Cholestatic hepatitis is a disease in the development of which the obstruction of bile flow, as well as the accumulation of its components in the liver, is of key importance. Clinically, the disease is manifested by itching, discomfort in the area of the right hypochondrium, intense jaundice, dyspepsia, enlarged liver and the appearance of xanthelasmas on the skin. In diagnosis, general clinical and biochemical blood tests with determination of liver tests, ultrasound of the liver and gallbladder, sonography of the pancreas, and MRI of the abdominal organs are of primary importance. Therapy is aimed at improving the outflow of bile and normalizing organ function.
General information
Cholestatic hepatitis is a fairly rare pathology, the pathogenesis of which is based on intrahepatic cholestasis with deterioration of the excretory function of cells and damage to the ducts. The frequency of detection of the disease does not exceed 10% among all chronic hepatitis. Cholestatic hepatitis mainly occurs in older people.
Despite its relatively low prevalence, the disease is difficult to treat due to the fact that it is not always possible to clearly establish its cause. Clinical gastroenterology studies the etiology and pathogenesis, as well as the development of new methods of treating cholestatic hepatitis.
Cholestatic hepatitis
Complications accompanying alcoholic hepatitis
Various complications often develop against the background of alcoholic hepatitis. The most common of them:
- Accumulation of fluid in the abdominal cavity. In some cases, ascites is not amenable to drug treatment. Then the patient's abdominal cavity is pierced and the fluid is removed. The puncture allows you to perform an analysis (the composition of the pumped out liquid is examined) and reduce the pressure exerted on the internal organs.
- Inflammation of the membranes lining the abdominal cavity from the inside and covering the internal organs (periodontitis).
- An increase in venous pressure, as a result of which the veins of the esophagus dilate and internal bleeding begins. Its symptoms are: vomiting mixed with blood, black stools, an increase in heart rate to one hundred beats per minute (the norm is sixty to eighty), a decrease in blood pressure to less than 100/60 mm Hg.
- Development of hepatorenal syndrome, manifestation of severe renal failure. Kidney functions are inhibited, and toxic substances accumulate in the blood.
- Confusion (decomposition products have a toxic effect on brain tissue, blood circulation is disrupted).
- The formation of hepatocellular carcinoma is a difficult to treat malignant liver tumor.
- Hepatopulmonary syndrome (the patient has a very low oxygen content in the blood due to impaired blood circulation in the lungs).
- Menstrual dysfunction in women (menstruation is completely absent, too heavy, scanty or irregular).
- Infertility (female and male).
- Hepatic gastropathy (a gastrointestinal disease that develops due to impaired blood circulation and changes in liver function).
- Hepatic colopathy (damage to the large intestine).
Causes
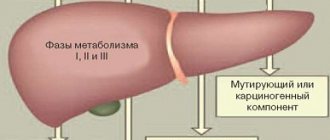
This pathology may be caused by intrahepatic or extrahepatic stagnation of bile. In the first case, disruption of the outflow of bile is possible both at the level of liver cells and at the level of intrahepatic ducts. The causes of intrahepatic cholestasis with subsequent development of hepatitis can be:
- transition of acute viral hepatitis B, C or other types into a chronic form;
- liver damage by Ebstein-Barr viruses, herpes, cytomegalovirus, mycoplasma infection;
- taking various drugs, such as aminazine, some diuretics, antibiotics, anabolic steroids, contraceptives;
- exposure to toxins, alcohol, poisons;
- endocrine diseases.
Extrahepatic cholestasis results from obstruction of large ducts. In this case, its possible causes are:
- blockage of the common bile duct by a stone;
- chronic calculous cholecystitis;
- chronic pancreatitis;
- cancer of the head of the pancreas and tumors of other organs of the hepatobiliary system.
Against the background of cholestasis in the liver, destruction of hepatocytes occurs with subsequent dysfunction of the organ. In some cases, it is not possible to establish the cause of the disease, which is interpreted as idiopathic cholestatic hepatitis.
Hepatitis: differential diagnosis
Of great importance is a carefully collected anamnesis, establishing the possibility of professional or household intoxication, taking into account the epidemiological situation in identifying the nature and cause of the disease. In unclear cases, the first consideration should be viral hepatitis. The detection of the so-called Australian antigen is characteristic of serum hepatitis B (it is also detected in virus carriers, rarely in other diseases). Mechanical (subhepatic) jaundice usually occurs acutely only when the common bile duct is blocked by a stone due to cholelithiasis. But in this case, the appearance of jaundice is preceded by an attack of biliary colic; bilirubin in the blood is mostly straight, stool is discolored. With hemolytic adrenal jaundice, free (indirect) bilirubin is detected in the blood, the stool is intensely colored, and the osmotic resistance of red blood cells is usually reduced. In the case of false jaundice (due to staining of the skin with carotene during prolonged and abundant consumption of oranges, carrots, and pumpkins), the sclera is usually not colored, and there is no hyperbilirubinemia.
Prevention of acute hepatitis, taking into account the diversity of their etiological factors, consists of strictly carrying out sanitary and epidemiological measures, observing the rules of personal hygiene, ensuring appropriate sanitary and technical supervision at enterprises, preventing the possibility of industrial poisoning with hepatotropic poisons. You should not eat mushrooms that are obviously inedible or unknown, as well as edible but old ones (which can also cause severe poisoning).
Symptoms of cholestatic hepatitis
The symptoms of cholestatic hepatitis are similar to those of other chronic liver diseases. Distinctive features are more pronounced jaundice and skin itching, which is often the first manifestation of the disease. Itching in this case is caused by the entry of bile acids into the blood due to stagnation of bile in the liver. Also, patients with cholestatic hepatitis often develop xanthomas, which look like yellow spots.
The color of the stool, as a rule, becomes lighter, and the urine darkens. Palpation reveals an increase in size and increased density of the liver without splenomegaly. During an exacerbation, an increase in temperature and mild symptoms of intoxication are possible. The severity of the clinical picture depends on the severity of cholestasis.
Alcoholic hepatitis – contagious or not?
Since alcoholic hepatitis is a toxic disease, it is not transmitted from person to person, as happens, for example, with viral hepatitis C. Moreover, women are more at risk than men - their bodies produce fewer enzymes that eliminate alcohol. Also at risk for alcoholic toxic hepatitis are:
- obese people;
- people who are underweight;
- patients with viral hepatitis;
- patients diagnosed with liver disease;
- patients who are forced to take medications that have a negative effect on the liver;
- regularly drinking alcoholic beverages.
Diagnostics
Laboratory and instrumental research methods play an important role in diagnosing the disease. Of the laboratory techniques, the main one for diagnosing cholestasis is a biochemical blood test.
- Liver tests. A biochemical study reveals an increase in the level of bilirubin due to the direct fraction, an increase in the level of transaminases, alkaline phosphatase (more than 5 times), gamma-glutamine transferase and cholesterol. You can also determine an increased amount of phospholipids, B-lipoproteins and bile acids in the blood.
- Serological and PCR diagnostics. To confirm the viral etiology of the disease, specific markers are studied using ELISA and PCR methods. A characteristic serological marker of intrahepatic cholestasis is the determination of antimitochondrial antibodies.
Among the instrumental methods used are echographic, X-ray, magnetic resonance, and invasive diagnostics:
- Ultrasound of the liver and gallbladder. Ultrasound examination reveals signs of chronic hepatitis. Ultrasound of the biliary tract, gallbladder and pancreas can confirm or exclude extrahepatic cholestasis.
- Radiography. If there are difficulties in diagnosing cholestasis, retrograde cholangiopancreatography, percutaneous transhepatic cholangiography or cholecystography is performed, which can detect stones in the bile ducts in cases where they are not visible on ultrasound.
- MRI. Modern non-invasive methods for identifying the causes of cholestatic hepatitis are MR-pancreatocholangiography and MRI of the hepatobiliary zone.
- Biopsy with histology. To study morphological changes, a puncture biopsy of the liver can be performed, although it does not play a decisive role in the diagnosis of cholestasis.
Diet
The energy value of food consumed for alcoholic hepatitis should not be lower than 2000 calories. The optimal amount of protein is determined at the rate of 1 g per 1 kg of body weight (not less). The role of amino acids in the treatment of hepatitis is explained by the fact that when their ratio in the body is normalized, protein catabolism in the muscles and liver decreases, and metabolic processes in the brain improve.
Additionally, the patient should take vitamin preparations and macroelements. Zinc is especially important. It reduces the level of alcohol dehydrogenase, an enzyme that breaks down alcohol, which increases the risk of liver toxicity.
The patient's daily diet should include:
- dairy products (a lot of protein is found in cheese, cottage cheese, kefir);
- lean meat;
- any types of fish;
- legumes
Prohibited:
- fried, salted, spicy, smoked, fatty;
- coffee, carbonated drinks, cocoa, alcohol.
Food should be consumed frequently and in small portions.
Drug treatment of alcoholic hepatitis
In severe forms of alcoholic hepatitis, to exclude the addition of a bacterial infection and minimize endotoxemia and hepatologists prescribe short courses of antibacterial drugs. Treatment is not complete without hepatoprotectors, the action of which is aimed at:
- normalization of liver function;
- creating conditions suitable for the restoration of damaged hepatocytes;
- improving the body’s ability to process alcohol and its impurities;
- restoration of liver cells;
- reducing the susceptibility of the liver to the destructive effects of pathogenic factors.
Conventionally, hepatoprotectors can be divided into:
- Medicines containing milk thistle (this plant qualitatively supports the functions of the liver, protects its cells from destruction and oxygen starvation);
- Medicines made on the basis of ademetionine (ademetionine protects hepatocytes from destruction, improves the flow of bile, neutralizes toxins that enter the body);
- Medicines containing bear bile (activate regeneration processes).
- Medicines based on “essential” phospholipids (block free radicals, reduce fatty liver disease, suppress the activation of stellate cells).
- Organic preparations of animal origin (stimulate intracellular renewal processes).
Surgical treatment of alcoholic hepatitis
Surgical treatment of alcoholic hepatitis that develops due to excessive alcohol consumption involves transplantation. The operation is performed quite rarely and is very expensive. It is used in the last stages of liver failure.
Liver transplants are successfully performed in Germany, Israel, and Turkey. The Russian Federation provides quotas for free treatment of this type at the expense of the federal budget.
The complexity of the surgical method lies not only in the high cost (on average one hundred and fifty thousand euros), but also in the problem of finding a donor. A person in good physical health can become a donor. Ideally this should be a relative. During the operation, approximately half of the donor's liver is taken, which is then regenerated to normal size. It is also possible to take the liver from a dead person, but then it does not take root as well.
After transplantation, a patient with alcoholic hepatitis faces a long recovery period, during which he needs to take immunosuppressants, drugs that promote the engraftment of the new liver.
Possible complications after surgery
- Complications that may occur immediately after liver transplantation include:
- Primary inactivity of the liver. Requires repeated surgery.
- Bleeding (occurs in 7% of cases).
- Immunological difficulties. The liver is an important organ and has a special relationship with immunity. At the same time, it is less vulnerable than other internal organs. However, some operated patients still experience rejection - acute (treatable) or chronic (not controlled). If the donor is a relative, the risk of immunological disorders and rejection is minimal.
- Vascular diseases manifested by thrombosis, hepatic artery stenosis, steal syndrome. The risk of developing these complications is 3.5%. They are dangerous and may require a second transplant.
- Portal vein stenosis/thrombosis (observed in 1.3%). Ultrasound diagnostics helps to detect pathology. If thrombosis is detected at an early stage, the outcome of the operation can be saved.
- Small liver transplant syndrome. Occurs only when part of an organ taken from a living donor is transplanted. The reason is that the size of the transplanted liver was incorrectly determined by doctors. If symptoms do not disappear within two days, a repeat operation is performed.
- Obstruction of the hepatic veins. Very rare.
- Bile leakage (occurs in 25% of cases). Bile entering directly into the abdominal cavity during the postoperative period.
- Infection. It can occur hidden and cause pneumonia. To prevent the development of an infectious disease, it is necessary to take antibacterial drugs until all catheters and drains are removed.
Treatment of alcoholic hepatitis at home
You can treat alcoholic hepatitis at home with the help of herbs. At the first symptoms of alcoholic liver damage, decoctions of yarrow, plantain, and dandelion can help. Garlic, horsetail, and thyme also have a choleretic effect. Currants and rose hips help strengthen the immune system. Natural hepatoprotectors are very effective: milk thistle, corn silk, knotweed leaves, agrimony, tansy. But it should be understood that it is impossible to completely restore liver function in the final stages of the disease without seeking qualified medical help.
You can increase the effectiveness of home treatment for alcoholic hepatitis by regularly drinking mineral water. Hydrocarbonate-sulfate water improves the composition of bile and promotes its separation. The chloride-sulfate composition has a choleretic and mild laxative effect.
In the remission stage, patients are recommended to undergo sanitary-resort treatment with mineral waters and mud. You should not expect a quick improvement in your well-being, but if you follow medical recommendations, there will be positive dynamics.
Folk remedies prepared from corn silk have a positive effect on the health of patients with alcoholic hepatitis. You can cleanse an inflamed liver with tea.
Treatment of cholestatic hepatitis
Treatment of chronic hepatitis with cholestatic syndrome should be based on eliminating the cause that led to cholestasis. If the cause of the disease is exposure to toxic factors or medications, then it is necessary to stop their entry into the body. All patients are recommended to adhere to diet No. 5, which includes the exclusion of spicy, fatty and fried foods. Be sure to minimize alcohol consumption, which negatively affects liver cells. A nutritious diet with sufficient protein is also recommended.
Drug therapy
At any stage of the disease, it is advisable to take fat-soluble vitamins A, E, and B12. To improve hepatocyte function, hepatoprotectors, essential phospholipids and lipoic acid can be prescribed. In the presence of intrahepatic cholestasis with high activity of the inflammatory process, the administration of small doses of prednisolone is indicated to reduce the severity of pathological changes.
If the patient is bothered by severe itching, it is necessary to use drugs to neutralize bile acids, such as cholestyramine or lignin. The most effective treatment for intrahepatic cholestasis is ursodeoxycholic acid, which improves the flow of bile. The drug is recommended for all patients with cholestatic hepatitis.
Surgery
If hepatitis is caused by extrahepatic cholestasis, it is necessary to eliminate its cause. Various operational methods are used for this:
- laparoscopic or open cholecystectomy;
- resection of the head of the pancreas;
- extraction of bile duct stones during RPCG;
- endoscopic balloon dilatation of the sphincter of Oddi, etc.
Alcoholic chronic hepatitis - case history
The term was added to the International Classification of Diseases in 1995.
From this moment the “documented” history of the disease “alcoholic hepatitis” begins. The name of the pathology is used to characterize inflammatory liver lesions that arise due to alcohol abuse and often progress to cirrhosis. According to medical research, 90% of alcohol ingested is broken down in the liver, releasing acetaldehyde. The named substance affects hepatocytes - organ cells. Alcohol metabolism products activate a number of chemical reactions that provoke:
- oxygen starvation of cells;
- development of hepatocyte necrosis;
- scarring of connective tissue;
- slowing down the process of protein formation in liver cells, which causes them to swell and the liver increases significantly in size.
Publications in the media
Acute viral hepatitis (AVH) is a group of acute viral diseases that occur with diffuse inflammation of the liver.
Etiology • Hepatitis viruses A (HAV), B (HBV), C (HCV), D (HDV), E (HEV), G (HGV). The pathogens are stable in the external environment. The genome of most hepatotropic viruses is RNA (except for HBV, which contains DNA).
Incidence: 134.9 per 100,000 population in 2001.
Mechanisms of transmission • Parenteral mechanism of transmission (viral hepatitis B, C, D, G). Characterized by a chronic course and the phenomenon of carriage •• Transfusions of blood and its preparations, hemodialysis, injections, surgical and dental treatment during the previous 6 months •• Sexual contacts with a person infected with hepatitis B, C, D viruses •• Children born from mothers infected with HBV, HCV, HDV, HGV •• Close household contact with a family member infected with HBV, HDV • Enteral (fecal-oral) transmission mechanism (viral hepatitis A, E). It is characterized by seasonality (autumn-winter) and a predominant affection of children and young patients. Diseases are always acute, have a favorable course, do not form carriers of the virus •• Contact with the patient 15–60 days before the onset of the disease •• Residence in an epidemiologically disadvantaged area •• Group morbidity with the formation of epidemic foci in children's and youth groups.
Clinical picture
• Incubation period •• With OVG A - 15–45 days •• With OVG B - 30-180 days •• With OVG C - 20-90 days •• With OVG D - 30-50 days •• With OVG E - 15 –60 days •• For OVG G and F, the duration of the period is not reliably determined.
• Pre-icteric period; duration 3–15 days •• Dyspeptic syndrome (nausea, vomiting, flatulence, constipation, diarrhea) is characteristic mainly of OVG A, C and E •• Intoxication syndrome (fever, general weakness, lethargy, apathy, irritability, sleep disturbance, loss of appetite ) •• Catarrhal syndrome (nasal congestion, hyperemia, granularity of the mucous membrane of the posterior wall of the pharynx) is characteristic of OVG A and E •• Joint and muscle pain is characteristic of OVG B and D •• Skin rash (spotty, maculopapular, urticarial) is characteristic only for OVG B •• Pain in the right hypochondrium and/or epigastrium; possible muscle tension in the projection of the liver, pain on palpation along the colon •• Enlarged liver, its pain on palpation •• Enlargement of the spleen •• Discoloration of feces and darkening of urine in the last 1-2 days of the period.
• Jaundice period (high period); duration ranges from 7–10 (common) to 30–40 (rare) days •• Jaundice. The appearance of icteric staining first of the mucous membranes, then of the skin (the icterus of the mucous membranes is always more pronounced and lasts longer than the jaundice of the skin). In the cholestatic form of AVH, jaundice is intense, long-lasting, and often accompanied by itching. The syndrome is not observed in anicteric and subclinical variants of AVH •• Hepatomegaly: the liver is enlarged, compacted, the edge is rounded, the surface is smooth, moderately painful on palpation; usually the left lobe is enlarged slightly more than the right •• Enlargement of the spleen in 30–50% of cases of all OVH (more often for OVH A) •• Symptoms of vagotonia (bradycardia, decreased blood pressure, expansion of the borders of the heart, muffled heart sounds, systolic murmur at the apex and at the point Botkin, accent and splitting of the second tone above the pulmonary artery, extrasystoles) •• Signs of moderate and severe course: dyspeptic syndrome (pain in the right hypochondrium and/or epigastrium, heartburn, belching, nausea, vomiting, diarrhea), intoxication syndrome (fever , malaise, weakness, drowsiness, decreased mood, decreased appetite) •• Markers of severe course: hemorrhagic syndrome (hemorrhages on the skin and mucous membranes; microhematuria; uterine, nasal and intestinal bleeding, bleeding from the gums), encephalopathy (psychomotor agitation, delirium, depression of consciousness in the form of somnolence, stupor, coma).
• The period of convalescence, determined from the moment of disappearance of jaundice until the complete clinical and laboratory resolution of the disease.
Features of the course of typical forms of common OVH
• Jaundice is a typical sign of AVH.
• OVG A •• The pre-icteric period is short (5–7 days). The onset of the disease is acute. Characterized by the predominance of intoxication syndrome with fever in the pre-icteric period, catarrhal syndrome, dyspeptic and asthenovegetative disorders •• With the appearance of jaundice, a decrease in intoxication and improvement of well-being are noted •• The icteric period lasts about 2-3 weeks; An enlarged spleen is often observed.
• OVH B •• The pre-icteric period is long (on average 14 days). In children, the pre-icteric period can be short (up to 1–2 days). The severity of the clinical form is not determined by the severity of the symptoms of the pre-icteric period! The onset of the disease is gradual. Characterized by moderate intoxication, joint pain and skin rash •• With the appearance of jaundice, increased intoxication and deterioration of health are possible, which is associated with a higher frequency of development of moderate and severe forms •• The jaundice period is long (4–6 weeks) with a gradual increase and slow resolution of jaundice .
• OVG C •• The pre-icteric period is erased with minor symptoms of intoxication and dyspeptic syndrome •• The icteric period is short-term (5–7 days); noted in 50% of patients; slight jaundice; intoxication is moderate •• It occurs much more easily than OVG B and OVG A.
• HBV D is registered only in persons infected with HBV, and occurs in two variants •• Coinfection (simultaneous infection with HBV and HDV). Signs: short prodromal period with severe fever, migrating pain in large joints, increasing intoxication during the icteric period, pain in the projection of the liver and/or epigastrium, the appearance of laboratory or clinical laboratory exacerbation 2-3 weeks after the onset of the disease, a long period of convalescence, benign course •• Superinfection (HDV infection of a person infected with HBV). Signs: short incubation period; short pre-icteric period (3–5 days) with severe fever, intoxication, repeated vomiting, joint pain; severe jaundice; development of edema and ascites; significant enlargement of the liver and spleen; repeated clinical and laboratory exacerbations; the development of a malignant form with a fatal outcome is possible.
• OVH E •• The clinical picture resembles OVH A; the pre-icteric period is erased, with a predominance of dyspeptic syndrome •• The icteric period is short (2 weeks), the development of cholestatic variants of AVH is possible •• An unfavorable course is noted in pregnant women (if infected in the second half of pregnancy) with the development of acute hepatic-renal failure and thrombohemorrhagic syndrome.
Features of the course of atypical forms of AVG • Erased form: slight and short-term (several days) jaundice; always proceeds easily • Anicteric form: there is no icteric period; proceeds easily • Subclinical form: only laboratory signs of hepatitis are recorded (cytolysis syndrome, usually no more than 1 week). There are no clinical symptoms.
Research methods
• Biochemical blood test •• Cytolysis syndrome: increased levels of ALT, AST; characteristic of all clinical variants of OVH •• Cholestasis syndrome: increased levels of total bilirubin (due to conjugated bilirubin), cholesterol, alkaline phosphatase, g-glutamyl transpeptidase; observed only in icteric forms •• Mesenchymal inflammation syndrome: increased immunoglobulin content, increased thymol test, decreased mercuric test; characteristic of all clinical variants of OVH •• Hepatodepressive syndrome: decrease in PTI, serum albumin concentration; registered only in severe forms.
• UAC •• Leukopenia; registered frequently; in severe, malignant and complicated forms, leukocytosis is noted •• Lymphocytosis; typical for mild and moderate forms; in severe, malignant and complicated forms, neutrophilia is recorded.
• OAM •• Bile pigments (mainly direct bilirubin) are recorded in typical forms of OBG; absent normally and in anicteric forms •• Urobilin (absent when the flow of bile into the gastrointestinal tract completely stops); characteristic of typical forms of OVG; not normally determined.
• Stool analysis •• Reduction or absence of stercobilin due to the cessation of bile flow into the intestines; determined normally; the appearance of stercobilin in feces during the icteric period of AVH is evidence of resolution of jaundice (a prognostically favorable sign).
Specific markers of common OVH
• OVG A •• HAV Ag (RIF). Viral Ag can be detected in feces; diagnostically low-specific, because the peak of its excretion occurs during the incubation and beginning of the icteric periods; used for epidemiological examination of contact persons •• Anti-HAV IgM (ELISA). Class M antibodies to the virus indicate acute infection •• Anti-HAV IgG (ELISA). Class G antibodies to the virus indicate a past infection and remain in the blood for life •• RNA-HAV (PCR, molecular hybridization). Virus RNA is detected from the first days of illness; it is not recorded during the icteric period.
• OVG B •• HBsAg (ELISA, RPGA). The surface Ag of the virus marks infection by the virus; appears 1.5 months after infection and persists throughout the disease until the period of convalescence •• Anti-HBcIgM (ELISA). Class M antibodies to viral nuclear Ag; in the absence of HBs, Ag marks an acute process; detected from the first days of the disease, can persist for several months •• Anti-HBcIgG (ELISA). Class G antibodies to the nuclear Ag of the virus indicate a previous HBV infection; determined for differential diagnosis and assessment of the completion of the viral process •• DNA-HBV (PCR, molecular hybridization). Viral DNA appears in serum simultaneously with other HBV Ags; disappears from the bloodstream at the beginning of 2 weeks of OVH; long-term persistence is evidence of chronic HBV infection; in the diagnosis of OVH B is rarely used.
• HCV C •• RNA-HCV (PCR). Virus RNA is detected in serum 1–2 weeks after infection •• Anti-HCV (ELISA, immunoblotting). AT to viral proteins encoded by both structural (C-100-3, 5-1-1) and non-structural (C-22, C-33c, E2/NS1 and NS5) parts of the RNA-HCV genome; test systems determine IgM (activity markers) and IgG; reference test - RIBA (immunoblotting).
• OVV D •• RNA-HDV (PCR). Virus RNA is a marker of active replication of the pathogen •• HDAg (ELISA, RIA). d-Ag during coinfection is detected in the serum on the 4th–7th day of jaundice and persists for 1–2 weeks; during superinfection, it is not always detected •• Anti-HDV IgM (ELISA). Anti-d-Ag class M antibodies are detected from the first days of jaundice; marker of active replication of the pathogen •• Anti-HDV IgG (ELISA). Antibodies to d-Ag class G mark the period of convalescence of co-infection with AVG D; in case of superinfection, it is detected in high titers during the height of the disease (a laboratory criterion for differentiating two variants of infection).
• OVG E •• RNA-HEV (PCR, molecular hybridization). Viral RNA is detected from the first days of illness; •• Anti-HDV IgM (ELISA) is not recorded during the icteric period. Antibodies to class M virus Ags are recorded from the 10th–12th day of illness, they persist for 1–2 months •• Anti-HDV IgG (ELISA). Antibodies to class M virus Ags appear a month after the illness.
For differential diagnosis , see Chronic viral hepatitis.
Treatment • Mandatory hospitalization. The criterion for discharge from the hospital is the disappearance of clinical signs of the disease and normalization of laboratory parameters • Diets No. 5, 5a • Bed rest - in case of intoxication and severe jaundice • You should not prescribe many drugs or medical procedures at the same time • For cholestasis - ursodeoxycholic acid, hepatofalk planta, ademetionine • In severe forms - detoxification infusion therapy, protease inhibitors, antibiotics • In acute liver failure - extracorporeal detoxification methods.
Complications • Acute liver failure • Inflammatory processes in the biliary tract • Liver cirrhosis • Hepatocellular carcinoma.
Course and prognosis. Most hepatitis cures spontaneously within 1–2 months. 5–10% of OVH B becomes chronic. Mortality with OVH B in the elderly and after blood transfusion reaches 15%. Hepatitis C is characterized by a wave-like course; the probability of becoming chronic is 50%.
Prevention • Passive immunization of children born from HBsAg-positive (especially HBeAg-positive) mothers - immunoglobulin (IgHB) together with vaccination • Active prevention - inactivated (Havrix-A) and recombinant vaccines (Engerix-B, H-B-VAX II) - to prevent HBV and HAV infections. Prevention of hepatitis A - double parenteral administration of the vaccine with an interval of 1 month. Prevention of hepatitis B is a three-time administration of the vaccine (1 and 5 months after the first injection). When vaccinating newborns - repeated administration of the vaccine (the first dose is administered on the first day of life) - after 1, 2 and 12 months • Measures for the prevention of AVH with a parenteral transmission mechanism: the use of disposable medical equipment, testing blood products for the presence of markers of viral hepatitis, a system of strict control of cleaning and sterilization of reusable medical instruments, vaccination • Measures to prevent HCV with the fecal-oral transmission mechanism: early isolation of sick people, control of the water supply and public catering systems, vaccination.
Reduction. AVH - acute viral hepatitis
ICD-10 • B15 Acute hepatitis A • B16 Acute hepatitis B • B17 Other acute viral hepatitis
Prognosis for alcoholic hepatitis
The prognosis for treatment for alcoholic hepatitis is variable. It is determined by the severity of the diagnosed disease, the presence or absence of background cirrhosis. According to statistics, the fatal outcome is 10-30%. Hepatologists give an unfavorable prognosis if they detect: renal failure, encephalopathy, an increase in blood clotting time by more than 50% (compared to the norm).
In 38% of patients, hepatitis progresses to cirrhosis within five years. In 52% of patients, the acute form of the disease becomes chronic and liver fibrosis develops. Only 10% of people who have undergone complex treatment experience a complete recovery.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.