Viral hepatitis B in adults is a serious infectious disease that can cause severe liver damage. Is it possible to cure this pathology? What does each of us need to know about hepatitis B?
A few numbers. In 90% of cases, hepatitis B is cured. But 10% of people remain carriers of the virus after treatment - their blood can be infected for months, years, and sometimes for life. Why the virus remains with them is not known for certain.
70% of carriers develop chronic persistent hepatitis B. They look healthy, the liver does not bother them, or it makes itself felt, but extremely rarely. The remaining 30% of carriers constantly suffer from liver disease. They may eventually develop cirrhosis and then, 30 to 40 years later, liver cancer.
There is currently no treatment for carriers. The risk of becoming a chronic carrier is inversely proportional to the age of the infected person. For example, infants become carriers in 90 - 95% of cases, while adults will become carriers in only 3 - 10%.
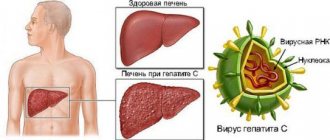
What is viral hepatitis B
Viral hepatitis is an infectious disease that primarily affects the liver.
The provocateur of this infection is the hepatitis B virus (HBV), which enters the body through blood, saliva or semen, and then travels through the bloodstream to the liver. The body has several defense mechanisms to fight disease. White blood cells, which protect the body from infections, attack and destroy infected liver cells. In addition, our immune system produces antibodies that circulate in the blood to destroy the virus and protect against subsequent infection.
The incubation period (the time between initial exposure to the virus and the onset of illness) for hepatitis B ranges from 60 to 150 days. Symptoms appear on average 90 days after infection.
Diagnostics
If a person has identified symptoms indicating that he has developed hepatitis B, or he has reason to believe that he could be infected with this disease, he urgently needs to visit a medical facility. During the appointment, the specialist will conduct an examination, examine the liver area using palpation and collect an anamnesis of the disease.
confirm or refute the primary diagnosis.
To diagnose this disease, in addition to the usual biochemical analysis for bilirubin and ALT, specific markers of hepatitis B are used:
- HBsAg antigen;
- HBeAG antigen.
In addition, specific diagnostics use the detection of antibodies to these antigens and to the specific HBcore protein, which appears in acute hepatitis B:
- anti-HBcore;
- anti-HBe.
Routes of transmission of viral hepatitis B in adults
Blood is the main source of hepatitis B virus. It can also be found in other tissues and body fluids, but in lower concentrations.
The hepatitis B virus can be transmitted in several ways.
Through blood.
This may happen in the following cases:
- punctures of the skin with infected needles, lancets, scalpels or other sharp objects;
- direct contact with open sores of an infected person;
- splashes of infected blood on the skin with minor scratches, abrasions, burns or even minor rashes;
- splashes of blood on the mucous membranes of the mouth, nose or eyes;
- using other people's toothbrushes or razors.
Contact with surfaces contaminated with blood can also cause illness, but to a lesser extent.
By the way, the virus can remain stable in dried blood for up to 7 days at 25 °C.
Hand contact with blood-contaminated surfaces such as laboratory benches, test tubes, or laboratory instruments can transmit the virus to the skin or mucous membranes.
Through saliva.
The saliva of people with hepatitis B may contain the virus, but in very low concentrations compared to blood. Nevertheless, infection is possible, for example, through bites.
But it is impossible to become infected through dishes or mouthpieces (smoking or musical instruments) - such cases have not been registered.
Through semen or vaginal secretions.
Hepatitis B is found in semen and vaginal secretions. The virus can be transmitted during unprotected sex and from mother to child during childbirth.
Feces, nasal discharge, sputum, sweat, tears, urine, and vomit do not spread hepatitis B. Unless they are contaminated with blood, the risk of contracting hepatitis B from these fluids is very low.
Synovial fluid (lubricant for joints), amniotic fluid, cerebrospinal fluid, and peritoneal fluid (found in the abdomen) may contain hepatitis B virus, but the risk of transmission is unknown.
Hepatitis B is not spread by sneezing, coughing, shaking hands, hugging, kissing, breastfeeding, or sharing cutlery, water, or food.
Hepatocellular carcinoma (HCC)
Hepatocellular carcinoma is a malignant and the most common primary liver tumor (more than 90%). Its origin is undoubtedly connected with:
- hepatitis B or hepatitis C;
- aflatoxin;
- cirrhosis;
- additional risk factors are smoking, obesity and alcohol consumption.
HCC may form a solid mass, multiple nodules, or diffusely invade the liver tissue. It is white-yellow in color and often contains bleeding and necrotic areas.
It metastasizes most often through the lymphogenous route to regional lymph nodes and gives hematogenous metastases most often to the lungs and other organs: adrenal glands, stomach, heart, pancreas, spleen, ovaries, bones.
It is the sixth most common cancer in the world, with 90% of cases in the Western world directly related to chronic liver disease or cirrhosis.
Symptoms of viral hepatitis B in adults
The main symptoms of hepatitis B include:
- dark urine;
- clay-colored stool (gray-white);
- jaundice;
- heat;
- joint pain;
- abdominal pain;
- fatigue;
- lack of appetite;
- nausea, vomiting.
Symptoms may vary depending on the person's age.
Many people may not show symptoms (asymptomatic disease). A very small proportion of patients develop a critical form of the disease called fulminant hepatitis B. This condition occurs as a result of a sudden loss of liver function.
Modern methods of treatment
Currently, there is no specific treatment for patients with acute hepatitis B. The acute infection is usually short-lived and often goes away on its own, due to the immune system.
Your doctor may recommend rest and proper nutrition and fluids to help your body fight the infection. Hospitalization may be required for patients who experience severe vomiting and are unable to maintain adequate nutritional levels. This may also be necessary to prevent the development of complications.
Although a chronic infection cannot be cured, there are two standard treatments that will help control the virus and prevent further liver damage:
- liver transplantation – this may be recommended in cases where the liver is seriously damaged;
- antiviral drugs, for example, Interferon - this is prescribed for a short period of time to suppress the virus.
“Antiviral therapy for chronic hepatitis B is carried out if there are certain indications,” says infectious disease specialist, hepatologist Tatyana Kovaleva.
– The specialist assesses the level of viral load, changes in liver enzymes, the degree of liver damage based on the results of ultrasound examination (ultrasound) of the abdominal organs and liver elastography (fibroscan) and then makes a decision. If antiviral therapy is prescribed, it is carried out over a long period of time, and in some cases permanently. Modern antiviral drugs lead to remission of the disease, prevent the progression of liver damage and the development of deaths. “Despite the successes of modern therapy, it is currently impossible to completely eliminate the hepatitis B virus from liver cells, since the DNA of the virus can integrate into the genetic apparatus of liver cells,” continues Dr. Tatyana Kovaleva. “Therefore, even with complete clinical recovery and the absence of the hepatitis B virus in the blood, it remains in the liver cells for life. With a pronounced decrease in immunity (use of immunosuppressive therapy, hormones, cytostatics, etc.), the hepatitis B virus can become active, which will require the re-prescription of antiviral therapy.
Treatment information
In 90% of cases, acute hepatitis B is treatable. The patient's recovery occurs 1-6 months after the start of therapy. The prognosis improves markedly when symptoms of the disease are detected at an early stage. Diagnosis and treatment of all forms of viral hepatitis B is carried out by a hepatologist or infectious disease specialist. In a chronic course, the prognosis is poor, recovery is impossible, the patient will die in 6-10 years due to complications.
Diagnosis of hepatitis B is achieved by detecting specific virus antibodies in the serum and immunoglobulins to them in the blood. Using a PCR test, the DNA of the virus is isolated to assess activity. Serological tests ELISA and RIA are carried out.
Treatment of hepatitis B should be supervised by a specialist. Self-medication will not lead to good results. Therapy is based on several principles:
- detoxification of the body;
- support of vital functions;
- strengthening the immune system;
- diet;
- suppression of symptoms.
For mild hepatitis, a gentle diet is necessary. The patient should eat in small portions 5-6 times a day, stay in bed, getting up only for self-care. If the condition is moderate, detoxification drugs are administered by drip, hepatoprotectors are used to protect cells from destruction, and vitamins are used. In severe cases, treatment is provided in intensive care.
Prevention of viral hepatitis B in adults at home
The most reliable prevention is vaccination.
Since 2000, it has been administered to all children, starting at birth. And more recently, for adults too. Vaccines provide safe and reliable protection—tests show that 90 to 95% of vaccinations in healthy people result in resistance to hepatitis B. Hepatitis B vaccination is safe. Side effects are usually minor, most often soreness at the injection site.
A contraindication to vaccination is an allergy to any ingredients of the vaccine.
Who is at risk
- Those who are promiscuous and have a non-traditional sexual orientation. To minimize the chance of contracting hepatitis B, contraception should be used;
- Injecting drug addicts using poorly disinfected syringes;
- Infants born from sick mothers;
- Those undergoing hemodialysis, if medical specialists do not follow precautionary measures;
- Tourists vacationing in countries with unfavorable epidemiological conditions;
- Family members of a hepatitis patient who do not follow hygiene rules;
- Those working in the healthcare sector and in direct contact with infected people;
- Those serving sentences in penitentiary institutions.
People at risk need to know exactly how hepatitis B is transmitted. They should undergo regular testing for the presence of the virus, and if it is detected, begin treatment immediately. Remember: the result of the fight against this dangerous pathology depends on the timeliness and adequacy of therapy.
Popular questions and answers
Infectious disease specialist and hepatologist Tatyana Kovaleva answered our questions related to hepatitis B.
What complications can there be with viral hepatitis B?
Acute hepatitis B in some people occurs with the development of jaundice and may be accompanied by severe liver damage with the development of liver necrosis.
In most adults, acute hepatitis B is asymptomatic without any clinical manifestations and ends with self-recovery. Only in 5 - 10% of adult patients the disease becomes chronic and continues for many years. This condition is called “chronic carriage of the virus” or “chronic hepatitis B”.
Because infection with the hepatitis B virus is often not accompanied by the development of jaundice, many patients are unaware that they have this disease. Chronic hepatitis B is often diagnosed during routine examination, including during pregnancy. If chronic hepatitis B is detected in a pregnant woman, she can pass the infection to her child. Currently, it is recommended to monitor the level of viral load during pregnancy; if high levels are detected, the pregnant woman is prescribed preventive antiviral therapy. If the child has not been vaccinated after birth, the risk of contracting the hepatitis B virus from the mother can reach 90% or more. In childhood, the risk of the disease becoming chronic is 30 - 98%.
If chronic hepatitis B is detected, constant monitoring by a specialist is necessary.
Many people with chronic hepatitis B may not have any symptoms for a long period of time. However, after a few years without antiviral therapy, severe manifestations of hepatitis may develop - liver cirrhosis or liver cancer (hepatocellular carcinoma). Weight loss, increased fatigue, and yellowing of the skin and sclera may indicate progression of the disease.
When to call a doctor at home for viral hepatitis B?
If jaundice develops, sleep disturbances, deterioration in health, swelling in the legs or development of ascites (increase in the size of the abdomen), darkening of the urine, you must call a doctor at home. The doctor will assess the severity of the patient’s condition and the need for his hospitalization in an infectious diseases hospital.
Sources
- Hepatitis B. World Health Organization.
- J. Feld (Canada) and HLA Janssen (Canada/Netherlands). Hepatitis B. Global Practical Recommendations of the World Gastroenterological Organization. — February, 2015.
- Information page about the hepatitis B virus. State of Israel, Ministry of Health.
- Viral hepatitis B: symptoms, treatment, prevention. GBUZ "Specialized Clinical Infectious Diseases Hospital" of the Ministry of Health of KK.
- Hepatitis B. Wikipedia.
- Acute and chronic viral hepatitis in the practice of a local physician. State budgetary educational institution of higher professional education "Ivanovo State Medical Academy" of the Ministry of Health of the Russian Federation. — 2015.
- Order of the Ministry of Health of the Russian Federation dated March 21, 2014 N 125n “On approval of the national calendar of preventive vaccinations and the calendar of preventive vaccinations for epidemic indications” (with amendments and additions).