What is fecal incontinence?
Fecal incontinence (fecal or anal incontinence) is an impairment of the ability to retain and control the passage of gas and stool from the anus. The severity of the condition can vary from the inability to hold gas (moderate incontinence) to the inability to control the retention of liquid and dense stool (severe incontinence). Stool incontinence is a fairly common problem, but due to existing social prejudices, patients rarely consult a doctor about it and are embarrassed to talk about it.
Causes
A blockage in the intestines is common in chronic constipation. The causes of pathology can be:
- abuse of fatty foods, smoked meats;
- hemorrhoids, rectal fissures;
- deterioration of intestinal tone;
- excessive stress on the gastrointestinal tract, overeating;
- intestinal atony and other deformations;
- sedentary lifestyle;
- stones in the kidneys;
- typhoid fever;
- eating persimmons.
At risk are the elderly and the mentally ill. Most often, these individuals do not control the emptying process, simply forgetting about it. In this case, more and more new portions of feces are gradually formed in the intestine, which leads to their hardening.
What causes anal incontinence?
Causes of anal incontinence can be:
- Injury to a woman's perineum during childbirth;
- Injury to the muscles of the anal canal;
- Decreased tone of the perineal muscles;
There are many causes of fecal incontinence. The most common of these is trauma to the anal canal during vaginal delivery. Such injuries can cause rupture of the muscles located in the anal canal, as well as the nerves that provide innervation to these muscles. It is possible to recognize some types of damage immediately after childbirth, but there are some situations that may not be immediately noticed or paid attention to, but which can subsequently lead to incontinence many years later.
Surgeries on the anal canal and perineum or trauma to them can cause problems with holding stool. Some people, especially older people, may have a decrease in the tone of the anal muscles, which can increase with age. As a result, if at a young age there are only minor disturbances in holding stool, then over time they can develop into severe anal incontinence.
Diarrhea (diarrhea) may be accompanied by a sudden urge to defecate (empty the bowel), as well as leakage of loose stool. If you are concerned about bleeding from the anus along with anal incontinence, you should definitely consult a doctor. These symptoms may be signs of inflammation of the colon (colitis), a tumor of the colon, or prolapse of the rectum (rectal prolapse), all of which require professional attention from a doctor.
Causes of encopresis
There are primary (congenital) and secondary (acquired) fecal incontinence. The primary form is of an organic nature, that is, it is caused by a lack of structural-muscular apparatus or innervation and control by the nervous system. The secondary form can also be organic (due to acquired disorders) or psychogenic, that is, caused by psychosocial reasons or stress.
The occurrence of encopresis is facilitated by physiological, neurological, mental and psychological disorders.
Psychological ones include:
- inability to obey social norms, conflict situations with peers or elders;
- insufficient formation of consciousness and control over one’s own behavior;
- lack of adequate toilet training;
- psychotrauma associated with forced potty training;
- stress;
- instability of the child’s emotional background.
Other factors contributing to the occurrence of encopresis:
- pathological birth (asphyxia, birth trauma, hypoxia) or threatened miscarriage, resulting in neurological disorders;
- gastroenterological disorders (tight compression of feces and intestinal overflow, disturbance of intestinal anatomy, its motility, etc.);
- traumatic injuries;
- intestinal infections;
- fractures of the spine, pelvic bones and traumatic brain injuries;
- mental illnesses (childhood schizophrenia, mental retardation, paranoid syndrome, autism spectrum disorder, catotonic syndrome, childhood depression, etc.).
For adults, somatic disorders are the most common causes, but uncontrolled bowel movements can also occur due to serious mental illnesses (schizophrenia, dementia). Depending on the cause of the disease, as well as the age of the patient, appropriate treatment is prescribed. Before making a diagnosis, it is necessary to undergo a series of examinations and confirm the symptoms.
How to determine the cause of anal incontinence?
At your initial appointment, a coloproctologist will help determine the severity of anal fecal incontinence and its impact on your lifestyle. By ascertaining a patient's life history, many clues may be revealed that point to the cause of the disease. For example, when examining a female patient, it is necessary to know the birth history. Multiple pregnancies, large fetuses, the use of forceps or episiotomy can cause muscle and nerve damage during childbirth. In some cases, an underlying chronic disease or chronic use of certain medications may play a role in the development of fecal incontinence.
It is necessary to conduct an examination of the perineum and a digital examination of the anal canal and rectum. With such an examination, injury to the muscles of the anal canal can be immediately determined. In addition, ultrasound examination of the anal canal can be used to determine its structure and possible defects.
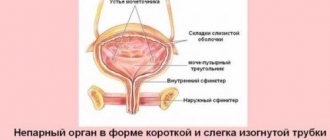
Often, additional research is necessary for a more complete and accurate study of the structure and functioning of the anal canal. During a test called anal manometry, a thin catheter is used to measure and record the relaxation and contraction of the muscles of the anal canal. This method determines how weak or strong these muscles are. Another test can determine the proper function of the nerves innervating the anal muscles.
What can be done to treat anal incontinence?
The following treatments for anal incontinence may be used:
- Diet correction;
- medicines to harden stool;
- exercises to strengthen the muscles of the anus;
- Biofeedback therapy (exercises with biological feedback);
- Surgical correction of anal muscle defects;
- Artificial anal sphincter;
After a thorough history, examination and examination of the patient, aimed at determining the cause and severity of the problem, it is possible to determine a treatment method or methods. To combat mild incontinence, it is enough to adjust the diet and use medications that fix the stool. Some diseases that cause inflammation of the colon (colitis) can also affect your ability to hold stool. Treatment for these conditions may help eliminate or improve symptoms of fecal incontinence. Changing medications in some cases improves the patient's condition. For moderate anal fecal incontinence, your coloproctologist can recommend a set of simple exercises to strengthen the muscles of the anus, which can be performed at home. It is possible to use the method of training the muscles of the anal canal with biological feedback (biofidek therapy). Such exercises help patients better feel the urge to defecate and strengthen the muscles of the anus.
Traumatic defects of the anal canal muscles can be corrected using surgical methods. For some patients, it will be optimal to use electrical stimulators of the skin and muscles of the perineum, which strengthen this area and help improve holding function.
In a group of patients with damage to the nerves and muscles of the anus, implantation of an artificial anal sphincter is possible. This is a special device that consists of a plastic ring filled with liquid. It is placed around the damaged muscles of the anal canal. When the ring is filled with fluid, the anal canal is closed. To empty the bowel, it is necessary to pump out fluid from the artificial sphincter ring.
In severe cases of anal incontinence, the best option would be to form a colostomy, which significantly improves the patient’s quality of life.
Fecal incontinence in adults - symptoms and treatment
Regardless of the severity and cause of incontinence, treatment usually begins with simple conservative measures.
Diet and exercise
Proper nutrition, taking fiber and drugs that slow down peristalsis help about half of patients. It is also recommended to avoid soda and foods that increase gas formation and peristalsis: mucous porridges, dairy products, fresh vegetables and fruits. The diet should be dominated by foods that fix intestinal contents: rice, bananas, etc.
For minor injuries to the pelvic muscles (for example, for second-degree perineal ruptures during childbirth), special exercises will be useful.
Drug treatment
For incontinence, drugs for diarrhea are prescribed: Loperamide or Diphenoxylate with Atropine. According to some studies, antidepressants, such as Amitriptyline, are effective in treating the disease. However, the mechanism of their action is not fully understood, so these drugs are used as a last resort if other means have not helped [9].
Biofeedback
Biofeedback therapy is a daily exercise that helps strengthen the muscles of the pelvic floor and abdominal wall, as well as increase the compression of the anal sphincter. During it, a special dilating balloon is inserted into the anal canal and within two seconds the patient compresses the sphincter as much as possible. At least 10 sessions are necessary, but if the symptoms do not decrease, therapy is stopped.
This method is ineffective for severe fecal incontinence, damage to the pudendal nerve and diseases of the nervous system.
Perianal injection therapy
10–20% of the intestinal contents are retained by hemorrhoids, so fecal incontinence often occurs after their removal and operations to treat fistulas and anal fissures [14].
In such cases, intraanal injection therapy can be used - a gentle method in which gel-like substances or fillers (Solesta, Permacol, Durasphere) are injected into the thickness of the anal canal. They compensate for the lost function of hemorrhoids: they create elastic submucosal “cushions” that help the walls of the anal canal to close hermetically during muscle contraction. These “cushions” can be compared to the rubber gaskets on sliding doors, thanks to which the doors fit snugly against each other.
Radiofrequency ablation
Another method of treating incontinence is radiofrequency ablation, or SECCA procedure. It helps strengthen the muscle layer of the anal sphincter by thickening collagen, the elastic scar tissue. The tip of the device is inserted into the thickness of the internal anal sphincter and heated to 85 °C. To avoid overheating of tissues, the instrument is cooled with a constant flow of water. The procedure is usually performed in the operating room under intravenous anesthesia [9].
Sphincteroplasty
If drug treatment and other minimally invasive methods do not help, then surgery is recommended.
If the muscles of the anal canal are damaged, sphincteroplasty can be performed - surgical restoration of the damaged muscle under spinal anesthesia [11]. It is indicated only for large ruptures of the anal sphincter, for example after difficult childbirth, severe operations in the anorectal area or pelvic injuries.
To prevent infection from developing, antibiotics are used an hour before sphincteroplasty. After the operation, defecation is held back for several days and the perineal wound is examined daily. An anti-diarrhea medicine can help control bowel movements.
On the first day after surgery, the patient can walk and sit freely, and take any food that does not cause diarrhea.
Complications of sphincteroplasty are rare and not life-threatening. The most common of these is infection of postoperative wounds, which can be resolved by removing superficial sutures and prescribing antibiotics [7]. Properly performed plastic surgery is effective in 80–90% of cases [14].
If the sphincter ruptures during childbirth, surgery with layer-by-layer restoration of the perineum may be required. If the plastic surgery was not performed immediately, then it can only be done six months later: 12–24 hours after the injury, the tissues inevitably become inflamed, and operations under such conditions are almost always unsuccessful.
For several weeks after sphincteroplasty, it is recommended to take short, cool sitz baths 3-4 times a day. In addition, it is important to learn not to strain during bowel movements.
Basic rules will help make it easier:
- eat more foods rich in fiber - they should make up at least half of a healthy person’s diet;
- drink at least 1.5–2 liters of fluid per day;
- sit on the toilet correctly, use a footrest;
- if defecation is impossible without straining, use microenemas or laxatives.
To improve the functioning of the pelvic floor muscles, it is recommended to perform special exercises after surgery. Your doctor will tell you more about them.
Sacral nerve stimulation
It is used if fecal incontinence occurs due to minor damage or degenerative changes in the anal sphincter and weakened pelvic floor muscles.
The procedure is performed under local anesthesia on an outpatient basis. Fine electrodes are inserted into the foramina of the 3rd sacral vertebra (S3), which stimulate the nerves with a weak current. As a result, the sensitivity and function of the rectum and anal sphincter improves, and the tone of the pelvic floor muscles increases. On average, after stimulation, fecal incontinence is 50% less common [15].
The method only works with constant nerve stimulation, so the electrode is installed for life, changing the battery every 5–7 years. Before permanent placement of the electrode, a test period is carried out for 2-3 weeks to help evaluate the effectiveness of stimulation for a particular patient.
Sacral stimulation is a relatively safe procedure that rarely leads to complications. Possible unpleasant consequences include:
- pain in the implantation area;
- electrode displacement;
- addition of infection;
- bowel or urinary dysfunction;
- unwanted overstimulation, which leads to unpleasant trembling or twitching.
Typically, these problems can be easily corrected by changing the strength of the stimulation, but sometimes the device may have to be removed. If the patient later wants to remove the electrode, this does not require hospitalization.
Magnetic stimulation
Based on sacral stimulation, extracorporeal magnetic stimulation (EMS) has been developed, i.e. taking place outside the body. A method of stimulating the pudendal nerve with a magnetic field directly in the perineal area is also used.
For damaged organs and structures of the pelvis, it is recommended to combine sphincterolevatoplasty (suturing the pelvic floor and anal canal muscles torn due to injury) with subsequent lifelong stimulation of the sacral nerves.
Intestinal stoma
If all of the above methods do not help, then the doctor may suggest creating an intestinal stoma. It is required in approximately 5% of patients with fecal incontinence.
After having a stoma installed, a person is forced to get used to a new body image and use special hygiene products. However, modern colostomy bags are equipped with odor filters, are securely fixed to the skin, and do not need to be changed daily. Most ostomy patients report that their quality of life has improved as a result. A few months after the operation, they fully return to their usual activities and live the same way as other people [8][9].