segment. In a study by M. Polok et al. [36] the ureteral stump was left open in 25 (75%) patients who had ureteral obstruction. In the remaining patients with VRR, the ureteral stump was sealed. Two (6%) patients required reoperation due to recurrent UTI resulting from reflux into the residual ureteral stump. R. Sydorak and D. Shaul [37] also reported this complication in 1 of 9 patients undergoing transperitoneal GNE. The authors emphasized that this complication could have been avoided if the entire ureter had been removed and ligated at the entrance to the bladder. The authors confirmed that removal of the entire ureter is necessary in every case where vesicoureteral reflux exists.
Comparison of minimally invasive treatment methods for kidney duplication.
Several studies have compared different surgical approaches to the treatment of nonfunctioning segments in the duplicated renal system. Currently, scientific papers compare at least predominantly two approaches to the treatment of kidney duplication; for example laparoscopy and open surgery or laparoscopy and retroperitoneoscopy. A. Golebiewski et al. [38] described their experience of laparoscopic treatment of 15 patients who underwent laparoscopic GNE and compared it with the results of treatment of 12 patients who underwent open GNE. This study found no statistically significant differences in operative time (mean time 148 minutes for laparoscopy, range 100–220 minutes vs. 124 minutes for open surgery, range 100–150 minutes). However, when using the open approach, the average length of hospital stay was shorter and the need for analgesia was greater than in patients in the laparoscopic group [38].
In another retrospective multicenter study, Q. Ballouhey et al. [39] compared the results of treatment of 15 patients who underwent robotic GNE and 13 patients who underwent open GNE. The average hospital stay in the open group was significantly longer than in the robotic group (6.3 days, range 5–8 days vs. 3.4 days, range 1–7 days; p
<0.001).
When comparing postoperative pain, total morphine consumption was significantly higher in the open group (0.52 mg/kg/day vs. 1.08 mg/kg/day; p
< 0.001). There were no significant differences in the duration of the operation, the incidence of complications or decline in renal function.
S. Esposito et al. [40] published data from an international multicenter European study analyzing the results of treatment of 102 children who underwent partial nephrectomy over a 5-year period using two different laparoscopic approaches—transperitoneal laparoscopic GNE (52 patients) and retroperitoneoscopic GNE (50). The overall complication rate was significantly higher after using the retroperitoneal approach (15 of 50, or 30%) than the laparoscopic approach (10 of 52, or 19%; p
=0.05).
The mean operative time (laparoscopy 166.2 minutes vs. retroperitoneoscopy 255 minutes; p
<0.001) as well as the mean length of hospital stay (laparoscopy 3.5 days vs. retroperitoneoscopy 4.1 days;
p
<0.001) were significantly shorter in the laparoscopic group. Postoperative loss of renal function was not recorded. The authors concluded that, compared with retroperitoneoscopic GNE, laparoscopic partial nephrectomy is a faster, safer procedure and technically easier to perform in children, mainly due to the larger abdominal working space. In addition, the ability to perform total or subtotal ureterectomy in case of reflux is also considered an advantage of laparoscopy and a disadvantage of retroperitoneoscopy.
M. Escolino et al. [41] also published the results of a comparison of transperitoneal and retroperitoneal approaches in the treatment of duplex kidneys. The authors found an increase in the duration of the operation when using a retroperitoneal approach (80 minutes versus 50 minutes). The remaining ureteral stump after standard laparoscopy (range 3–7 mm) was significantly shorter than after retroperitoneoscopy (range 2–5 cm). Despite these data, there is still no other evidence to show which approach, laparoscopic or retroperitoneoscopic, is advantageous for the patient. Nevertheless, literature data reflect a higher rate of conversions and complications of retroperitoneal access when performing retroperitoneoscopic partial GNE than when performing a laparoscopic procedure.
A. Neheman et al. [42] presented several advantages in favor of minimally invasive approaches (laparoscopy, retroperitoneoscopy and single-port surgery). Compared with open access, the use of all three endosurgical methods was accompanied by less blood loss during surgery and a shorter period of patient stay in the hospital. At the same time, the duration of surgery in the open intervention group was less than in the laparoscopy and retroperitoneoscopy group, but longer than in the single-port surgery group. For all other parameters, the advantages of one approach over the other have not been identified.
Single-port surgery assumes that all manipulations on the organs of the retroperitoneal space can be performed through one access located deep in the navel. This technique challenges classical multiport laparoscopy, but creates significant ergonomic difficulties such as interference of instruments from the outside, crowding (many instruments within one port) and most importantly, crossing of instruments [43, 44]. The latter means that all movements become unnatural, such as crossing your arms when playing the piano.
Despite the predominant cosmetic effect of the single-port approach, lively debate continues regarding the place of this method in the treatment of duplex kidneys. Y. Tam et al. [43] from Hong Kong found that single-port nephrectomy took longer than standard laparoscopy (mean 156 min vs. 99 min). However, S. Islam et al. [45] reported that when their costs were considered, single-port nephrectomy and HNE were less expensive than standard laparoscopy (GBP 942 versus UK£1127).
The safety and effectiveness of robotic surgery (RS) has been proven for various urological procedures in children, including pyeloplasty, orchidopexy, and nephrectomy [46]. The robotic system allows for fine and precise movements that are ideal for pediatric reconstructive surgery [46]. The disadvantages of the method in children are the large size of the instruments, loss of the feedback tactile sensation from working with tissues, and high operating costs [47, 48]. Most studies reporting robotic HNE compare their data with results from open surgery [49]. However, this comparison appears to be unfair because the surgical “competitor” in terms of access, tissue trauma, and cosmesis are other minimally invasive techniques such as conventional laparoscopy or single-port laparoscopy. Such comparisons are certainly limited. R. Malik et al. [49] compared the results of open surgery, standard laparoscopy and LC and found that the robot provided comparable results in terms of postoperative complications and preservation of renal remnant function. Two other studies compared standard laparoscopy, single-port surgery, and LC for nephrectomy in children. Both studies confirmed a longer operative time with the use of RS, while no other differences in postoperative analgesia and length of hospital stay were identified [29, 48].
H. Till et al. [50] presented a meta-analysis of studies examining all three current minimally invasive methods of GNE—standard laparoscopy, single-port laparoscopy, and R.H. Although a single laparoscopic approach and robot offer clear advantages at first glance, it has been found that technologies should be selected according to the age of the patient. This study provides a comprehensive review of the literature to answer an important question for parents: Which kidney fragment removal procedure is best for the child?
There are serious concerns regarding the use of minimally invasive treatment technologies for renal duplication in newborns and children of the 1st year of life. S. Dingemann et al. [51] compared two age groups of patients younger (group 1) or older (group 2) 12 months of life who underwent laparoscopic GNE. The authors found an increase in the duration of the operation in group 2 (average time 197 minutes versus 152 minutes) and found the formation of urinoma in 1 patient from group 1. The authors concluded that laparoscopic transperitoneal GNE is safe and feasible even in young children. The long-term results of these surgeries were also excellent regardless of the patient's age at the time of surgery.
Laparoscopic GNE is a technically complex procedure that requires staff training to master [23, 32, 33]. Both the incidence of postoperative complications and the duration of the operation depend on the quality of training. The results of laparoscopic HNE have been found to be associated with a learning curve [36]. All complications in the series of cases presented by the authors (33 operations) occurred during the first 16 operations. With increasing experience, the duration of the operation has also decreased. Another study confirmed that the time required to perform the operation also depends on the experience of the surgeon. According to M. Polok et al. [36], the average duration of the operation was 137 minutes. With increasing experience, this figure decreased significantly - from 140 to 125 minutes.
In existing reports, the duration of GNE from transperitoneal access ranges from 167 to 190 minutes [33, 52–54]. At the same time, the duration of robot-assisted GNE using the da Vinci robot increased compared to the duration of laparoscopic surgery [22]. The average duration of the operation was much longer than in the mentioned laparoscopic series, reaching an average of 275 minutes.
Analysis of postoperative pain relief has demonstrated clear advantages of all minimally invasive technologies over open operations that are used to treat renal anomalies. The open approach has been shown to be associated with an increased need for narcotic and nonsteroidal anti-inflammatory drugs. A non-narcotic regimen for postoperative analgesia in patients undergoing minimally invasive urological surgery has been previously described by Z. Lee et al. [55]. Their retrospective analysis presented 96 patients who underwent robotic pyeloplasty. Of these, 49 patients received intravenous doses of acetaminophen and ketorolac every 3 hours (group 1), 47 patients received nonsteroidal anti-inflammatory drugs in combination with narcotics (group 2). At the same time, the hospital stay of patients of group 1 was shorter than that of patients of group 2 (on average 1.0 days versus 2.0 days; p
<0.001). Therefore, it has been suggested that managing postoperative pain with nonsteroidal anti-inflammatory drugs is an effective regimen and may help reduce the length of hospital stay in patients with duplex kidneys.
The next important issue in surgical treatment for kidney duplication is the “fate” of the remaining kidney segment. In a multicenter review, G. Jayram et al. [56] reviewed the evolution of the remnant kidney after laparoscopic HNE and found that 4.9% of patients who were in the younger age group experienced a significant decline in function in the remnant kidney. The authors concluded that laparoscopy is associated with satisfactory results in children, but caution should be exercised when using laparoscopy in young children requiring GNE.
In another study by M. Leclair et al. [23] described, based on the results of radionuclide testing, a loss of function of more than 5% in 7 (24.13%) patients. The authors concluded that loss of function may occur as a result of inadvertent stretching and subsequent stenosis of the vascular pedicle of the remaining kidney. However, several studies have demonstrated that the function of the remaining part of the kidney was preserved in long-term follow-up [30, 31, 57].
Treatment for associated anomalies.
GNE of non-functioning parts in duplex renal systems in children requires a longer experience in order to correctly assess during the operation the blood supply to the kidney segments, the anatomy and type of ureters (obstructive or refluxing), as well as the pathology of the vesicoureteral junction (ureterocele or ectopic ureteral orifice). About 30% of all types of renal duplication are associated with ureteral obstruction and ectopia, ureterocele and VUR. During surgery, the pediatric urologist should be able to resolve all of these problems. Consequently, his experience and technical equipment must be adequate to solve these problems.
The debate about the ideal treatment approach for these cases continues. Depending on the malformations underlying this pathology, some authors suggest performing operations on the upper urinary tract [58-60], others on the lower urinary tract [7], others choose operations on the upper and lower sections, using both staged and one-step approaches [61]. Currently, most authors prefer to postpone the final reconstruction of combined malformations with renal duplication until the 2nd or 3rd year of the patient’s life [61]. However, performing surgery at a later age carries the risk of developing recurrent UTIs, kidney damage, and bladder dysfunction [62–64]. Therefore, surgical interventions for renal duplication are recommended to be performed at an early age, including in newborns [57]. Early surgical intervention can prevent the development of UTIs and therefore effectively prevent kidney scarring and subsequent loss of kidney function.
There is no consensus regarding the optimal treatment method for ureterocele. Based on the theory that the ureterocele need not be dissected and the enlarged ureteral stump will not cause problems once the renal segment is removed, some authors recommend HNE without intervention in the lower urinary tract [7]. There are other views, based on the experience of treating patients, showing that after GNE, repeated surgical interventions are often required in cases of ectopic ureter, ureterocele, obstructive megaureter or high-grade VUR [3, 62].
Few authors recommend endoscopic techniques as a definitive procedure for the correction of these conditions [65]. However, most surgeons consider endoscopic intervention as the first line of treatment for UTI to prevent urosepsis until definitive surgery is performed [65]. To restore the lower urinary tract in VUR, endoscopic methods gradually began to be replaced by open surgical approaches. The effectiveness of using Deflux gel injection varies from 70 to 90% after 1-3 endoscopic injections. Regarding double ureters, there are reports of a small number of patients who underwent endoplasty of the ureteral orifice. Some authors report comparable results when using the gel in duplex systems compared to single systems [66, 67], others demonstrate significantly lower success rates for such therapy - 15.3-63% when used in duplex systems [65].
The negative prognosis of the use of the gel in case of duplication of the kidneys and ureters is associated with a number of features inherent in these systems - grossly dilated massive ureteral orifices, their lateralization, the perpendicular course of the ureteric tunnels in the bladder wall, or the connection with other anomalies, such as ureterocele, neurogenic bladder [68].
Based on these findings, the current preferred surgical approach is a combination of laparoscopic GNE and a full open bladder procedure, given the unfavorable bladder anatomy that accompanies duplex systems [57]. In confirmation of this, V. Ellerkamp et al. [57] reported on 13 patients with duplex kidneys who underwent simultaneous ureteral neoimplantation using the open Politano-Leadbetter technique. When lower urinary tract reconstruction is required, single-stage surgery is an excellent option to permanently correct the complex abnormality.
Prices
| Disease | Approximate price, $ |
| Prices for examination and treatment for testicular cancer | 3 730 — 39 940 |
| Prices for vaporization of prostate adenoma with a “green laser” | 16 050 |
| Prices for diagnosis and treatment of impotence | 1 320 — 50 000 |
| Prices for diagnostics of the genitourinary system in men | 5 630 |
| Testicular cancer treatment prices | 15 410 |
| Prices for the treatment of urolithiasis | 11 760 — 16 180 |
| Bladder cancer treatment prices | 21 280 — 59 930 |
| Prices for diagnosing prostatitis | 2 720 |
| Prices for diagnosing male infertility | 6 300 |
| Prices for prostate cancer treatment | 23 490 — 66 010 |
| Disease | Approximate price, $ |
| Prices for kidney cancer treatment | 28 720 — 32 720 |
Causes
The pathology can be exclusively congenital; it begins during the period of intrauterine development of the fetus. Hereditary disposition is often important when one of the parents and close relatives has a similar anomaly. Also, a number of factors can have a pathogenic effect on the body of the mother and fetus, as a result of which a kidney with structural defects is formed during embryogenesis.
Among these factors are:
- Receiving radioactive and x-ray irradiation.
- Work in hazardous industries.
- Poisoning with drugs, poisons, intoxication.
- Taking drugs with teratogenic effects.
- Drug addiction, alcoholism.
- Severe vitamin deficiency.
The result of the action of such factors is the appearance of two foci of kidney growth, when 2 pyelocaliceal systems are formed. Their final separation does not happen, so the double kidney is covered with a common fibrous membrane. The vessels depart separately from the aorta, or have a common trunk, which is then divided into two parts and approaches each kidney individually. Sometimes the arteries inside the double kidney penetrate from one abnormal organ to another, which can create certain difficulties during surgery. In the video about what kidney doubling is like:
Treatment for double kidney
Treatment tactics for kidney duplication are determined individually. The patient is prescribed a course of medications or surgery.
Conservative
If a bifurcated kidney leads to complications, doctors prescribe appropriate therapy. A patient with pyelonephritis is prescribed a course of antimicrobial drugs (Furadonin, Amoxiclav) and general restoratives. When small stones are detected, drugs are prescribed that can dissolve them (Allopurinol, Prolit), as well as antispasmodics (No-shpa), analgesics (Ibuprofen, Ketanov). In addition to drug treatment, urologists and nephrologists advise taking kidney tea and other herbal remedies.
Surgical
The question of surgery becomes relevant when bifurcation of the kidneys - the cause of the accumulation of a large amount of fluid inside or a complication of the anomaly - does not respond to conservative therapy.
When choosing intervention tactics, specialists try to preserve the organ. But if its structures are significantly affected and cannot cope with their function, the question arises of removing the kidney.
Problems associated with extravesical ectopia can also be solved surgically. An open operation with complete reconstruction of the ureters is performed. As an alternative, use:
- electroincision - an endoscopic method allows you to normalize the normal outflow of urine from the upper sections of the excretory tract;
- ureterectomy - removal of the ureter extending from a non-functioning segment of the kidney;
- ureteroureterostomy – connection of the excretory canals into one;
- heminephrectomy – cutting off half of a doubled organ.
By what methods is it determined?
Today, along with other countries, we use ultrasound screening in the first year of life to determine kidney function, so developmental anomalies are detected quickly and early. Once kidney duplication is detected, a decision is made on the tactics of further observation or treatment. Usually, additional examinations are prescribed in the form of contrast-enhanced radiography, or MRI, urography and duplex scanning of the renal vessels to determine the renal vessels, and cystoscopy is also indicated.
It is equally important to carry out a number of tests that reflect the functioning of the kidneys and the presence of infection. These include clinical urine tests, smears from the urethral canal and urine culture, urine biochemistry. As the baby grows and develops, he is given examinations to assess kidney function over time or control studies to determine the effectiveness of treatment measures.
Forms of pathology
As already noted, the anomaly can be one-sided or two-sided.
But in medical practice, differentiating pathology into the following forms is also of great importance:
- Full doubling. Both the left and right kidneys have their own ureter, their own pyelocaliceal system. The pelvises are located parallel, connected only by a small isthmus of connective tissue. The calyx that is located at the top, as a rule, is underdeveloped, and the lower pelvis functions fully. Each of the doubled kidneys is, in fact, a separate organ.
- Incomplete doubling. With this anomaly, the parenchyma of the organ is double, its vessels are also doubled. The pyelocaliceal system develops without duplication. The top of the abnormal kidney is smaller than the bottom.
The most common occurrence is incomplete duplication of the left kidney. The right organ is affected much less frequently. The underdeveloped part of the double kidney resembles the state of the organ during dysplasia.
The photo shows the form of kidney doubling
The course of pregnancy with a bifurcated kidney
Women who know that they have this feature of the urinary organs need to prepare in advance for conception. It is worth consulting a nephrologist, checking your blood and urine in the laboratory to make sure there is no inflammation.
Typically, women carry their pregnancies normally and often do not even realize there is an anomaly in the structure of the kidney.
A contraindication for pregnancy is severe renal failure that develops against the background of doubling. Women whose anomaly was identified before conception are observed by a nephrologist for the entire 9 months. If any malfunctions occur in the urinary system, the pregnant woman is hospitalized.
Prevention
To prevent the defect, parents themselves should carry out prevention even before planning a child - this is a healthy lifestyle, playing sports and giving up bad habits.
If the defect has already been identified, the patient must follow certain rules that will prevent dangerous consequences due to kidney doubling:
- follow a diet that limits salt, spices, soda, alcohol and processed foods;
- avoid hypothermia - dress according to the season and use protective equipment;
- Visit your doctor regularly to prevent complications.
The program is adjusted by the doctor, depending on the patient’s condition. If you do not deviate from the recommendations, you can live a long and fulfilling life with a doubling kidney.
Kidney duplication can be asymptomatic for a long time and is detected accidentally during scanning of the lumbar region. Usually a bilateral process or complete doubling, in which one of the organs is underdeveloped and does not function sufficiently, causes inconvenience. In this case, drug therapy is prescribed, and in severe cases, surgery is performed.
Author: Denis Filin, doctor, especially for Nefrologiya.pro