The gallbladder in the human body is a completely replaceable system. Therefore, when indications indicate that it would be better for the patient if the bladder is removed, it is removed without much regret. Despite the fact that the gallbladder is not a vital organ, its amputation is a serious stress for the body. And he will need a lot of internal resources and strength to redistribute the “responsibilities” of the bubble to other systems. It is during this difficult postoperative and critical period for organs and systems that various complications may arise. Among which are serious pains in the stomach.
After removal of the gallbladder, why does the stomach hurt, what factors and circumstances cause these unpleasant feelings, which significantly reduce the quality of life?
Causes of pain after removal
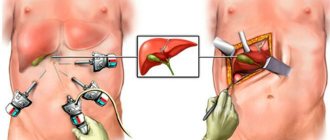
Amputation of this organ is scientifically called cholecystectomy. The bladder is amputated in two ways: using laparotomy - abdominal surgery with a full incision of the skin, muscles of the peritoneal wall and laparoscopy - a gentle minimally invasive intervention.
In many ways, if the operation was performed efficiently and correctly, the pain (their severity and duration) will depend on the method by which the organ was removed.
If you have undergone abdominal surgery, the recovery can be quite long. And some patients who have problems with tissue regeneration and wound healing may experience pain in the incision area for three years and three years later. If, after endoscopic removal surgery, the puncture incisions hurt in the postoperative period during the first two to three days and are relieved with painkillers, this is considered normal. Long-lasting pain and cramping in the peritoneum may be signs of various types of postoperative complications.
What can be evidenced by ongoing and intractable pain after amputation of the gallbladder? With the removal of the organ, cholecystitis, the inflammatory process, or even the remaining hard tumors, stones in the ducts did not completely go away, and the surgeon who performed the operation did not clear them. Most likely, in this case, repeated intervention will be required.
If the liver hurts, this may be due to stagnation of bile in it due to cholestasis syndrome. Perhaps the pain will go away when the functions of the gallbladder are redistributed among all other systems, and the flow of bile without entering the gallbladder is adjusted. However, sometimes with these symptoms it is worth helping the body: taking bile-thinning and choleretic drugs so that the bile leaves the liver flows on its own.
Continuous intestinal pain - these symptoms may be markers of damage to the intestinal mucosa due to the uncontrolled flow of bile there.
Symptoms accompanying pain
If the pain is not associated with tissue incisions made by surgeons to perform surgery to amputate the gallbladder, then the pain is usually accompanied by other unpleasant symptoms that worsen the quality of life. The pain from the incision site passes into the navel - this is how the inflammatory process in the abdominal cavity manifests itself, caused by leakage of bile into the peritoneum or infection introduced during the operation . Usually all this is accompanied by an increase in the patient’s body temperature to critical levels.
Lower back pain or severe back pain in general - these signs may indicate a malfunction in the functionality of the sphincter of Oddi. The sphincter of Oddi is a kind of “border post” that controls the release of bile into the duodenum. This system is a special muscle ring. When everything is in order and there are no failures in the system, the muscle tone is good, and they relax solely on a special command. If a “breakdown” occurs, the muscles weaken and bile is released randomly. And along with it, all sorts of unnecessary substances and bacteria enter the intestines. This provokes discomfort and pain in the back and lower back.
Also causing back pain may be inflammatory processes in the peritoneum caused by postcholicectomy syndrome. Which, in turn, was provoked by inflammation in the bile ducts, stones remaining in the ducts or injuries caused by the duct during surgery by an inexperienced surgeon. If the lower abdomen hurts, this also indicates some kind of inflammatory process, most likely associated with the intestines. There is a cut on the left side under the ribs, perhaps the inflammation has spread to the spleen.
Chronic cholecystitis and cholelithiasis in pregnant women
Diseases of the biliary system occupy one of the leading places among diseases of the digestive system. They occur in people of any age, but are especially common in young people, with women 4-7 times more likely than men
.
Often, chronic diseases of the gallbladder and bile ducts first begin in women during pregnancy. For example, pregnancy is considered one of the risk factors for developing gallstones
.
Chronic cholecystitis
Chronic cholecystitis
is a chronic relapsing disease associated with the presence of inflammatory changes in the wall of the gallbladder. Two factors play a fundamental role in its development: infection and bile stagnation caused by dyskinetic disorders. The latter, as a rule, cause the clinical manifestations of the disease.
Dyskinesias of the gallbladder and biliary tract are based on disturbances in their motor activity caused by disorders of neurohumoral regulation. There are two types of dyskinesia: hyper- and hypomotor, which have certain differences.
Pregnant women are characterized by hypomotor disorders, since the main hormone predominant in the second half of pregnancy is progesterone, which relaxes all smooth muscle organs (the main physiological meaning of its action in the pregnant woman’s body is relaxation of the uterus, preventing premature birth and miscarriage). Hypomotor dyskinesia is based on insufficient, weak emptying of the gallbladder. It is motor disorders that determine the clinical manifestations of chronic cholecystitis in pregnant women, and not inflammation.
Usually a woman is bothered by pain in the right hypochondrium
. Depending on the type of dyskinesia, dull aching pain, a feeling of heaviness in the right hypochondrium (with concomitant hypomotor dyskinesia), or, conversely, sharp, cramping pain (with hypermotor dyskinesia) prevail. The pain may be accompanied by dyspeptic symptoms: a feeling of bitterness in the mouth, nausea, vomiting, belching of air, heartburn, bloating. An increase or appearance of pain has been noticed after errors in the diet.
Our own long-term experience of monitoring pregnant women has shown that approximately 1/4 of women suffering from cholecystitis associate the appearance or intensification of pain in the right hypochondrium with fetal movements and its position in the uterus. Sometimes a woman is bothered by a burning sensation of the skin in the area of the right hypochondrium, under the right shoulder blade - these are the so-called zones of skin hyperesthesia (increased sensitivity) of Zakharyin-Ged. You should not be afraid of this unpleasant sensation, since it is a “continuation” of pain, and not the result of the addition of any new disease or complication.
In the diagnosis of gallbladder diseases, the leading role today belongs to ultrasound examination, during which the specialist makes a conclusion about the nature of the detected disorders, the possible presence or absence of stones.
Pregnancy often worsens the course of pre-existing cholecystitis; exacerbation of the disease occurs in half of the cases, most of them in the third trimester. And in the clinical picture of exacerbation, symptoms of hypomotor dyskinesia prevail. Chronic cholecystitis, in turn, affects the course of pregnancy. Often there are painful nausea, toxicosis - vomiting of pregnant women, and a little less often - drooling. Moreover, early toxicosis drags on until 16–20, and sometimes 28–29 weeks of pregnancy.
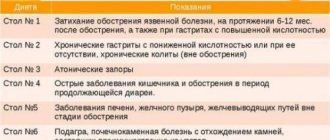
The principles of treatment of chronic cholecystitis in pregnant women are the same as in non-pregnant women. Diet therapy (table No. 5) is carried out without too restrictions while maintaining the optimal (for each stage of pregnancy) ratios between proteins, fats and carbohydrates. Restrictions apply to refractory fats, rough foods, exclude spices, pickles, marinades, fried foods, and smoked foods. Food is taken in fractional portions at least 5 – 6 times a day. With concomitant hypomotor dyskinesia of the gallbladder, the diet includes “cholecystokinetic” products, that is, those that promote contraction of the gallbladder: weak meat or fish broths, soups, cream, sour cream, soft-boiled eggs. It is useful to include foods rich in lipotropic substances (cottage cheese, egg white omelet, cod).
Drinking mineral waters such as Essentuka No. 4 and No. 17, Smirnovskaya, Slavyanovskaya, sulfate Narzan has a positive therapeutic effect during the absence of attacks of cholecystitis and edema. Mineral water is consumed 200 ml warm 3 times a day 1 - 1.5 hours before meals for 14 - 21 days. In the 3rd trimester, when it is desirable to reduce the amount of fluid you drink, treatment with mineral waters is not indicated.
All pregnant women without exception suffering from chronic cholecystitis are recommended to use choleretic drugs
. First of all, sorbitol or xylitol should be mentioned, which are used in the form of a 10–15% solution of 50–70 ml 30 minutes before meals 2–3 times a day. Having a laxative effect, they can benefit a pregnant woman in this regard. It is most advisable to take herbal preparations in the form of decoctions prepared independently. The easiest way is to brew tea at the rate of 1 tablespoon of plant materials (immortelle flowers, corn silk, peppermint leaves, dill seeds, rose hips, barberry root, separately or in a 1:1 mixture) per 1 cup of boiling water. After straining, take 1/3 cups warm 30 minutes before meals 3 times a day. Especially in the second half of pregnancy, when it is necessary to strictly take into account the amount of fluid consumed, it is convenient to use Flamin (extract of immortelle sandy) 1 - 2 tablets 3 times a day 30 minutes before meals. When prescribing a decoction of a mixture of choleretic herbs, positive diuresis is also noted, since they have a sufficient diuretic effect.
To combat stagnation of bile, after consulting with your doctor, you can carry out “blind” probing or tubage with vegetable oil (30 - 40 ml of corn or olive oil), Carlsbad salt or Barbara salt (1 teaspoon per glass of water), mineral water ( 500 ml warm, in the absence of swelling) To carry out tubage in the morning on an empty stomach, you need to drink the above mentioned remedies, lie down in a warm bed on your right side for 1.5 - 2 hours. It is not necessary to use a heating pad for a pregnant woman.
For acute pain in the right hypochondrium, you can take noshpa, baralgin
.
Cholelithiasis
Cholelithiasis
(cholelithiasis, calculous cholecystitis) is a disease characterized by the formation of gallstones in the bile ducts or gallbladder. Many scientists are of the opinion that it is pregnancy that contributes to the formation of stones and the development of the disease.
Without an exacerbation, gallstone disease can manifest itself as a feeling of heaviness in the right hypochondrium, a number of dyspeptic symptoms (nausea, bitterness in the mouth, etc.). However, in exacerbation, that is, with the development of biliary colic, another name for hepatic colic, the disease has clear clinical symptoms, depending on the location of the stones, their size, and the activity of the concomitant infection. Typically, colic develops in the late evening or at night, usually after errors in the diet, as a result of experiences caused by negative emotions (usually emotions of anger). A bumpy ride the day before and intense movements of the fetus can also trigger colic. A painful attack in the right hypochondrium, but can be in the epigastrium and even the left hypochondrium, is intense, the pain radiates (“gives”) to the right shoulder, shoulder blade, neck, lasts from 15 – 40 minutes to 12 hours, if no measures are taken.
Palpation of the area of the right hypochondrium causes sharp pain. The pain is accompanied by nausea, vomiting, bitterness in the mouth, heartburn, and bloating. If the common bile duct is blocked by a stone, jaundice may occur.
as in acute viral hepatitis, dark urine,
discolored feces
.
Pregnancy promotes the manifestation of latent cholelithiasis. That is, in women with cholelithiasis, the appearance of clinical signs of the disease is not uncommon. Quite often in this group of patients, the onset of pregnancy is accompanied by early toxicosis - vomiting of pregnant women. Exacerbation of the disease most often occurs in the second trimester of pregnancy.
Treatment of cholelithiasis is in many ways similar to that for cholecystitis (therapeutic nutrition, mild choleretic agents). If pain occurs, it is permissible to take painkillers and antispasmodics (baralgin, noshpa, papaverine hydrochloride, analgin). If the pain does not subside within an hour, the woman should consult a doctor (call an ambulance) for more intensive treatment measures.
In recent years, drugs that promote the dissolution of stones (cheno- and ursodeoxycholic acids) have been used to treat cholelithiasis, but pregnant women are strictly prohibited from carrying out this type of therapy (the negative effect of these drugs on the formation of the fetus has been proven), as well as the crushing of stones (shock wave lithotripsy). If absolutely necessary during pregnancy, surgical treatment can be performed - cholecystectomy (removal of the gallbladder).
Pregnancy after gallbladder removal
In the last two decades, in parallel with the increase in the number of patients with chronic cholelithiasis, the number of cholecystectomies has been steadily increasing throughout the world. Surgeries on the gallbladder are becoming the most common intervention on the abdominal organs after appendectomy. In approximately 80–90% of patients, cholecystectomy does not cause noticeable disturbances in the body. However, during pregnancy, digestive system disorders can occur and a woman should be prepared for this (however, the fear that a “liver rupture” will occur is not justified).
In some patients, after surgical treatment for cholelithiasis, the so-called postcholecystectomy syndrome develops. It is manifested by pain in the right hypochondrium, dyspeptic complaints (nausea, bitterness in the mouth, heartburn, etc.), it seems that the disease has returned again. Therefore, all pregnant women who have undergone cholecystectomy in the past must be monitored by a antenatal clinic physician and take preventive measures aimed at preventing the development of possible complications. They should follow a diet
(5 – 6 times a day, in fractional portions) and a diet like table 5. Taking choleretic drugs (for example, Flamin) and performing “blind” tubes are indicated.
Make an appointment with specialists by calling a single call center:
+7(495)636-29-46 (metro stations “Schukinskaya” and “Street 1905 Goda”). You can also make an appointment with a doctor on our website, we will call you back!
Diagnosis and identification of causes
If all the symptoms described above do not give the patient peace of mind due to the removal of the gastric assistant - the gallbladder, then the patient needs an urgent examination. A person with such complaints is prescribed an ultrasound and x-ray examination of the peritoneum with an emphasis on the place where the amputated organ was located, the liver, ducts, intestines or other area that bothers the operated area.
also prescribed to have urine and sometimes feces analyzed to find out if there is bile there.
Based on research, they find out the cause of the uncomfortable postoperative period and show measures that should save the patient from suffering. Sometimes you can get by with therapy, and in some cases the patient is sent back to the operating table.
Drug treatment
How can you get rid of pain after gallstone removal and eliminate other unpleasant symptoms? Naturally, carefully and thoroughly following the doctors' instructions. Cuts at the site of tissue excision, if there are no other pathologies, are relieved with pain relievers. Stagnant biliary phenomena can be removed with bile-liquefying and bile-expelling drugs, inflammatory processes can be removed with anti-inflammatory drugs.
If the patient takes the medications as prescribed, his condition will soon stabilize, and the quality of life will be equal to that of people who have not survived amputation of the gallbladder.
Diet and prevention
Of course, after amputation of the gallbladder, you will not be able to eat almost anything for the first time in the postoperative period. Later, along with water, they will be allowed to eat pureed soups with vegetables, lean fish or chicken . Also, along with these food products, you can eat porridge with water. Ideally, the patient will need to adhere to the so-called diet No. 5 for up to six months after organ amputation.
Particular attention will need to be paid to the amount of food, this is most important in the first time after surgery. The fact is that bile, which does not have “sludge” in the gallbladder due to its absence, is less concentrated and is able to cope with only a small amount of food when processing food. So portions should be minimal, and the number of meals increased to five or even six.
Allowed and prohibited foods for bloating
There are a number of products that increase gas formation. These include rye and wheat bread, especially fresh bread. Also, you should not eat pearl barley, semolina, or millet. Prohibited are fatty meats, sweet products (honey is allowed), whole milk, even diluted powdered milk. Soda, alcohol and all types of pasta, even hard varieties, are prohibited.
Among vegetables, all types of cabbage (cauliflower, Brussels sprouts, cabbage, broccoli), corn and potatoes, raw onions, radishes and radishes, spinach and peppers, artichokes and fresh asparagus shoots cause severe flatulence. Fruits that cause bloating are apples and pears, peaches and grapes, gooseberries and cherries, dates and figs, and prunes.
Nutritionists say that a number of products are strictly prohibited from being combined with each other, since their interaction can cause the accumulation of gases in the intestinal tract. It is best not to mix milk and grain products, berries and fruits with a sour taste, fresh vegetables and fruits. Experts do not recommend serving a side dish of potatoes with meat dishes.
You can eat quite a wide variety of permitted foods. In particular, cheeses, cottage cheese, any cereals except prohibited ones (rice, buckwheat), eggs in the form of omelets or soft-boiled. Vegetables can be cooked stewed or batched, in the form of soufflés or casseroles, and dishes can be made from lean meat. For drinks, you can drink juices from berries and fruits. Salads and cereals should be seasoned with butter or vegetable oil, olive oil or flaxseed oil. Bread must be eaten dried or yesterday's bread.
YouTube responded with an error: The request cannot be completed because you have exceeded your quota.
Video
Why does my stomach hurt?
The gallbladder was removed on January 31, 2018; the gallbladder was severely inflamed. Every day there is pain in the right hypochondrium and in the left after eating. what to do? The surgeon who performed the operation says that it is necessary to check the stomach
The Ask a Doctor service offers an online consultation with a gastroenterologist on any problem that concerns you. Expert doctors provide consultations around the clock and free of charge. Ask your question and get an answer immediately!
In medical circles, surgery to remove the gallbladder is called cholecystectomy. There are two main methods of performing it - laparoscopy (abdominal surgery) and laparotomy (abdominal surgery). And although laparoscopy and laparotomy are recognized as relatively safe methods of treating cholelithiasis, cholecystitis and cholesterosis, any method of performing the operation cannot protect the patient from complications and postcholecystectomy syndrome that appears in the postoperative period.
Diarrhea
After surgery, the digestive process malfunctions and problems with the intestinal tract occur. This is especially true for surgery to remove the gallbladder, the treatment of the consequences of which requires an integrated approach. This organ is important for the biliary system, since in its absence hypersecretion of bile occurs. Many patients complain of bloating after gallbladder removal, flatulence and diarrhea. A fifth of all patients experience diarrhea with blood clots, intestinal disorders, and fever. As a rule, all these phenomena disappear by discharge, this is influenced by medications and dietary nutrition. Clinical practice calls these symptoms hologenic diarrhea.
Read also: How to treat suspension in the gallbladder?
Symptoms of hologenic disorder include the following:
| № | Helpful information |
| 1 | diarrhea |
| 2 | discolored stool or green clumps in stool due to bile secretion |
| 3 | pain in the right half of the peritoneum and in the iliac region |
| 4 | chronic diarrhea |
Unformed stools and frequent hologenic diarrhea provoke obstructive jaundice and dehydration. Experts note the development of vomiting. To eliminate these symptoms, it is necessary to treat with enzyme-containing drugs, drink plenty of fluids, and follow a diet with anti-diarrhea products.
What is postcholecystectomy syndrome?
Despite the fact that surgeons call cholecystectomy one of the simplest operations in medical practice, it is associated with the loss of one of the human organs - the gallbladder. And although such an operation allows patients to forget about problems associated with the gallbladder, after it is performed in the human body, there is a violation of the outflow of bile, a malfunction of the digestive system and liver. As a result of such changes, the patient may experience the so-called postcholecystectomy syndrome, which is usually accompanied by pain in the right hypochondrium and abdomen.
Depending on the location of pain after surgery to remove the gallbladder, it can be divided into the following types:
- pancreatic - predominantly localized in the left hypochondrium and back;
- biliary – most often occur in the upper abdomen (in the stomach area) and spread to the right shoulder blade;
- bile-pancreatic - have a girdling character.
Other symptoms of postcholecystectomy syndrome are:
- diarrhea;
- flatulence;
- bitterness in the mouth;
- nausea and vomiting;
- weakness;
- jaundice;
- belching;
- decreased performance.
What are the consequences of gallbladder removal?
A successful operation requires monitoring the condition of the patient, who spends the first hours in intensive care. Specialists monitor his feelings after anesthesia. On average, the patient is discharged on the third day, but if complications arise, they may remain in the hospital. The wound becomes dark in color, with the release of watery clots, and a lump may appear in the area of compaction. Only slight redness of the skin at the site where the incision was made is considered normal.
There are many consequences that occur when there is a failure in the release of bile and a change in its composition:
- impaired motility in the muscles of the duodenum;
- too low bile concentration;
- the occurrence of expansion in the bile canal;
- impaired pathogen defense;
- failure of microflora in the intestinal tract;
- accumulation of serous fluid in the place where the gallbladder was;
Gallbladder removal
- the occurrence of severe bloating, flatulence and defecation disorders;
- the appearance of belching, often with air;
- development of pain syndrome;
- lack of movement of masses in the digestive tract;
- problems with the digestive process;
- impaired absorption of bile.
All these symptoms in clinical practice are called postcholecystectomy syndrome, which is most pronounced during abdominal surgery. The composition of the bile does not change, since the gallbladder with the stones inside has been removed. The toxic liquid released irritates the mucous membranes in the intestinal tract, and accumulation occurs in the common bile duct. In cases where the common bile duct is damaged, pain, diarrhea, and flatulence may occur.
Why does pain occur after cholecystectomy?
Disorders of the sphincter of Oddi
Answering the question why, after removal of the gallbladder, the right side, stomach, intestines or back hurts, experts in this field note that most often this occurs due to disruption of the sphincter of Oddi - a special muscle formation that controls the flow of bile and gastric juice into the stomach. duodenum. As a result of a decrease in the tone of the sphincter of Oddi, not only bile, but also pathogens enter the intestines and bile ducts. This leads to inflammatory processes.
Damage to the extrahepatic bile ducts
According to many studies, after removal of the diseased organ, there is an increase in the volume of the common bile duct and inflammation of the bile ducts. Most often, this situation occurs due to injury to the bile ducts during surgery or disruption of the drainage process in the postoperative period.
Also, alarming symptoms may occur against the background of the formation of a common bile duct cyst or as a result of a long stump of the bile duct.
However, the most dangerous cause of pain that appears after cholecystectomy is inflammation of the bile ducts (cholangitis), which develops as a result of impaired outflow of bile, its stagnation and the spread of infection along the bile ducts.
Liver diseases
Patients often ask why their liver hurts after gallbladder removal. Typically, pain in the area where the liver is located is associated with a violation of its basic functions. If an inflammatory process occurs in the liver, along with unpleasant and painful sensations in the right hypochondrium, the patient has back pain, lower back pain, and also feels discomfort in the spine. One of the most common causes of such ailments can be fatty hepatosis, which in the postoperative period develops in 42% of patients after cholecystectomy.
Another cause of pain in the liver can be cholelithiasis. Even if the diseased organ is removed, stones may remain in the liver and bile ducts. Small stones can easily pass out of the body along with feces, but large stones can cause blockage of the bile ducts, intestinal obstruction, sepsis, biliary pancreatitis and liver abscess.
Typically, a painful attack lasts 10-20 minutes, occurs after eating or at night, and is accompanied by nausea and vomiting.
Diseases of the gastrointestinal tract
If a person has a stomach ache after removal of the gallbladder, this may be due to the development or exacerbation of concomitant diseases such as ulcers, gastritis or inflammation of the pancreas.
Signs of postcholecystectomy syndrome can also occur against the background of impaired bile passage. After removal of the gallbladder, the main reservoir for bile, it begins to flow uncontrollably into the intestines. As a result of changes in the composition of bile, the body's ability to dissolve bacteria is reduced, intestinal microflora and the metabolism of bile acids are disrupted.
Other causes of pain that occurs after cholecystectomy in the back, abdomen or side may include:
- damage to the intestinal mucosa, small and large intestine;
- an increase in the amount of liver enzymes in the blood;
- damage to neighboring organs during surgery;
- violation of the prescribed regime.
Severe pain may occur due to surgical complications. First of all, we are talking about the formation of postoperative adhesions and scars on the bile ducts.
Pain and dyspepsia after cholecystectomy
Over the past few decades, gallstone disease (GSD) has become one of the most frequently reported organic human diseases, reaching a prevalence of 10-15% in industrialized countries (in the adult population). This explains the large number of planned and emergency surgical interventions for cholelithiasis worldwide [2, 33]. In the United States alone, about 1 million new cases of cholelithiasis are diagnosed annually, and the cost of treating this disease exceeds $6 billion per year [16]. In Russia, about 200 thousand cholecystectomies are performed annually, mostly laparoscopically [1].
On average, only 20% of patients with cholelithiasis have a symptomatic course, which includes classic biliary colic [36]. With this course of cholelithiasis, surgical intervention can achieve symptom relief in 53.0-81.5% of patients [25, 32, 38], and reduce the severity of dyspepsia and abdominal pain in 56% and 72% of cases, respectively [12]. Unfortunately, a very significant proportion of patients (about 40%) do not note resolution of abdominal pain and symptoms of dyspepsia after cholecystectomy; moreover, in 12.0-38.6% of all cases of cholecystectomy, painful symptoms first appear after surgical treatment [27, 38 ]. In general, abdominal pain and dyspepsia after cholecystectomy are recorded in a wide frequency range (from 5.6% to 57.3%), which is determined by differences in study design [21, 28, 30, 41, 42]. Thus, up to half of patients at different times from the moment of cholecystectomy complain of abdominal pain, symptoms of gastric and intestinal dyspepsia, which can have both organic and functional causes [2, 16].
POSTCHOLECYSTECTOMIC SYNDROME
Definition and brief excursion into history
It should be noted that postcholecystectomy syndrome (PCES) is only at first glance a simple problem; the difficulties of understanding this syndrome begin with its definition [2].
The first works that one way or another describe pathological conditions after removal of the gallbladder appeared in foreign literature in the late 30s of the last century [19, 23, 31]. The most important and interesting remains the first series of observations presented by J. Hellstrom (taking into account data obtained by KK Nygaard) in 1938. It consisted of 141 patients after removal of the gallbladder, 30% of the total sample had cramping abdominal pain similar to those were before surgery. Only 9 patients were diagnosed with choledocholithiasis; acute pancreatitis was diagnosed even less often. In most cases, the causes of pain could not be explained, and therefore the author called the identified pain “postcholecystectomy colic” [23].
The next largest series of observations was presented by H. Doubilet in an oral report at a meeting of the surgical section of the New York Academy of Medicine in April 1943 [17] and detailed in a subsequent review by R. Colp [15]. The cited series included 253 patients after cholecystectomy with follow-up periods ranging from 1 to 7 years. 40% of patients had persistent postoperative symptoms, often similar to clinical manifestations before cholecystectomy. It was in these two works [15, 17] that the term PCES was first used, within which the authors combined a complex of various disorders after cholecystectomy. Most of the postcholecystectomy disorders, due to the absence of organic causes (cystic duct stump, residual choledocholithiasis, etc.), are recognized by researchers of those years as functional disorders, accompanied by recurrent colic-type pain. The authors suggested that the basis of frequently recorded functional pain is a spastic type of motor disorder (dyskinesia) of the sphincters of the biliary tract and intestines, as well as borderline mental disorders in some patients. One of the compelling reasons for such a judgment was the statement of a higher incidence of postcholecystectomy functional disorders in patients with a potentially functioning gallbladder (acalculous cholecystitis or calculous cholecystitis without pronounced fibrosis of the gallbladder wall) [15, 17]. Thus, for the first time in history, the authors outlined clear ideas about the possibility of the formation of postcholecystectomy disorders and identified potential groups of signs that increase the risk of their development:
- the presence of functional causes of pain and dyspepsia before cholecystectomy;
- borderline mental disorders in patients before surgery;
- the presence of a functioning gallbladder.
Taking into account the experience and knowledge accumulated to date [4, 8, 9], we can assume that:
- functional diseases, manifested by complaints of pain and dyspepsia before cholecystectomy, may persist or worsen after surgery;
- borderline mental disorders in patients with functional gastrointestinal diseases are extremely common, closely intertwined in the general pathogenesis of somatoform disease; therefore, borderline mental disorders before surgery for cholelithiasis (which can be combined, for example, with irritable bowel syndrome - IBS) will definitely persist after, forming persistent or even progressive functional symptoms of pain and dyspepsia;
- removal of a functioning gallbladder (calculous acute cholecystitis, stage I cholelithiasis with biliary sludge, solitary stones in young people) may increase the risk of maladaptive functional disorders in the postoperative period relative to that in persons operated on under other conditions (non-functioning, “disconnected” gallbladder, etc.) . P.).
Returning to the first works that formed the idea of PCES, it should be noted that the hypothesis of spasm of the biliary tract sphincters as the cause of functional pain after cholecystectomy formed the basis for the empirical use of nitrates and atropine to relieve spasm [15]. A number of simple descriptive studies of those years made it possible to develop indications and even discuss the theoretical possibilities of papillotomy, based on experimental work from the beginning of the last century.
In the 1940-1970s, the term PCES was firmly established and regularly appeared in the scientific literature [14, 34, 37, 39, 40], by the mid-1970s the number of such works reached one hundred [2]. It is curious that one of the first domestic works reviewed in international databases [10] demonstrated a skeptical attitude towards the term PCES and contained its active criticism. What’s even more interesting is that since the late 60s of the last century, the number of English-language articles on the topic of PCES in the most authoritative international journals has been rapidly falling and by the 80s it has practically been reduced to zero, while in Eastern Europe and the USSR the number of works devoted to PCES, on the contrary, increases significantly. In the 1980s, due to the abandonment of the term PCES in authoritative English-language journals, it was successfully replaced by postcholecystectomy pain [13, 35], papillary dysfunction [11] and even, using the terminology of the 30s of the last century, biliary dyskinesia [26 ].
Today it is obvious that the complexity of studying and verifying postcholecystectomy disorders, the similarity of symptoms with organic changes and functional disorders have led to the fact that the term PCES ceased to be used in Western countries by the mid-80s of the 20th century. In international practice, there is still no unified term PCES, since it is incredibly difficult to determine the exact mechanism and root cause of pain and dyspepsia that occur at different time periods after cholecystectomy. However, paradoxically, the term PCES was included in ICD-10 and was extremely popular in the USSR, and now in Russia (both in routine practice and among scientists). The wide recognition of this term in the 1970-1980s in the USSR was not accidental; it was explained by the growing number of cholecystectomies, objective diagnostic difficulties and insufficient understanding of doctors about the possible consequences of intervention - from functional maladaptation of the biliary tract (and even the entire digestive system) to gross organic changes [2].
In Russia today, PCES refers to many different diseases and conditions that arise in patients after cholecystectomy and theoretically can be associated with it [2]. It was the impossibility of combining organic changes and functional disorders with a single diagnosis that led to the abandonment of this term abroad, where any abnormalities in a patient after cholecystectomy, theoretically associated with it, are considered as a “condition after cholecystectomy” [24, 29]. According to clinical indications in risk groups and in the presence of markers of organic changes, a diagnostic search for the cause is carried out, otherwise a diagnosis of sphincter of Oddi dysfunction is established according to the Rome III criteria [18].
Structure of postcholecystectomy syndrome
An objective understanding of the structure of nosologies that are the causes of pain and dyspepsia after cholecystectomy allows us to formulate the results of recent clinical studies. In one study, 80 patients with symptoms of pain and dyspepsia after gallbladder removal were monitored for 36 months. A comprehensive examination using biochemical tests (bilirubin and alkaline phosphatase), transabdominal and endoscopic ultrasound, endoscopic retrograde cholangiopancreatography and sphincter of Oddi manometry allowed the authors to accurately determine the causes of pain and dyspepsia in patients after cholecystectomy. In addition to functional disorders, they included a wide range of organic diseases of the hepatopancreatobiliary zone. The majority (57.5%) of patients had organic pathology of the biliopancreatic zone (Fig.). At the same time, dysfunction of the sphincter of Oddi and a complex of functional non-biliary causes (including IBS) accounted for a fairly large proportion - 42.5% of all cases (8.75% and 33.75%, respectively) [20].
Rice. Causes of pain and dyspepsia in patients with cholecystectomy, %. Research Center for Gastroenterology and Hepatology, Institute of Medicine and Pharmacy, Craiova, Romania (after [20])
In a study conducted in the UK to assess the incidence of diarrhea in 100 patients followed for 6-12 months after cholecystectomy, in 17% of them this symptom appeared for the first time and became persistent only after surgery. The authors identified young age as the most significant risk factor for diarrhea after cholecystectomy (OR: 3.4; 95% CI: 1.16–9.96; p = 0.026) [22]. Of course, it is in young and middle-aged patients that functional gastrointestinal disorders, including IBS, are most common [8]. One of the reasons for functional disorders of the intestine after cholecystectomy is the malabsorption of bile acids and the development of secretory diarrhea due to excessive and asynchronous entry of unconcentrated bile into the lumen of the intestinal tube. The pathophysiology of secretory diarrhea is also based on the accelerated passage of contents through the small and large intestines, accompanied by hypermotility of intestinal smooth muscles. Hypermotility and spasm with the appearance of pain are very similar conditions in pathophysiological terms. Visceral hypersensitivity, spasm (pain) and diarrhea form IBS-like symptoms in some patients after cholecystectomy. The psychosomatic background in some of these patients is a risk factor for the persistence of symptoms [2].
It is important to note another study that included 158 patients scheduled for laparoscopic cholecystectomy. The authors assessed quality of life and checked for the presence of IBS before and after surgery using criteria for IBS (Manning criteria and Rome II criteria) and the Gastrointestinal Quality of Life (GQL) questionnaire, respectively. As it turned out, 32 (20.3%) patients had IBS before cholecystectomy [24], i.e., somewhat more often than in the general population (10-17%) [8]. Observation of patients in the general sample at 6, 12 weeks and 2 years after surgical treatment showed that cholecystectomy generally improves the quality of life of patients in the early recovery period after surgery. Thus, the average GQL score 6 weeks after surgery increased significantly: from 88.8 ± 1.3 to 105.5 ± 1.3 (p < 0.001). A similar picture persisted after 3 months. However, 2 years after surgery, the authors noted a significant deterioration in the quality of life of patients: on average 7.6 ± 2.3 points lower than the values before surgery (p = 0.003). This probably happened precisely due to the development in some patients of certain deviations, which can be designated as PCES. It is important that in people who suffered from IBS before cholecystectomy, the quality of life worsened already by the 6th week after surgery, probably due to the worsening of IBS symptoms. In such patients, the presence of each Manning symptom reduced the quality of life by 5.2 ± 1.3 points compared with the main group without IBS (p < 0.001). When using the more modern Rome II criteria, it turned out that in people with IBS, the quality of life decreases more pronouncedly - by an average of 12 points compared to the general group of patients [24].
Not surprisingly, one of the largest studies to date, conducted at the Mayo Clinic (Rochester, Minnesota) and Kaiser Permanente (San Diego, California) and including 1008 patients who underwent cholecystectomy for cholelithiasis, identified significant factors for the absence of abdominal pain after surgery (p < 0.05) [38]:
- rare frequency of pain attacks (once a month or less);
- manifestation of pain in the period 1 year or less before cholecystectomy;
- duration of pain attack from 30 minutes to 24 hours;
- night pain;
- high intensity pain.
As can be seen from the factors presented above, they do not at all correspond to the signs of functional disorders, which are characterized by long-term non-progressive persistence of pain, frequent short-term attacks or prolonged multi-day periods of moderate pain bordering on discomfort, absence of pain at night [7, 8, 18 ]. Moreover, the authors of the work cited above [38] noted that the risk of persistent pain after cholecystectomy may increase in somatized patients, in those with lower abdominal pain, recurrent bloating, and other markers of IBS.
Thus, if a patient had IBS before surgery, it is quite possible that it will persist and even worsen after surgery. It is in such a patient that we can most likely expect repeat visits to the surgeon and gastroenterologist after surgery with persistent complaints of abdominal pain and symptoms of dyspepsia, bowel disorders and deterioration in quality of life [2]. Extrapolating from these data, it can be assumed that cholecystectomy in patients with cholelithiasis, combined not only with IBS, but also with other functional gastrointestinal disorders, may have a worse prognosis in terms of persistent pain and dyspepsia than in patients who suffer only with cholelithiasis.
Pathophysiology of postcholecystectomy disorders
Based on the many organic and functional causes of pain and dyspepsia after cholecystectomy, it is necessary to distinguish organic and functional causes in the pathophysiology of postcholecystectomy disorders [2].
1. Organic reasons:
- pain, dyspepsia and other symptoms caused by organic pathology associated with cholelithiasis and/or cholecystectomy (cystic duct stump, choledocholithiasis, acute biliary pancreatitis, stricture of the common bile duct and major duodenal papilla, etc.) [5];
- clinical manifestations of another organic pathology, theoretically not related to cholecystectomy (de novo tumors of the digestive organs).
2. Functional reasons:
- dysfunction (spasm) of the sphincter of Oddi, which occurred initially or appeared/worsened after cholecystectomy (the so-called true PCES);
- digestive disorders due to changes in the properties and secretion of bile, called “biliary insufficiency.” Although this term is not yet generally accepted, the deficiency of the effects of bile and the asynchronism of its secretion can contribute to the development of various pathological conditions that determine the clinical picture of postcholecystectomy disorders: exocrine pancreatic insufficiency, duodenogastric reflux, small intestinal bacterial overgrowth syndrome (SIBO), etc. [ 3, 4, 6];
- other functional disorders of the digestive system (IBS, functional dyspepsia, gastroesophageal reflux disease).
To present the pathophysiology of postcholecystectomy disorders, we should dwell on the functions of the gallbladder (prolapsed after cholecystectomy) [1, 2]:
- the evacuation function ensures the release of bile into the duodenum (duodenum) during the digestive period;
- concentration and reservoir promote the accumulation of concentrated bile, which has the best digestive and bactericidal effects;
- absorption (absorption of individual components of bile) underlies the compensatory reaction when they are in excess;
- secretory (secretion of mucus by the glands of the cervical region) facilitates the flow of bile into the gallbladder and the evacuation of bile from it;
- the hormonal function is the secretion of anticholecystokinin, which has a modulating effect on the sphincter of Oddi.
- The sphincter of Oddi also performs important functions related to the functioning of the gallbladder [2]:
- regulates the outflow of bile and pancreatic juice into the duodenum;
- prevents reflux of duodenal contents into the common bile duct and main pancreatic duct;
- ensures the accumulation of bile in the gallbladder during the period between meals (as it is able to overcome the secretory pressure of the liver);
- carries out synchronous work with the gallbladder.
So, the loss of the gallbladder with the loss of its functions and the resulting development of dysfunction of the sphincter of Oddi leads to a decrease in the quality and quantity of flowing bile and pancreatic secretion in the duodenum, which cannot always be fully compensated by the work of the physiologically associated digestive organs. In this regard, real conditions for digestive dysfunction are created. The pathogenesis of PCES is partly due to loss of gallbladder functions: the lack of evacuation and concentration functions determines the disruption of lipolysis processes in the small intestine and the weakening of the bactericidal properties of bile. Continuous bile leakage can also determine digestive dysfunction, contribute to the formation of biliary reflux and the development of hypertonicity of the sphincter of Oddi [1, 2, 5, 9].
Under the influence of altered small intestinal microbiota, bile acids are deconjugated with subsequent damage to the mucous membrane, the development of duodenitis, reflux gastritis and esophagitis. In some cases, duodenitis is accompanied by duodenal hypertension and duodenal dyskinesia, which contributes to the persistence of pathological refluxes [2, 5].
Clinical picture of postcholecystectomy syndrome
Pain after cholecystectomy, being the main reason for the low quality of life of patients, comes from the multifaceted pathophysiology of postcholecystectomy disorders presented above. The main cause of abdominal pain is the functional restructuring of the sphincter apparatus of the biliary tract after the loss of the gallbladder.
The Rome consensus of the III revision well presents the clinical picture of three types of sphincter of Oddi dysfunction after cholecystectomy: biliary, pancreatic and mixed [18]. With isolated dysfunction of the common bile duct sphincter, biliary pain occurs, localized in the epigastrium and/or right hypochondrium with possible irradiation to the back and right scapula. When the sphincter of the main pancreatic duct is predominantly affected, pain of the so-called pancreatic type is typical, localized in the epigastrium and left hypochondrium, sometimes radiating to the lumbar region and back. With spasm of the common sphincter, combined biliary-pancreatic pain is observed, often described as “girdling” [2, 9].
Management tactics and principles of treatment of patients with postcholecystectomy syndrome
The basis of approaches to the control of pain and dyspepsia after cholecystectomy is the timely and correct identification of their causes. The primary task is to exclude organic pathology of the digestive organs, which may be the cause of complaints - choledocholithiasis, biliary strictures, tumor diseases of the biliopancreatic zone, etc. The presence of such changes, as a rule, dictates the need for surgical or endoscopic treatment. In the absence of organic reasons for the persistence of symptoms, one should think about the functional nature of pain and dyspepsia, especially if there is an association with a number of indirect markers of functional pain [2]:
- the current symptoms existed before the operation, and in the postoperative period they appeared again, with the same or even greater severity;
- there is a long-term non-progressive course of the disease;
- known about mental disorders and/or use of psychotropic drugs before cholecystectomy;
- chronic complaints meet the criteria for functional disorders of the digestive system - functional dyspepsia, sphincter of Oddi dysfunction, IBS.
Statement of the fact of functional disorders of the digestive organs as the cause of pain and dyspepsia after cholecystectomy is an indication for conservative treatment. The basis for the selection of drugs for the correction of functional postcholecystectomy spasms and dyspeptic disorders is empirical, while most doctors prefer combination pharmacotherapy with the mandatory use of antispasmodic drugs. Additionally, medications may be prescribed to correct SIBO (intestinal antiseptics, dietary fiber, enterosorbents), duodenogastric reflux (prokinetics, ursodeoxycholic acid preparations, sorbents), modern microencapsulated pancreatin preparations for the correction of secondary pancreatic insufficiency, etc.
Unfortunately, there are no standardized pharmacotherapy regimens for PCES, which is explained by the frequent combination (so-called overlap) of various functional disorders in one patient, which can alternate over time, as well as the presence of optional, but often accompanying syndromes (SIBO, etc.) after cholecystectomy. It should be noted that in case of proven dysfunction of the sphincter of Oddi, resistant to adequate conservative treatment for 3 months, endoscopic intervention (endoscopic papillotomy and common bile duct stenting) is possible. Other cases of functional disorders after cholecystectomy require conservative treatment.
The choice of an antispasmodic in routine practice is also carried out empirically, since it is extremely difficult to verify the type of motor disorders and conduct pharmacological tests with different drugs. Comparative controlled studies assessing the effect of different antispasmodics on the function of the sphincter of Oddi have not yet been conducted. Due to the fact that due to the combination of functional disorders in the same patient it is quite difficult to separate complaints caused by dysfunction of the sphincter of Oddi, functional dyspepsia and duodenogastric reflux, IBS and SIBO, practicing doctors, as a rule, choose antispasmodics that can eliminate spasm as in the biliary tract and in the intestines, with a priority of prolonged action and with a minimum of adverse effects, which allows them to be used effectively and safely for a long time.
CONCLUSION
The term “postcholecystectomy syndrome” is extremely unfortunate; in modern English-language literature it is replaced by “post-cholecystectomy condition” due to a wide range of organic and functional reasons that determine the persistence of the main manifestations - abdominal pain and dyspepsia.
The risk of developing functional disorders after cholecystectomy is increased in individuals with initial borderline mental disorders and in young patients with a functioning gallbladder.
Only a comprehensive examination of patients using biochemical tests, transabdominal and endoscopic ultrasound and/or endoscopic retrograde cholangiopancreatography and manometry of the sphincter of Oddi allows us to determine in detail the cause of pain and dyspepsia in patients after cholecystectomy.
The basis for the selection of drugs for the correction of functional postcholecystectomy spasms and dyspeptic disorders is empirical, while most doctors prefer combination pharmacotherapy with the mandatory use of antispasmodic drugs. In case of proven dysfunction of the sphincter of Oddi, resistant to adequate conservative treatment for 3 months, endoscopic papillotomy and common bile duct stenting are possible.
Diagnostic methods
Before treating pain after cholecystectomy, it is necessary to find out the main cause of its occurrence.
The main diagnostic methods are:
- a chemical blood test that allows you to determine the level of liver enzymes and bilirubin, a special bile pigment;
- ultrasound examination, which can be used to assess the condition of the liver, stomach and intestines;
- radionuclide scanning of the hepatic and bile ducts;
- endoscopic retrograde cholangiopancreatography, which allows you to identify abnormalities in the hepatic and bile ducts;
- sphincter of Oddi manometry, which is necessary to measure the pressure in the sphincter;
- CT scan.
Methods of treatment and prevention
Depending on the cause of pain after removal of the diseased organ, the patient is prescribed drug therapy. In most cases, conservative treatment methods help eliminate pain after cholecystectomy.
To eliminate severe pain in the abdomen and lower back, the doctor prescribes painkillers and antispasmodics (Drotaverine, Bencyclane, Mebeverine). Nitroglycerin will help quickly relieve spasms. However, this drug must be used very carefully, since long-term use of nitroglycerin can negatively affect the cardiovascular system.
Patients may also be recommended special medications aimed at improving the outflow of bile, restoring the functions of the liver, intestines and digestive system organs. First of all, we are talking about choleretic drugs (Panzinorm forte, Allochol) and enzyme preparations (Creon, Pancitrate).
In case of inflammatory processes and the growth of pathogenic bacteria, it may be advisable to use antibiotics (Doxycycline, Intetrix, Furazolidone, Metronidazole). To restore the natural intestinal microflora, along with antibiotics, it is recommended to take probiotics and prebiotics (Hilak-Forte, Linex, etc.).
If the above medications are ineffective, patients are prescribed endoscopic papillosphincterotomy - a small operation that normalizes the outflow of bile and the flow of gastric juice into the duodenum, removes remaining stones in the ducts and thereby eliminates pain. Unlike conventional abdominal surgery, endoscopic papillosphincterotomy is performed using a papillotome, which the surgeon inserts into the major duodenal papilla and makes a bloodless tissue incision.
How does bloating feel?
Clinical manifestations of flatulence differ in their severity depending on the disease that provoked this disease.
The patient feels bloating as a combination of several conditions:
- distension of the abdomen and fullness of the stomach even with a small amount eaten;
- discomfort in the epigastric region;
- bloating of the intestines and abdomen;
- rumbling in the stomach (borborygms);
- increased gas volume, often escaping gases through the intestines (flatulence);
- nausea and vomiting;
- constipation and diarrhea, alternating and not going away;
- frequent belching of air;
- pain syndrome in the abdominal area.
It is during bloating that the volume of accumulated gases compresses and stretches the intestinal walls, causing irritation of parasympathetic type receptors. Through them, a signal goes to the axons in the spinal cord, which carry these impulses to the brain. The pain is felt not in the abdomen, but in the sternum. The symptoms are reminiscent of heart pain due to angina pectoris.
Experts distinguish pain during bloating from the abundance of gases under the diaphragm. A similar anomaly occurs in patients who wear tight underwear for too long or have problems with posture. Pain on the right in the lumbar region and under the ribs indicates a bend in the intestine between the liver and the diaphragm.
Read also: Symptoms and treatment of gallbladder bending
When should you see a doctor?
Many patients are convinced that if their back hurts after removal of a diseased organ, as well as liver colic and slight pain in the abdomen, this is not a reason for concern. However, in some cases, the patient may urgently need medical attention.
Urgent hospitalization is necessary if:
- pain that is localized in the abdomen, side or back does not go away for a long time;
- a person’s body temperature rapidly rises;
- a painful attack lasts more than 20 minutes;
- pain is accompanied by vomiting.
If people who have had cholecystectomy experience back, abdominal or side pain, it is important to remember that self-medication can be dangerous.
To avoid problems with the biliary tract and reduce the risk of pain, patients who have had their gallbladder removed will benefit from additional preventive measures, in particular, a special diet and split meals. In the postoperative period, which, depending on the complexity of the operation, can last from several months to a year, doctors recommend refraining from eating fatty, spicy and fried foods, and also eliminating spices, seasonings, coffee, alcohol and foods rich in essential oils (garlic) from the diet. , radish and onion).
The main food products in the next few years after cholecystectomy should be soups, boiled meat and fish, baked dishes, vegetables and fruits. If the pancreas is functioning normally, the diet can be supplemented with carbohydrates.
Only timely diagnosis and thorough examination of patients who have had their gallbladder removed will make it possible to quickly and accurately determine the true causes of pain and prescribe effective treatment to completely eliminate the pain syndrome.
How to treat bloating?
Flatulence is difficult to treat because it is caused by unconscious aerophagia. In some cases, there may be increased sensitivity to the amount of accumulated gases in the intestinal tract. To relieve aerophagia, you must not smoke or use chewing gum. With diseases of the upper stomach, increased production of saliva develops and, as a result, bloating. Antacids and soda are avoided if they cause belching. It is also necessary to avoid indigestible carbohydrates in foods. All fermented milk products are excluded from the diet if you are lactose intolerant.
Frequent belching should be confirmed before treating bloating. Relaxation therapy and biological feedback are used to change the cycle of discomfort and belching due to aerophagia. Any drugs are not effective.
Simethicone
Simethicone is a medicine that can break up small gas bubbles in cases where other anticholinergic drugs have not had the expected effect. For dyspepsia and postprandial fullness in the upper abdomen, there may be a noticeable effect from the use of antacids.
Activated carbon
Activated charcoal can reduce the amount of gas produced and odor, but its use can stain clothes and mucous membranes in the mouth, so patients are not very fond of taking it. Chlorophyll tablets can reduce odor and are more often chosen by patients. Flatus, flatulence and bloating are only partially curable. The disadvantage of activated carbon is the absorption of essential minerals and vitamins and beneficial microbes.
Smecta
It is important to know!
78% of people with gallbladder disease suffer from liver problems! Doctors strongly recommend that patients with gallbladder diseases undergo liver cleansing at least once every six months... Read more...
Smecta is a symptomatic drug that is used for chronic diarrhea. This medicine is an absorbent. For an adult, 3 sachets per day are required, and a weekly course is required. Oddly enough, a side effect of Smecta is flatulence.
Polyphepan
Inna Lavrenko
auto RU
Polyphepan is an adsorbent used for gastrointestinal diseases, flatulence and diarrhea. Tablets should be taken before meals, about 16 tablets per day. The medicine is tolerated very well, without causing dysbacteriosis. It is forbidden to take this drug for gastritis, atony of the intestinal tract, exacerbation of ulcers, duodenum.
Read also: Treatment methods for gallbladder tumors
Almagel
Almagel consists of magnesium and aluminum (hydroxides) and can reduce the harmful effects of gastric juice in cases of gastrointestinal diseases associated with its increase. Local anesthesia, laxative, adsorbent and choleretic effects have been proven. Almagel can be prescribed to adults for 12 days.
Motilium
Motilium is taken for severe bloating; it enhances motility in the intestinal tract and stops vomiting, relieves bloating and reduces belching. The active component of the drug, domperidone, is an antipsychotic and enhances the production of the hormone prolactin. Therefore, the side effect is amenorrhea and galactorrhea, gynecomastia. Contraindicated in pregnancy, renal failure, and diseases of the cardiovascular system.