ACUTE STOMACH
- a clinical symptom complex that develops with injuries and acute diseases of the abdominal organs and retroperitoneal space; this requires or may require urgent medical (usually surgical) assistance. Acute abdomen, while not being a final diagnosis, serves as an alarming signal forcing a doctor or paramedic to take immediate measures for emergency hospitalization of the patient in a specialized institution, where the necessary diagnostic and therapeutic measures should be carried out as soon as possible after his admission. Sometimes in honey. In the literature, especially in pediatric literature, the term “abdominal syndrome” is used, Crimea unites all pathological conditions accompanied by acute abdominal pain, including those that are not subject to surgical treatment (see Pseudo-abdominal syndrome). Thus, abdominal syndrome is a broader concept than Acute abdomen.
Causes
The occurrences of Acute abdomen are numerous and can be grouped as follows.
1. Injuries to the abdominal organs and retroperitoneal space, which are usually divided into closed and open (see Abdomen, injuries; Retroperitoneal space, injuries). The most common cause of Acute abdomen is damage to the hollow organs of the gastrointestinal tract and bladder. Symptoms of an Acute abdomen often occur with fractures of the pelvic bones, as well as the lower thoracic and lumbar spine, which is due to the formation of a retroperitoneal hematoma in these cases. The cause of Acute abdomen is sometimes through damage to the stomach wall, which occurs in some cases during chemical reactions. his burns. Relatively rarely, the cause may be a rupture of the colon, which occurs when air enters its lumen under high pressure.
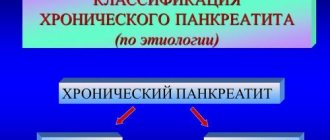
2. Inflammatory diseases, including peritonitis (see). The most common cause of pancreas is acute inflammatory processes in the appendix, gall bladder, and pancreas. Less often, its cause may be phlegmon of one of the sections of the gastrointestinal tract. tract, diverticulitis, epiplitis, etc.
3. Perforation of a hollow organ (see Perforation). Most often, it occurs as a result of various diseases of the abdominal cavity and retroperitoneal space (for example, acute cholecystitis, acute appendicitis, ulcers and tumors of the gastrointestinal tract, diverticula of the small and large intestine, bladder, etc.). In some cases, perforation can occur as a result of entry into the gland. tract of foreign bodies (bones, needles, etc.).
4. Internal bleeding into the lumen of the colon. tract (see Gastrointestinal bleeding), into the abdominal cavity (eg, rupture of the tube during tubal pregnancy) and retroperitoneal space (eg, rupture of the kidney or dissecting aneurysm of the abdominal aorta).
5. Intestinal obstruction resulting from intestinal volvulus, nodulation, intestinal strangulation in an internal or external hernia, obstruction of the intestine from the outside or inside, intussusception, compression of the intestine by adhesions (see Intestinal obstruction).
6. Acute disorders of mesenteric circulation (arterial and venous), leading to infarction (gangrene) of the intestine. In this case, the symptoms of dynamic intestinal obstruction usually predominate. As a rule, mesenteric circulation disorders occur against the background of pronounced changes in the vascular wall and blood coagulation system.
7. Inflammatory processes in the uterine appendages, ectopic pregnancy, ovarian apoplexy, torsion of the tumor stalk or ovarian cyst, necrosis of the uterine myomatous node or ovarian tumor.
8. A number of diseases of the cardiovascular, respiratory and other systems, certain infectious diseases. Wedge, the picture in these diseases can cause diagnostic errors (see Pseudo-abdominal syndrome).
9. In children - birth trauma (with damage to the liver, spleen and other organs), congenital and acquired intestinal obstruction, intestinal perforation in ulcerative colitis, etc.
What is acute abdomen
The internal organs are covered with peritoneum. When any organ becomes inflamed, irritation of the peritoneum occurs. It causes abdominal muscle spasms. Pain in acute abdomen is a compensatory reaction.
In this case, pain in one place can lead to sensations of pain in a completely different place. This is called pain radiation. The most famous example is pain in the arm, although at this moment the person is having a heart attack.
Acute abdomen is possible at any age, both in children and adults.
The concept of “acute abdomen” was introduced back in 1940 by G. Mondor, who wrote a book on the diagnosis of emergency conditions. Mondor called such pathological processes “a catastrophe in the abdominal cavity.” After the publication of the work, surgeons began to study all possible ways of diagnosing and treating acute abdominal syndrome and its causes. It became known why severe abdominal pain needs to be responded to as quickly as possible. You can’t wait, “suddenly it will go away on its own.”
Acute abdominal syndrome is a manifestation of inflammation of the abdominal organs. A variety of diseases can manifest themselves in similar ways, so acute abdominal pain is an insidious sign. This always requires urgent diagnosis to rule out life-threatening conditions.
Causes of acute abdomen in adults
The syndrome is caused mainly by inflammatory processes in the abdominal cavity. The intestines, gallbladder, and pancreas may become inflamed.
Bleeding also provokes an acute abdomen. For example, an ulcer that has reached the stage of perforation - the formation of a through hole in the wall of the stomach or intestines, rupture of the spleen, ovary and other organs. Ectopic pregnancy also leads to heavy bleeding.
Stay up to date!
First aid for injuries, poisoning, bites: KP memo
Equally important is normal blood supply to all organs. If the vessels of the peritoneum are spasmed, blocked by blood clots or air bubbles, the organs begin to experience oxygen starvation. This causes pain, and the retention of metabolic products causes inflammation.
Also common causes are infections, poisoning, abdominal trauma, and tumors. Less commonly accompanied by signs of an acute abdomen are diseases of the kidneys and female and male internal genital organs.
Symptoms of acute abdomen in adults
Acute abdomen is different from normal abdominal pain during menstruation, for example. With an acute abdomen, the pain begins quite sharply. At the same time, the front wall of the abdomen tenses and becomes “stone”. The peristalsis of the digestive tract is upset. This can cause diarrhea, constipation, and flatulence.
Other signs will vary depending on the disease that caused the acute abdomen. Usually the pain is dagger-like, sharp, and gradually increases. Sometimes temporary relief occurs, vomiting and nausea are possible. Temperature is often elevated and heart rate is increased.
The symptoms of an acute abdomen are difficult to miss: the stomach begins to ache sharply, like a dagger, the temperature often rises and nausea sets in. Photo: Pixabay
If there is heavy bleeding or leakage of gastric contents in the abdominal cavity, the abdominal muscles become stronger. A “vanka-stand up” symptom may appear. In this case, the pain noticeably decreases in a sitting position. If you quickly move from a lying position to a sitting position, dizziness develops and loss of consciousness is possible.
With acute abdomen syndrome, at some point paleness, chills, and cold sweat occur. But these signs may appear quite late. In the most advanced cases, shock is possible: apathy, lethargy, the skin becomes sallow in color, the face becomes sharper.
Treatment of acute abdomen in adults
Successful treatment depends on quickly identifying the cause. It is important to call a doctor as soon as possible. In order not to aggravate the situation, you should not heat your stomach or take medications, no matter how painful it may be. Painkillers will distort the picture of pain, and it will be more difficult to understand what is happening. This is dangerous because every minute can count. You should also not eat, drink or give an enema.
The main treatment is surgery, which can rarely be avoided. After emergency diagnosis, the patient is operated on. During the operation, the treatment method is finally determined. Correct diagnosis is very important. It is necessary to exclude pathology that only resembles an acute abdomen, but is not one. It is dangerous for patients with chronic serious illnesses to undergo emergency surgery - this can worsen their condition or lead to death. For example, this is especially dangerous in case of myocardial infarction, renal or hepatic colic.
Diagnostics
The doctor collects anamnesis and interviews the patient. It is necessary to remember exactly how and when the pain began, how it changed. Was there vomiting, diarrhea or other phenomena, how did this happen? For women, gynecological data is additionally clarified - what diseases they had, cycle, etc.
Next, the patient is examined, blood pressure and pulse are checked, and the abdomen is palpated. This is painful, so the pressure is as gentle as possible. The presence of Shchetkin-Blumberg's symptom is checked - during acute inflammation, the patient's pain always increases if you press on the stomach and sharply remove your hand.
Additionally, a rectal examination is possible, especially often used in children. All women undergo a vaginal examination to exclude diseases of the reproductive system.
Important! Acute abdominal syndrome requires hospitalization. In a hospital setting, blood tests are taken, abdominal x-rays, and ultrasounds are performed.
Inna MazkoGastroenterologist, therapist
The latter method is best suited for identifying problems with the reproductive organs. Sometimes colonoscopy is used - examination through the intestines using a flexible colonoscope, as well as gastroscopy through the esophagus.
Sometimes it is still not possible to determine the cause of pain and inflammation. In such severe cases, an operation is performed for diagnostic purposes - through minimal holes. Sometimes a complete opening of the abdominal cavity is required.
Modern methods of treatment
You should call an ambulance as quickly as possible. Calm the person, lay him on his back and apply cold to his stomach. This will reduce possible bleeding or inflammation.
Next, the patient is hospitalized either in the hospital or immediately in intensive care if the condition is critical. First, anti-shock therapy is carried out, otherwise there is a risk of death, and only then further treatment.
To the point
Such a banal but dangerous appendicitis: what you need to know
Using diagnostics, they find out what the cause of the acute abdomen is, and urgent surgery is performed. This usually occurs within 2 to 3 hours after hospitalization. If the patient is already in agony, the operation is performed immediately.
Specific actions and methods of treatment are determined already on the surgical table - eliminating bleeding, removing dead tissue, restoring the integrity of damaged organs. The patient must take antibiotics, the sutures are treated with antiseptics - everything to eliminate infection and inflammation.
Treatment tactics
A patient diagnosed with O. g. must be immediately hospitalized in a specialized institution. Transportation of patients in serious condition should be carried out carefully, taking into account the possibility of carrying out the necessary resuscitation measures during the process. Character to treat. events for O. depends primarily on the cause of the disease. For certain inflammatory processes that are not accompanied by the development of peritonitis, complex conservative treatment is carried out, including diet, anti-inflammatory, detoxification and other measures. However, in most cases O. (for peritonitis, perforation of hollow organs, mechanical intestinal obstruction, internal bleeding, etc.) surgical treatment is necessary. In severe condition of the patient with severe intoxication and dehydration, intensive preoperative preparation is necessary for 2-3 hours. in order to correct any violations that have arisen. In difficult cases, the nature and scope of the treatment. activities should be determined by a council of specialists (surgeon, resuscitator, therapist, etc.). In certain cases of the patient’s extremely serious condition (for example, with massive gastrointestinal bleeding), surgical intervention is performed immediately after the patient’s admission to the hospital, while simultaneously performing resuscitation measures.
Until the issue of the need for emergency surgery is resolved, you should refrain from using analgesics, narcotics, sleeping pills, antipsychotics, tranquilizers, laxatives, enemas, since they can significantly distort the symptoms of the disease, which can cause a diagnostic error. To a certain extent, this applies to antibiotics, the use of which can temporarily create a misleading picture of relative improvement and cause an unreasonable delay in surgical intervention.
Prevention of acute abdomen in adults at home
Prevention consists precisely in preventing diseases, and not the acute abdomen itself. Because it is only a manifestation of disease.
You can reduce the risk of such a dangerous syndrome with proper nutrition, an active lifestyle, and weight control. It is important to monitor the condition of organs if they are already affected. For example, in case of chronic diseases of the kidneys, liver, stomach, you need to be examined on time and take prescribed medications. If an acute abdomen does develop, the prognosis is rather ambiguous. Recovery is greatly influenced by the speed of visiting a doctor, the person’s condition, and age. Children and the elderly suffer from this condition worse.
4.Treatment
Almost all cases of acute abdomen create absolute indications for emergency surgery. Currently, the standard of care, based on extensive statistical material, requires making and implementing a decision within a time period not exceeding six hours from the moment of the onset of diagnostically significant symptoms.
Therefore, it is worth recalling once again that in any situation and in any area, with any refusals and any dissimulation (deliberate concealment of sensations) on the part of the patient - who, before the onset of symptoms characteristic of an acute abdomen, could be as strong and healthy as he likes - as well as with any doubts among relatives, the time factor is critical, and the faster help is provided, the higher the chances of avoiding death. The question should be posed precisely in this formulation.
Popular questions and answers
Often, when experiencing abdominal pain, people prefer to take painkillers and charcoal and wait until it “goes away on its own.” Unfortunately, in the case of an acute abdomen, this is too dangerous. If you have severe abdominal pain, it is better to play it safe and call an ambulance. Gastroenterologist Inna Mazko will tell you more about all the complications of acute abdominal syndrome
What complications can occur with an acute abdomen?
The most common causes of acute abdomen: ● appendicitis;
● intestinal obstruction; ● acute pancreatitis; ● perforation of a gastric or duodenal ulcer; ● rupture of an ovarian cyst; ● ectopic pregnancy. Complications of these diseases are: bleeding, sepsis, shock, abscesses (suppuration) in the abdominal cavity, purulent peritonitis, etc.
When to call a doctor at home if you have an acute abdomen?
If you have severe abdominal pain, you should always call an ambulance or a doctor at home as quickly as possible.
Is surgery inevitable for acute abdomen?
Symptoms of an acute abdomen indicate a big problem in the abdominal cavity and almost always require emergency surgical care.
Material on the diagnosis of “acute abdomen” is presented. The main reasons for its occurrence are considered. The cardinal symptoms of acute surgical diseases of the abdominal organs are described in detail. Particular attention is paid to the interpretation of pain syndrome based on the anatomical and physiological characteristics of the innervation of internal organs and the anterior abdominal wall. Recommendations for preventing diagnostic errors are given.
Acute abdomen
The material for the diagnosis of “acute abdomen” and the main reasons for its occurrence are presented. It is detailed description of the cardinal symptoms of acute surgical diseases of abdominal organs. Particular attention is paid to the interpretation of pain at the basis of anatomical features physiological innervation of internal organs and abdominal wall. The recommendations for the prevention of diagnostic errors are given.
An analysis of lethal outcomes in acute surgical pathology of the abdominal organs shows that in most cases they are based on late admission of patients to the surgical hospital. And no matter how brilliantly the operation is performed, if it is performed at an advanced stage of the pathological process, only at the cost of “heroic” efforts does it become possible to achieve the desired result - to save the life of a seriously ill patient.
Diagnosis of acute surgical diseases at the prehospital stage has a characteristic feature - the specialist who first examines the patient is, in most cases, a non-surgical doctor. Since the time factor in emergency surgery plays a decisive role in the development of the pathological process, the qualifications of a given doctor ultimately determine the future fate of the patient.
The patient’s ability to detect symptoms of an acute surgical disease and promptly seek medical help largely depends on the level of his culture and education. Unfortunately, we have to admit the opposite phenomenon.
Often the cause of a serious complication of acute appendicitis, which is most often encountered in surgical practice, is the underestimation of the early manifestations of the disease by the patient himself. However, there are many examples where patients promptly sought medical help, but the symptoms of an “acute abdomen” were not recognized and surgical interventions were performed when the clinical picture of peritonitis was beyond doubt. There is also a number of non-surgical diseases, the manifestation of which is often accompanied by abdominal symptoms. Performing unnecessary laparotomy in such patients can aggravate the course of the underlying pathological process and lead to death. So, what is an “acute abdomen” and how to avoid mistakes in recognizing it?
“Acute abdomen” (AB) is one of the most generalized clinical syndromes that develops with traumatic injuries and acute surgical diseases of the abdominal organs and retroperitoneal space. The appearance of this symptom complex predetermines the immediate referral of the patient to a surgical hospital. Thus, the term OB should be considered not as medical jargon, but as a working hypothesis at the prehospital stage, which always requires the doctor examining the patient to take active action to clarify the nature of the disease.
The causes of coolant are numerous and can be grouped as follows:
- injuries of the abdominal organs and retroperitoneal space;
- acute inflammatory diseases of the abdominal organs;
- perforation of hollow organs;
- intra-abdominal bleeding;
- acute intestinal obstruction;
- acute disturbance of mesenteric circulation.
If a patient develops a symptom complex of coolant, the surgeon is asked questions that require an immediate answer:
1. Are the existing symptoms really caused by acute surgical pathology?
2. Does the patient need surgery and what is the degree of urgency?
To answer the first question, it should be remembered that, despite the variety of causes of coolant, its clinical picture is strictly delineated and determined by a number of cardinal symptoms:
1. Pain.
2. Vomiting.
3. Gas retention and lack of stool.
4. Protective muscle tension of the anterior abdominal wall.
The severity of cardinal symptoms depends on the duration of the disease, the age of the patient and the functional state of the body. The greatest difficulties arise when making a correct diagnosis in children and the elderly, pregnant women, people in a state of shock, alcohol intoxication and drug influence, patients with severe mental disorders. It is very important to clarify the chronological order and details of the occurrence of these symptoms. Since abdominal pain, as a rule, accompanies any acute disease of the abdominal organs and is the main reason for patients seeking medical help, the doctor’s attention should primarily be focused on finding out their cause, time of occurrence, nature and location.
The feeling of pain occurs involuntarily under the influence of a painful stimulus, which excites pain receptors and is processed in the diencephalon. Thus, pain is a subjective sensation of a person, which must be taken into account for its correct interpretation.
In accordance with the anatomical and physiological characteristics of the nervous system of the abdominal cavity and anterior abdominal wall, three main types of pain are distinguished:
1. Visceral pain.
2. Somatic pain.
3. Referred (referred) pain.
Receptors that perceive visceral pain are located on the visceral peritoneum, which covers the internal organs, and respond to an increase in intracavitary pressure, and not to direct irritants (burn, incision, necrosis). Pain impulses traveling along visceral afferents reach only the subcortical centers, so such pain does not have a clear localization. Depending on the affected organ, visceral pain can be approximately localized in the epigastrium, periumbilical region, lower abdomen, etc. It does not intensify when the patient’s body position changes; its intensity can be wavy or paroxysmal in nature.
An example of such pain is various colics (bilious, intestinal, appendicular, renal, etc.), which does not exclude acute surgical pathology in the initial stage of its development (acute cholecystitis, acute appendicitis, acute intestinal obstruction, acute pancreatitis, mesenteric thrombosis). The transition of cramping pain to constant may indicate a violation of blood circulation in the wall of the organ due to high intracavitary pressure. The well-known Volkovich-Kocher symptom in acute appendicitis shows how visceral pain, localized in the initial stage of the disease in the epigastric region, subsequently moves to the right iliac region. This feature is associated with the transition of the inflammatory process from the visceral peritoneum of the appendix to the parietal peritoneum of the iliac fossa. The pain that arises is called somatic . Its receptors are located in the parietal peritoneum. Since impulses traveling along somatic afferent pathways reach the cerebral cortex, these pains are always localized, are constant and increase in intensity. They intensify with changes in body position, coughing, deep breathing and walking. Due to intense pain that occurs during perforation of hollow organs, patients prefer to lie on their side with their knees brought to the chest, relaxing the muscles of the anterior abdominal wall and thereby alleviating their condition. At the moment of perforation of a stomach or duodenal ulcer, pain immediately reaches its maximum values. After some time, the intensity of somatic pain may decrease, which is associated with the peculiarities of the impact of pathological contents on the parietal peritoneum. This period of “imaginary well-being” can be misinterpreted, which leads to diagnostic errors at the prehospital stage. In this case, the doctor conducting the examination should pay attention to the appearance of symptoms in the patient indicating the development of endogenous intoxication (thirst, dry mouth, tachycardia) and intestinal paresis (nausea, vomiting, bloating, lack of stool and non-passage of flatus).
Thus, clinical signs of somatic pain, confirmed in doubtful cases by special research methods, serve as an indication for emergency surgical intervention.
Features of segmental anatomical relationships between the autonomic nervous system and spinothalamic nerves often lead to irradiation (reflection) of visceral pain. Since the same neurons in the dorsal horns of the spinal cord receive impulses coming from internal organs and from the surface of the body, the central nervous system does not always accurately differentiate the starting point of irritation. In this case, pain is projected not onto the area of the focus of the pathological process in the abdominal cavity, but onto the surface of the body, which is innervated by this spinal center. The localization of such radiating pain corresponds to the Zakharyin-Ged zones. Often the pain spreads beyond the abdomen. A typical example is the pain that appears in the shoulder girdle and the side of the neck with a perforated ulcer of the stomach or duodenum, pleurisy, hemoperitoneum, a destructive process in the gallbladder (Elecker's symptom). Due to irritation of the diaphragm by pathological contents of the abdominal cavity (intestinal contents, bile, blood), pain impulses are transmitted along the phrenic nerves to the fourth cervical segment and the areas that are innervated by the CIV. This feature forces the patient to take a position that facilitates the movement of peritoneal contents to other parts of the abdominal cavity and thereby reduces pain impulses. If there is a forcible attempt to change it, the patient again takes the original position (the “vanka-stand up” symptom). Another example of radiating pain is thoracoabdominal syndrome, which occurs due to pathology of the chest organs. Since the six lower intercostal nerves take part in the innervation of the anterior abdominal wall, lower lobe pneumonia, pleurisy, rib injuries, and pericarditis can occur with acute pain in the abdomen and tension in the abdominal muscles (thoraco-abdominal syndrome). Knowing the characteristics of radiating pain can help in making the correct diagnosis and avoiding unnecessary laparotomies.
An important feature of abdominal pain in acute surgical pathology is that it usually precedes the appearance of other symptoms (vomiting, fever, icterus of the skin and mucous membranes, flatulence and diarrhea), which over time can have independent significance.
It remains to add that intense pain involuntarily affects the autonomic innervation, which can be accompanied by tachycardia, a drop in blood pressure, increased sweating, and involuntary urination.
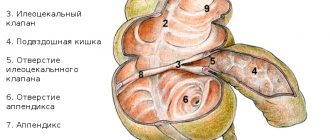
Vomiting is the next most common symptom of coolant. Its presence and nature often have no independent significance, except in cases of acute intestinal obstruction and gastroduodenal bleeding. Thus, with high small-intestinal obstruction, vomiting, being an early sign of the disease, is permanent and leads to rapid exhaustion of the patient. However, with low small-intestinal and large-intestinal obstruction, vomiting occurs in the later stages of the disease. The vomit is foul-smelling (“fecal vomit”) and is large in volume. Vomiting can be observed not only when the gastrointestinal tract is obstructed, but also occurs reflexively with renal colic, torsion of an ovarian cyst, acute pancreatitis, and acute cholecystitis. In acute appendicitis, vomiting is often one-time, less often repeated or repeated, but it is not indomitable. Most patients with ongoing intense bleeding from the stomach and duodenum experience vomiting of blood with clots. Characteristic vomiting is “fountain” or “mouth full”, which occurs when bleeding from varicose veins of the esophagus. Vomit the color of coffee grounds is often observed. It acquires this appearance due to the combination of hemoglobin with free hydrochloric acid to form hydrochloric acid hematin, which occurs with mild or stopped gastroduodenal bleeding.
The absence of stool and non-passage of gases is an important symptom of coolant, indicating mechanical or functional intestinal obstruction. This symptom is an early sign of colonic obstruction. It must also be remembered that with small intestinal obstruction, especially at the beginning of the disease (the first 6 hours), there may be stool and spontaneous passage of gases due to emptying of the distal intestines. The development of peritonitis leads to reflex inhibition of intestinal motor activity. However, with pelvic peritonitis, diarrhea and tenesmus may occur due to irritation of the rectal ampulla by peritoneal exudate. This feature is often observed in destructive pelvic appendicitis.
N. _ B. _ Coprostasis and non-passage of gases often accompany acute appendicitis in elderly and senile people.
The symptom of protective muscle tension (defense musculaire) clinically manifests itself due to irritation of the parietal peritoneum and occurs in parallel with somatic pain, being the result of a visceromotor reflex. Irritants of peritoneal receptors can be gastrointestinal contents, bile, urine, blood and peritoneal exudate. Impulses coming from the receptor field are transmitted to the corresponding segment of the spinal cord and from the motor neurons of its anterior horns to the muscles innervated by this segment, which enter a state of motor contraction. The protective tension of the muscles of the anterior abdominal wall causes a kind of immobilization and provides rest to the abdominal organs, creating optimal conditions for delimiting the pathological process. Assessing the clinical significance of the symptom of protective muscle tension, the famous French surgeon G. Mondor wrote: “Of all pathologies, there is hardly a more accurate, more accurate, more useful and more life-saving indicator.” The importance of this indicator for diagnosis lies in the fact that its localization mainly corresponds to the location of the diseased organ; the intensity of the muscle reaction often gives an idea of the degree of the inflammatory process. Despite its apparent simplicity, its identification will largely depend on the experience and skill of the surgeon. The severity of this symptom is determined not only by the quality of the current stimulus, but also by the place of its impact on the peritoneum. The latter is explained by the fact that not all areas of the peritoneum are equivalent as receptor fields for this reflex. Thus, a distinct defense musculaire occurs when the parietal peritoneum lining the upper and middle floors of the abdominal cavity is irritated. Protective muscle tension (PMT) is less pronounced when the peritoneum in the pelvic area is irritated. The duration of MN, which can be observed over several days, is of practical importance. This unusual duration of contraction of skeletal muscles, which easily tire under normal conditions, indicates the inclusion of special mechanisms in the implementation of mental health. Over time (after about 12 hours), a gradual weakening of muscle tension is observed, which is accompanied by increasing endogenous intoxication, metabolic and water-electrolyte disturbances characteristic of the late stages of general purulent peritonitis.
Crucial to detecting minor signs of MN is compliance with a number of methodological techniques that the doctor examining the patient must master. Pay attention to the following features:
- The study should take place in a warm room.
- The patient should lie calm and relaxed (as far as possible with this pathology).
- Before palpation begins, you should warm your hands, ask the patient to breathe deeply into the stomach and cough. In this case, a sharp increase in pain may be observed if the inflammatory process spreads to the parietal peritoneum.
- Palpation of the abdomen should begin superficially at the maximum distance from the area where the patient feels the greatest pain, gradually and methodically moving the hands to this area.
- When identifying a symptom of MN, it is necessary to determine its voluntary or involuntary (true) nature. Voluntary muscle contraction, as a rule, decreases with deep inhalation and subsequent exhalation, bending the legs at the knee and hip joints (false defense musculaire).
- Deep palpation should be performed at the very end of the examination to diagnose tumor formations and deeply localized sources of pain.
An intense and rapidly developing symptom of MN is observed with perforated ulcers of the stomach and duodenum. Bile and urine poured into the abdominal cavity have less effect on the parietal receptors. Blood causes the least irritation. However, in the generation and sending of impulses to the abdominal muscles, receptors not only of the parietal peritoneum, which form the main receptive field of the brainstem, take part, but also of the internal organs themselves. This feature allows us to explain a number of atypical clinical cases associated with the difficulty of diagnosing acute surgical pathology. The physiological characteristics of the body should also be taken into account. Thus, the symptom of MN is less pronounced in elderly people, in the early postpartum period, in patients in a state of collapse, toxemia, shock, or alcohol intoxication.
Other symptoms identified during examination of patients with abdominal pain can also help in diagnosing an “acute abdomen”. At the same time, you should not get too carried away in reproducing them, remembering that symptoms should not be counted, but weighed. An experienced clinician uses only a few, well-tested in practice, signs.
Symptoms of acute appendicitis
1. With a typical location of the appendix:
Bartomier-Mikhelson . Increased pain on palpation in the right iliac region with the patient positioned on the left side.
Volkovich-Kocher . The pain initially occurs in the epigastric region and only after some time is concentrated in the right iliac region.
Razdolsky. Percussion or light tapping of the abdominal wall with fingertips reveals pain in the right iliac region.
Rovzinga . With your left hand, press on the abdominal wall in the left iliac region and make a short push with your right hand in the left hypochondrium. Colon gases move proximally when pushed, causing sharp pain in the right iliac region in acute appendicitis.
Sitkovsky . Increased pain in the right iliac region when the patient lies on his left side.
Soresi . Pain in the right iliac region that occurs when coughing.
2. With a pelvic location of the appendix:
Cope (obturator muscle symptom). With the patient lying on his back, the leg is bent at the hip and knee joints at an angle of 900. When the right hip is rotated inwards, an increase in pain in the right iliac region is noted.
Rotter . A rectal examination reveals sharp pain in the right wall of the rectal ampulla.
Supolta - Seye . Taking a deep breath causes pain behind the bladder in the patient.
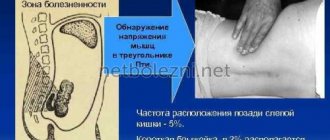
3. With a retrocecal location of the appendix:
Yaure - Rozanova . Pain when pressing on the area of Petite's triangle.
4. During pregnancy:
Brando . Increased pain in the right half of the abdomen when pressing on the left rib of the pregnant uterus.
Mikhelson . Increased pain in the right half of the abdomen when the patient is positioned on the right side, when the pregnant uterus presses on the inflamed appendix.
Symptoms of perforated gastric and duodenal ulcers:
Bailey (perverted thoraco-abdominal rhythm). When inhaling, the abdominal wall is drawn in simultaneously with the chest rising.
Grekova . Slowing of the pulse in the first hours after the ulcer perforates.
Dieulafoy . Sharp stabbing pain in the abdomen.
Clarke . Disappearance of “liver dullness” upon percussion.
Mondor triad. Acute stabbing pain in the abdomen, protective tension in the muscles of the anterior abdominal wall, history of ulcers.
Ratner-Wicker . Long-term persistent muscle tension in the right upper quadrant of the anterior abdominal wall with the general satisfactory condition of the patient. Characteristic for covered perforation.
Elekera (phrenicus symptom). Abdominal pain radiating to the shoulder or shoulder blade. It can also occur with intra-abdominal bleeding.
Peritoneal symptoms:
Winter . The anterior abdominal wall is not involved in the act of breathing.
Mendel . Pain that occurs when you lightly tap your fingertips on the anterior abdominal wall.
Stokes law. Widespread inflammatory processes in the abdominal cavity cause paralytic ileus.
Trendlenburg . Plank-shaped abdomen combined with contraction of the muscles supporting the testicle.
Shchetkin - Bloomberg . Increased pain when sharply tearing off the fingers of the hand palpating the anterior abdominal wall.
Symptoms of intra-abdominal bleeding:
Kulenkampf . With a soft abdomen, sharp pain upon percussion of the anterior abdominal wall.
Rozanova (symptom of “Vanka-Vstanka”). The patient lies on his left side with his thighs tucked toward his stomach. When you try to turn him over onto his back or the other side, he immediately turns over and takes his previous position. Observed when the spleen ruptures.
History and physical examination results provide up to 60-70% of the information necessary to establish the correct diagnosis. In order not to complicate the course of the pathological process and not to veil its clinical manifestations until examined by a surgeon, you should not: prescribe analgesics and antibiotics, use laxatives and cleansing enemas, wash the stomach, prescribe thermal procedures. At the prehospital stage, there is always overdiagnosis of the “acute abdomen”, which indicates the wariness of doctors in the polyclinic network and emergency medical services regarding acute surgical diseases, a lack of time and opportunity for a detailed examination of the patient. Nevertheless, the percentage of fatal diagnostic errors, when acute surgical pathology is not recognized in time, continues to remain quite high. Therefore, there is a rule according to which all patients with acute abdominal pain must be sent to a surgical hospital for urgent measures to clarify the nature of the disease. Carrying out dynamic monitoring of such patients on an outpatient basis is a serious mistake.
Currently, the arsenal of the emergency diagnostic program includes modern methods of radiological examination of the abdomen (ultrasound, CT) and video laparoscopy. This provides invaluable assistance in objectifying diagnoses of acute cholecystitis, destructive pancreatitis, appendicitis, acute gynecological pathology, and traumatic injuries to the abdomen.
Paradoxically, the use of unfounded diagnostic tests in emergency surgery increases the likelihood of false-positive results and the percentage of wasted laparotomies. However, when objective examination data can be interpreted ambiguously and the cause of acute abdominal pain remains unclear, a delay in performing laparoscopy and persistent continuation of conservative treatment should be considered a gross tactical error.
I.S. Malkov
Kazan State Medical Academy
Malkov Igor Sergeevich - Doctor of Medical Sciences, Professor, Head of the Department of Surgery