Inflammatory processes in different parts of the ear lead to irritation of the nerves, swelling and severe pain. Treatment of otitis media must be started as quickly as possible, otherwise there may be serious consequences.
ALENA PARETSKAYA
Pathophysiologist, immunologist, member of the St. Petersburg Society of Pathophysiologists SVETLANA KOMAROVA Otolaryngologist, Deputy Chief Physician for CER at SM-Clinic
Acute pain in the ear is one of the most painful sensations. Many patients compare its strength with toothache and severe injuries, and women - with the process of childbirth. Most often, ear pain is due to otitis media.
What is otitis media
Otitis is the general name for inflammatory processes in the ear area.
Inflammation can be acute or chronic, affecting various parts of the ear. If the inflammation is localized in the auricle and ear canal to the border of the eardrum, this is otitis externa; inflammation in the tympanic cavity is otitis media; if the area of the cochlea is affected, the inner part of the ear is internal otitis or labyrinthitis.
These pathologies are extremely painful, accompanied by fever, hearing impairment, and discharge from the external meatus. In addition, without treatment, otitis media can lead to serious complications - hearing loss or complete deafness, paresis in the area of the facial nerve, damage to the bones or brain.
Providing emergency medical care for acute allergic diseases
Ph.D.
A.V. Topolyansky, professor A.L. Vertkin Scientific Center for Children's Health of the Russian Academy of Medical Sciences, Moscow MMA named after I.M. Sechenov MGMSU named after. ON THE. Semashko Station of ambulance and emergency medical care, Moscow National Scientific and Practical Society of Emergency Medical Care, Moscow
P
According to the National Scientific and Practical Society of Emergency Medical Services, over the past 3 years the number of calls for acute allergic diseases in the Russian Federation as a whole has increased by 18%. Moreover, their frequency in different regions ranges from 1 to 5% of all cases of emergency medical team visits.
Main causes and pathogenesis
The pathogenesis of allergic reactions has been studied quite fully today and is described in detail in many domestic and foreign monographs on allergology and clinical immunology. In any case, in the tissue of the shock organ or the “target” organ, which can be the skin, bronchi, gastrointestinal tract, etc., signs of allergic inflammation appear. The central role in the implementation of these immunopathological reactions belongs to class E immunoglobulins
(IgE), the binding of which to the antigen leads to the release of allergy mediators (histamine, serotonin, cytokines, etc.) from mast cells.
Most often, allergic reactions develop when exposed to inhaled allergens in homes, epidermal, pollen, food allergens, medications, parasite antigens, as well as stings and insect bites. Drug allergies most often develop when using analgesics, sulfonamides and antibiotics from the penicillin group, and less often cephalosporins. In addition, the incidence of latex allergy is high.
Clinical picture, classification and diagnostic criteria
From the point of view of providing assistance and assessing the prognosis, acute allergic diseases can be classified as follows (Table 1):
Lungs
– allergic rhinitis (year-round or seasonal), allergic conjunctivitis (year-round or seasonal), urticaria.
Moderate to heavy
– generalized urticaria, angioedema, acute laryngeal stenosis, moderate exacerbation of bronchial asthma, anaphylactic shock.
The greatest concern when providing medical care at the prehospital stage should be caused by prognostically unfavorable cases of development of life-threatening conditions in patients: severe asthma attack (status asthmaticus), anaphylactic shock, Quincke's edema in the larynx, acute laryngeal stenosis.
When analyzing the clinical picture of an allergic reaction, the emergency physician should receive answers to the questions presented in Table 2.
The initial examination should assess for the presence of: stridor, dyspnea, wheezing, dyspnea, or apnea; hypotension or syncope; changes on the skin (urticaria-type rashes, Quincke's edema, hyperemia, itching); gastrointestinal manifestations (nausea, abdominal pain, diarrhea); changes in consciousness. If the patient has stridor, severe shortness of breath, hypotension, arrhythmia, convulsions, loss of consciousness or shock, then this condition is considered life-threatening.
Treatment of acute allergic diseases
In case of acute allergic diseases at the prehospital stage, emergency therapy is based on the following areas:
Stopping further entry of the suspected allergen into the body
. For example, in case of a reaction to a drug administered parenterally or to an insect bite/sting, apply a tourniquet above the injection or sting site for 25 minutes (every 10 minutes, loosen the tourniquet for 1–2 minutes); to the injection or bite site - ice or a heating pad with cold water for 15 minutes; pricking at 5–6 points and infiltrating the injection or bite site with 0.3–0.5 ml of 0.1% epinephrine solution with 4.5 ml of isotonic sodium chloride solution.
Antiallergic therapy (antihistamines or glucocorticosteroids)
.
The administration of antihistamines is indicated for allergic rhinitis, allergic conjunctivitis, and urticaria. Glucocorticoid therapy (GCS) is carried out for anaphylactic shock and angioedema (in the latter case, the drug of choice): prednisolone
(adults - 60-150 mg, children - at the rate of 2 mg per 1 kg of body weight).
For generalized urticaria or when urticaria is combined with Quincke's edema, betamethasone
1-2 ml intramuscularly is highly effective. In case of angioedema, to prevent the effect of histamine on tissues, it is necessary to combine new generation antihistamines (loratadine) with glucocorticoids.
Symptomatic therapy
. With the development of bronchospasm, inhaled administration of b2-agonists and other bronchodilators and anti-inflammatory drugs through a nebulizer is indicated. Correction of arterial hypotension and replenishment of circulating blood volume is carried out by administering saline and colloid solutions (isotonic sodium chloride solution 500–1000 ml, hydroxyethyl starch 500 ml, polyglucin 400 ml). The use of vasopressor amines (dopamine 400 mg per 500 ml of 5% glucose, norepinephrine 0.2 - 2 ml per 500 ml of 5% glucose solution; the dose is titrated until a systolic pressure level of 90 mm Hg is achieved) is possible only after replenishment of the circulating blood volume . For bradycardia, it is possible to administer atropine in a dose of 0.3–0.5 mg subcutaneously (if necessary, the administration is repeated every 10 minutes). In the presence of cyanosis, dyspnea, and dry wheezing, oxygen therapy is also indicated.
Anti-shock measures
(Fig. 1). In case of anaphylactic shock, the patient should be laid down (head lower than legs), head turned to the side (to avoid aspiration of vomit), protract the lower jaw, and remove removable dentures. Epinephrine is administered subcutaneously in a dose of 0.1 - 0.5 ml of a 0.1% solution (drug of choice); if necessary, injections are repeated every 20 minutes for an hour under blood pressure monitoring. In case of unstable hemodynamics with the development of an immediate threat to life, intravenous administration of epinephrine is possible. In this case, 1 ml of 0.1% epinephrine solution is diluted in 100 ml of isotonic sodium chloride solution and administered at an initial rate of 1 mcg/min (1 ml per min). If necessary, the rate can be increased to 2–10 mcg/min. Intravenous administration of epinephrine is carried out under the control of heart rate, respiration, and blood pressure (systolic blood pressure must be maintained at a level of more than 100 mm Hg in adults and > 50 mm Hg in children). Medicines used for allergic diseases of varying severity and their effectiveness are presented in Table 3.
Rice. 1. Treatment algorithm for anaphylactic shock
Clinical pharmacology of drugs used for the treatment of acute allergic diseases.
The method of administration and dosage of antiallergic drugs are presented in Table 4.
Epinephrine
Epinephrine is a direct stimulator of a- and b-adrenergic receptors, which determines all its pharmacodynamic effects. The mechanism of antiallergic action is realized:
The method of administration and dosage of antiallergic drugs are presented in Table 4. Epinephrine is a direct stimulator of - and - adrenergic receptors, which determines all its pharmacodynamic effects. The mechanism of antiallergic action is realized:
• stimulation of a-adrenergic receptors, vasoconstriction of the abdominal organs, skin, mucous membranes, increased blood pressure;
• positive inotropic effect (the strength of heart contractions increases due to stimulation of b1-adrenergic receptors of the heart);
• stimulation of b2-adrenergic receptors of the bronchi (relief of bronchospasm);
• suppression of degranulation of mast cells and basophils (due to stimulation of intracellular cAMP).
When administered parenterally, the drug has a short-term effect (intravenous - 5 minutes, subcutaneously - up to 30 minutes), as it is quickly metabolized in the endings of sympathetic nerves, in the liver and other tissues with the participation of monoamine oxidase (MAO) and catechol-O-methyltransferase (COMT) .
Side effects:
dizziness, tremor, weakness; strong heartbeat, tachycardia, various arrhythmias (including ventricular), the appearance of pain in the heart area; difficulty breathing; increased sweating; excessive increase in blood pressure; urinary retention in men suffering from prostate adenoma; increased blood sugar levels in patients with diabetes. Tissue necrosis has also been described with repeated subcutaneous injection into the same place due to local vasoconstriction.
Contraindications:
arterial hypertension; severe cerebral atherosclerosis or organic brain damage; cardiac ischemia; hyperthyroidism; angle-closure glaucoma; diabetes; prostatic hypertrophy; pregnancy. However, even with these diseases, it is possible to prescribe epinephrine for anaphylactic shock for health reasons and under strict medical supervision.
Glucocorticosteroids
The mechanism of the antiallergic action of glucocorticoids is based on the following effects:
• immunosuppressive property (suppression of growth and differentiation of immune cells - lymphocytes, plasma cells, reduction in antibody production);
• prevention of degranulation of mast cells and the release of allergy mediators from them;
• decreased vascular permeability, increased blood pressure, improved bronchial obstruction.
Prednisolone is used for parenteral administration during emergency treatment at the prehospital stage.
.
For the treatment of bronchial asthma, allergic rhinitis, and allergic conjunctivitis, topical forms of glucocorticosteroids ( fluticasone, budesonide
) have been developed. Side effects of systemic corticosteroids: arterial hypertension, agitation, arrhythmia, ulcerative bleeding. Side effects of topical corticosteroids: hoarseness, disturbance of microflora with further development of mucosal candidiasis, when using high doses - skin atrophy, gynecomastia, weight gain, etc. Contraindications: peptic ulcer of the stomach and duodenum, severe arterial hypertension, renal failure , history of hypersensitivity to glucocorticoids.
Betamethasone
– glucocorticosteroid drug, consists of 2 mg of disodium phosphate and 5 mg of betamethasone dipropionate. Betamethasone disodium phosphate provides rapid onset of effect. Prolonged action is ensured by betamethasone dipropionate. The drug has immunosuppressive, antiallergic, desensitizing and antishock effects. Betamethasone is biotransformed in the liver. The dose of the drug depends on the severity of the disease and the clinical picture of the course. It is used for the treatment of acute allergic diseases in the form of intramuscular injections of 1–2 ml. With a single administration, no significant side effects were noted.
Antihistamines (H1-histamine receptor blockers)
There are several classifications of antihistamines. According to one of them, drugs of the first, second and third generation are distinguished (at the same time, the question of whether different drugs belong to the 2nd or 3rd generation is still debated). Another classification, more popular among clinicians, distinguishes between classic antihistamines, for example, chloropyramine, and new generation drugs (acrivastine, fexofenadine, loratadine, etc.)
It should be noted that classical antihistamines, in contrast to new generation drugs, are characterized by a short duration of action with a relatively rapid onset of clinical effect. Many of them are available in parenteral forms. All this determines the widespread use of classical antihistamines at the present time.
Chloropyramine
– one of the widely used classical antihistamines. It has significant antihistamine activity, peripheral anticholinergic and moderate antispasmodic effects. When taken orally, it is quickly and completely absorbed from the gastrointestinal tract. The maximum concentration in the blood is achieved within the first 2 hours, the therapeutic level of concentration remains for 4–6 hours. Effective in most cases for the treatment of seasonal and year-round allergic rhinitis and conjunctivitis, urticaria, atopic dermatitis, eczema; in parenteral form – for the treatment of acute allergic diseases requiring emergency care. Has a wide range of therapeutic doses used. It does not accumulate in the blood serum, therefore it does not cause an overdose with long-term use. The drug is characterized by a rapid onset of effect and a short duration (including side effects). Can be combined with other H1 blockers to increase the duration of the antiallergic effect. Available in tablets and ampoules for intramuscular and intravenous administration.
New generation antihistamines are devoid of cardiotoxic effects, have a competitive effect on histamine, are not metabolized by the liver (for example, the pharmacokinetics of acrivastine does not change even in patients with impaired liver and kidney function) and do not cause tachyphylaxis.
Akrivastine
– a drug with high antihistamine activity with minimally expressed sedative and anticholinergic effects. A feature of its pharmacokinetics is a low level of metabolism and the absence of accumulation and addiction. Acrivastine is preferred in cases where there is no need for continuous antiallergic treatment. The gelatin capsule is quickly absorbed in the stomach, providing a rapid onset of effect. The drug has a short period of action, which allows the use of a flexible dosage regimen. No cardiotoxic effect. Selectively influencing H1 receptors, it does not irritate the gastric mucosa. There is no effect on H2 receptors.
Loratadine
– a new generation antihistamine over-the-counter.
Indications for use: allergic rhinitis (seasonal and year-round), allergic conjunctivitis, urticaria, generalized urticaria, Quincke's edema, allergic reactions to insect bites, itchy dermatoses (contact allergic dermatitis, chronic eczema).
The drug has no side effects such as drowsiness, dry mouth, headache, dizziness.
Bronchospasmolytics: short-acting b2-agonists and anticholinergics
Berodual is a combined bronchospasmolytic drug containing two bronchodilators: fenoterol (b2-agonist) and ipratropium bromide (anticholinergic). One dose of Berodual contains 0.05 mg of fenoterol and 0.02 mg of ipratropium bromide.
Method of use: using a nebulizer to relieve an attack of suffocation, inhale 10–20 drops of Berodual in 1–4 ml of physiological solution for 5–10 minutes. If there is no improvement, repeat inhalation after 20 minutes.
Salbutamol
– selective agonist of b2- adrenergic receptors. The bronchodilator effect of salbutamol occurs within 4–5 minutes. The effect of the drug gradually increases to its maximum at 40–60 minutes. The half-life is 3–4 hours, duration of action is 4–5 hours.
Directions for use: using a nebulizer; nebulas of 2.5 ml containing 2.5 mg of salbutamol in saline solution. 1–2 nebulas (2.5–5.0 mg) are prescribed for inhalation, undiluted. If there is no improvement, repeat inhalations of 2.5 mg every 20 minutes. In one hour.
Typical errors in the use of drugs in the treatment of acute allergic diseases at the prehospital stage
• Isolated administration of H1-histamine blockers for severe allergic reactions, as well as for broncho-obstructive syndrome, has no independent significance and at the prehospital stage only leads to unjustified loss of time.
• The use of diprazine is also dangerous because it worsens hypotension.
• Late administration of GCS; unreasonable use of small doses of corticosteroids.
• Use of certain drugs not indicated for the treatment of allergic diseases (calcium gluconate, calcium chloride, etc.).
• The presence of unidirectional drugs in the equipment list of ambulance teams is not economically justified.
• Non-use of topical corticosteroids and b2-agonists for allergic laryngeal stenosis and bronchospasm.
Patients with severe allergic diseases must be hospitalized. For mild allergic diseases, the issue of hospitalization is decided on an individual basis in each case.
APPENDIX
Allergic stenosis of the upper respiratory tract in children
Main causes and pathogenesis
Upper respiratory tract obstruction syndrome (croup, acute stenosing laryngotracheitis) in children is one of the common reasons for seeking emergency care. There are acute allergic stenosis of the larynx and stenosis developing against the background of ARVI.
The main reason for the development of allergic stenosis of the upper respiratory tract with a predominant localization of the process in the larynx is the body’s sensitization to food and drug allergens, as well as to allergens of house dust mites (Dermatophagoides pteronyssinus and Dermatophagoides farinae), animals, etc.
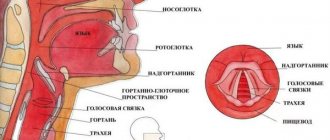
Acute allergic stenosis of the upper respiratory tract
more often observed in children with a hereditary predisposition to allergies. The development of croup is often preceded by the appearance of symptoms of skin and respiratory allergies. The occurrence of allergic stenosis of the larynx is also favored by such anatomical features of this organ in children as the softness of the cartilaginous skeleton, a short and narrow vestibule and a high-lying larynx, the presence of a delicate mucous membrane rich in cellular elements and a loose submucosal layer with an abundant vascular network and a large number of mast cells. . These structural features of the mucous and submucous membranes are especially characteristic of the area of the larynx surrounded by dense cricoid cartilage. This area is projected onto the subglottic space, where the most pronounced edema develops in children. Croup most often develops in children aged 6 months to 3 years, and boys suffer from it 3–4 times more often than girls.
The pathogenetic basis of allergic stenosis of the upper respiratory tract is IgE-mediated allergic reactions, causing the development of inflammation in the laryngeal mucosa in the form of edema, hypersecretion of mucus, spasm of the smooth muscles of the upper respiratory tract; In some patients, bronchospasm also occurs. The development of acute stenosing laryngotracheitis may also be associated with exposure to a viral infection, chemical pollutants, and changes in the weather situation.
Clinical picture, classification and diagnostic criteria
Acute laryngeal stenosis causes the development of respiratory failure and disruption of the child’s general condition. There are three degrees of stenosis
depending on the severity of the narrowing of the larynx:
I degree
laryngeal stenosis – compensated stenosis;
II degree
– subcompensated stenosis;
III degree
– decompensated stenosis (Table 5).
Children with allergic laryngeal stenosis are usually found to have heredity burdened by allergic reactions and diseases; they often also have manifestations of atopic dermatitis, food and drug allergies.
This variant of croup is characterized by the sudden development of stenosis “against the background of complete health,” in the absence of catarrhal symptoms, normal body temperature, as well as relatively rapid relief of symptoms of the disease when adequate therapy is prescribed. In a number of children, simultaneously with manifestations of allergic laryngeal stenosis, broncho-obstructive syndrome develops. Acute laryngeal stenosis, developing against the background of an acute respiratory infection, is characterized by a more gradual onset of the disease, the occurrence of stenosis against the background of catarrhal phenomena in the upper respiratory tract, an increase in temperature, the development of symptoms of intoxication, and inflammatory changes in a general blood test.
Laryngeal stenosis must be differentiated from laryngeal diphtheria, foreign body in the respiratory tract, obstructive bronchitis, retropharyngeal abscess, bronchial asthma, whooping cough, pneumonia with manifestations of respiratory failure.
Treatment of acute laryngeal stenosis
Children with acute laryngeal stenosis are subject to mandatory hospitalization. Therapy carried out for acute laryngeal stenosis should be pathogenetic and aimed at restoring air patency of the upper respiratory tract. Treatment is carried out taking into account the severity of laryngeal stenosis, begins with emergency medical services teams on call, and continues along the way to the hospital. The time required to provide prehospital care to a patient should not exceed 60 minutes.
For the treatment of acute laryngeal stenosis in the compensated stage (I degree) at the prehospital stage, inhalations of glucocorticosteroids are used (budesonide through a nebulizer at a dose of 0.25 mg; if nebulizers are ineffective or unavailable, antihistamines are used: intramuscularly (chloropyramine, 2% solution, 0.1 ml in the first year of life) or orally (for children over 12 years old - acrivastine (7 mg, capsule) or loratadine 10 mg (1 tablet or 2 teaspoons of syrup).
Treatment of acute laryngeal stenosis in the stage of incomplete compensation (II degree) begins with inhalation of glucocorticosteroids through a nebulizer at a dose of 0.5 mg. If ineffective, repeat budesonide inhalations in the same dose through a nebulizer with an interval of 20 minutes (maximum 3 times).
In the absence of nebulizers, antihistamines (chloropyramine intramuscularly) and systemic glucocorticosteroids (prednisolone at a rate of 2 mg/kg) are used. If the effect is insufficient, subcutaneous administration of a 0.1% epinephrine solution at the rate of 0.01 mg/kg body weight is additionally prescribed.
III degree laryngeal stenosis occurs with manifestations of respiratory and cardiovascular failure, metabolic disorders, and signs of toxicosis, which necessitates immediate hospitalization. At the prehospital stage, treatment of grade III laryngeal stenosis also begins with inhalation of glucocorticosteroids through a nebulizer at a dose of 1 mg.
If broncho-obstructive syndrome occurs, treatment is carried out with solutions of short-acting b2-agonists (berodual 10-20 drops for children under 6 years old or salbutamol - 1/2-1 nebul for children over 6 years old) through a nebulizer.
Causes of otitis media in adults
The most common causes of otitis externa are injuries, infections of the skin and underlying tissues in the ear canal area.
Chemical trauma to the ear, irritation and inflammation due to wax plugs, water getting into the ear, and the formation of boils are also possible. Otitis media is the most common form of the disease. It is usually provoked by bacterial infections, less commonly by viruses, pathogenic fungi, and mixed infections. The most common pathogens:
- Pneumococcus;
- hemophilus influenzae;
- influenza virus;
- various pathogens of ARVI.
In recent years, cases of fungal otitis media have become more frequently reported.
Risk factors that increase the likelihood of otitis media include sniffing and excess mucus in the nasopharynx. pressure difference when diving, diving to depth. Often, otitis media becomes a complication of a cold, ENT pathologies (adenoiditis, tonsillitis, pharyngitis, rhinitis). The risk is higher in people with immunodeficiencies.
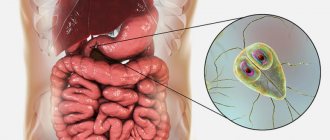
Gastrointestinal form of food allergy in children
The article presents generalized scientific and clinical data on the pathogenesis, clinical picture and treatment of gastrointestinal manifestations of food allergies in children.
Gastrointestinal forms of food allergy in children
The article presents generalized of scientific and clinical data on pathogenesis, clinical manifestations and therapy of gastrointestinal manifestations of food allergy in children.
Food allergy is intolerance to benign food products, not associated with metabolic disorders, caused by immunological reactions [12]. Food allergies can be caused by different types of allergic reactions. Of the 5 known types, the most commonly observed are: I (IgE - mediated mechanisms) - 92% of allergic reactions; Type III (immune complex reactions) - 53%, IV (cell-mediated reactions) - 76%. In the pathogenesis of gastrointestinal symptoms of food allergy, non-IgE-mediated immunological mechanisms associated with the activation of lymphocytes and the recruitment of eosinophils and mast cells play a significant role [8].
According to the frequency of allergic reactions in children, food allergens are divided into 4 groups: Group 1 - food allergens responsible for 78% of allergic reactions (egg -36%, peanuts -24%, cow's milk -8%, mustard -6%, fish - 4%; Group 2 - 10% of allergic reactions to food: shrimp, kiwi, wheat, beef, peas, lentils, soybeans, lupine; Group 3 - 10% of allergic reactions: sesame, pork, almonds, crab, pepper, apple, cherry , banana, chicken, goat's milk, duck, hazelnuts; group 4 - 2,% allergic reactions: chestnut, peach, turkey, potato [17].
According to Russian authors, the most common allergy in young children is to cow's milk proteins [13]. In 0.5% - 1.5% of children under one year of age, sensitization to milk also occurs [3]. Milk allergenicity is mainly associated with alpha-lactalbumin, beta-lactoglobulin, seroalbumin, gammaglobulin and casein.
Chicken eggs are highly allergenic. The most significant allergens are egg white proteins: ovomucoid, ovalbumin, conalbumin, lysozyme. The most stable and active allergen from this list is ovomucoid. Allergic reactions can also develop to egg yolk protein - livetin.
Fish belongs to the group of foods with a high allergenic potential. The most studied allergen at present is cod M, which is a sarcoplasmic protein from the parvalbumin group. Some types of fish (mackerel and tuna) are low in parvalbumin and therefore less allergenic. Fish can also be an inhalant allergen for sensitized individuals. The development of sensitization of the body can be initiated by crustaceans (shrimp, crabs). Currently, two types of food allergens have been identified in shrimp and three in crabs.
The cause of allergic reactions to food can be legumes: ground nuts (peanuts), soybeans, green peas. There are three groups of peanut proteins, among which the main allergens are arachine - alpha and lectin - reactive glycoprotein. Systemic allergic reactions have been described after eating peanuts. In soybean proteins, glycinin (11S fraction), b - conglycinin (7S fraction) and 2S fraction have allergenic activity. Allergy to soy protein isolate is observed in 15%-20% of children fed soy formula [12].
Children with food allergies often exhibit sensitization to cereal allergens. In the composition of wheat proteins, allergies are caused by: albumin, globulin, gliadin and glutenin (gluten complex),
Meat (beef, chicken and turkey) is a rare cause of allergies in children.
Among the food additives that can induce true food allergies are: papain, alpha-amylase, red cochineal (carmine) and sulfites.
The food allergy clinic is extremely polymorphic. It would not be an exaggeration to believe that with this type of sensitization, damage to any organ or system of the body is possible. Most often, food allergies are accompanied by pathological symptoms from the skin, gastrointestinal and respiratory tracts [5, 8, 9, 13].
Allergic lesions of the digestive organs occur with the same frequency as allergic dermatitis, but are still rarely diagnosed [2, 4, 7]. The development of allergic reactions is greatly facilitated by the extensive surface of the mucosa, its constant direct contact with the allergen and background gastroenterological pathology, which facilitates antigen penetration of the intestinal epithelium. It is important to emphasize that there are no specific clinical symptoms for damage to the digestive organs that are characteristic exclusively of the allergic nature of the disease. In part, this is the basis of numerous diagnostic errors, as a result of which patients receive treatment for intestinal infections, intestinal dysbiosis, chronic gastroduodenitis, reflux disease for a long time, and in some cases undergo unnecessary surgical intervention.
Infants are characterized by acute symptoms and generalization of the process involving significant areas of the mucous membrane. At older ages, a subacute and chronic course is more often observed. An allergic reaction can manifest itself as a symptom complex of glossitis, esophagitis, gastritis, enterocolitis.
In case of an allergic lesion of the oral cavity, swelling of the lips, tongue, and buccal mucosa develops immediately after contact with a food allergen. Possible aphthous stomatitis, catarrhal gingivitis.
Acute gastritis, as a manifestation of food allergy, is observed with sporadic consumption of the allergen. In young children, a few minutes after feeding, against the background of satisfactory health and normal temperature, recurrent vomiting develops. Older children are characterized by nausea, hypersalivation, intense epigastric pain, severe pain in the epigastric and pyloroduodenal region. During endoscopy, swelling and hyperemia of the mucous membrane, a sharp increase in the secretion of gastric juice, increased gastric motility, pyloric spasm and antiperistaltic waves are observed.
With long-term regular consumption of food allergens, chronic gastritis and gastroduodenitis develop. The clinical picture of chronic gastritis is characterized by a connection between exacerbations and the intake of a causally significant allergen. The pain is intense, but short-lived, occurring during or after eating, accompanied by symptoms of gastric dyspepsia (nausea, vomiting). Characterized by a violation of the motor function of the stomach and duodenum, an increase in the acid-forming function of the stomach. An endoscopic examination reveals gastroesophageal reflux, cardia insufficiency, superficial degeneration of the epithelium, and villous subatrophy. Erosive and ulcerative lesions of the mucous membrane are rarely observed [14].
Allergic esophagitis most often develops in older children and adolescents. It is characterized by a clinical picture of gastroesophageal reflux, dysphagia, intermittent vomiting, decreased appetite, abdominal pain, irritability, sleep disturbance, and lack of effect from standard antireflux therapy [1].
Young children may experience intestinal colic as a manifestation of food allergy [1, 6]. The attack develops acutely. A loud, piercing cry is typical, the child winces, grunts, and his face turns red. The stomach is tense, the legs are pulled up to the stomach. The attack occurs shortly after feeding. Symptoms disappear when a hypoallergenic diet is prescribed.
Enteritis with food allergies can occur in the form of anaphylactic (acute), acute and chronic forms. Anaphylactic form is observed in children in the first months of life with intolerance to cow's milk. A sharp deterioration in the child’s condition is observed after repeated feeding with a formula based on cow’s milk. There is pallor, severe pain (crying, anxiety), regurgitation, vomiting, acetonemia, severe bloating, tension, frequent stools with mucus and blood. Laboratory examination reveals anemia, eosinophilia, thrombocytopenia, and hypoproteinemia. The coprogram contains mucus, eosinophils, neutral fat, and red blood cells. The acute form of enteritis is manifested by bloating, colicky pain, and frequent bowel movements. The chronic form of allergic enteritis develops during a long-term allergic process; it is characterized by persistent malabsorption syndrome, more often - impaired absorption of lactose, sucrose, and glucose.
Allergic colitis is more often observed in children of the first months. Clinical symptoms appear 2-5 weeks after introducing the allergen into the diet. Characterized by anxiety after feeding, colic, bloating, unstable, mucous stool mixed with blood. The coprogram contains leukocytes, eosinophils, epithelial cells, fibrin threads. Sigmoidoscopy reveals cyanotic, bleeding intestinal mucosa [1, 14].
The significant role of food allergies in the formation of colitis and proctitis in children, accompanied by chronic constipation, persistent itching of the anorectal area, has been proven; in the most severe cases, the development of intestinal bleeding and posthemorrhagic anemia is possible [12].
Diagnosis of food allergy is based on analysis of medical history, allergological and laboratory examination results. An allergic history allows us to establish a connection between allergic manifestations and the consumption of certain foods. Keeping a food diary and an elimination diet helps to find out the necessary data.
Important information during the examination is provided by skin tests with food allergens (scarification test, prick test). The results of skin testing are taken into account when confirmed by history or provocative testing.
The “gold standard” for diagnosing food allergies is oral provocative tests [16]. Provocative tests are carried out in older children using a double-blind, placebo-controlled (DSPCPT) method only in a hospital setting. In children under 3 years of age, an open provocation test is performed under the supervision of trained personnel (the suspected food product is prescribed in its normal, undisguised form). It is not recommended to perform a challenge test with fish, eggs, milk and peanuts due to the high risk of systemic allergic reactions.
For widespread allergic skin lesions, in vitro allergy diagnostics are recommended. Various types of immunological methods are used (fluorescent immunoenzyme methods, ELISE, MAST - CLA, RASTCAP). Immunological diagnostics makes it possible to identify allergen-specific IgE to suspected allergens. Studies in recent years have shown that the level of specific IgG only indicates the use of this product in the past and, therefore, is not significant for dietary recommendations to the patient [13].
Children with food allergies need a comprehensive examination of the condition and function of the digestive organs using laboratory, ultrasound and endoscopic methods.
The basis of pathogenetic therapy for food allergies is: maintaining breastfeeding, using medicinal mixtures, and using elimination diets.
For a child of the first year of life, when treating food allergies, natural feeding is of paramount importance. In this case, rational nutrition of the mother becomes of great importance. The principles of a hypoallergenic diet for nursing mothers assume full satisfaction of physiological needs for energy and all replaceable and essential nutrients. From a nursing woman's diet, it is necessary to completely exclude foods to which the child is allergic, foods with preservatives, flavors, and dyes. Excluded: marinades, smoked meats, spices, salty and spicy dishes, stone meat, chicken and mushroom broths, carbonated drinks, products with dyes and preservatives, cow's milk, eggs, fish, seafood, honey, chocolate, nuts, citrus fruits. You should avoid consuming large quantities of foods and dishes that contain histamine and have a histamine-liberating effect, as well as combining them in the same day’s menu. Allowed: fermented milk products (in the absence of an allergic reaction in the child) without fruit additives, cereals (buckwheat, rice, corn, oatmeal, pearl barley), vegetables and fruits (white cabbage, Brussels sprouts, cauliflower, zucchini, lettuce, rutabaga, Jerusalem artichoke, green apples varieties, plums, white currant berries, gooseberries, lingonberries, cranberries, honeysuckle), vegetarian soups, meat (low-fat varieties of beef, pork; horse meat, rabbit, venison, lamb, turkey fillet, chicken) boiled, stewed, as well as in the form of steam cutlets, drinks (tea without dyes, flavors, compotes, fruit drinks).
If food allergies develop in breastfed children, nursing mothers can replace cow's milk in the mother's diet with goat's milk (Amalthea) based on individual indications. The main whey protein of goat's milk, in contrast to cow's, is alpha-lactalbumin, and the content of the main allergenic determinants (as 1 - casein and b - lactalbumin) is significantly lower [15].
If an allergy to cow's milk occurs in formula-fed children, formula milk is replaced with medicinal formula..
For many years, formulas based on soy protein isolate have been used for therapeutic nutrition of children. An important problem in recent years has been the constantly growing level of sensitization to soy proteins, reaching 20%, which significantly reduces the effectiveness of diet therapy using soy mixtures. When treating diseases caused by food sensitization, mixtures based on high hydrolysis of cow's milk proteins are recommended. The domestic market offers a wide range of products containing complete hydrolysates of whey proteins and casein (Alfare, Pregestimil, Nutrilon Pepti TSC, Frisopep AS, Damil Pepti), a mixture of amino acids (Neocate). Since an allergy to cow's milk may lead to the development of sensitization to various types and fractions of protein, such a variety of mixtures makes it easier to choose the most adequate nutrition. The use of specialized products based on goat milk (a mixture of NENNI 1.2, NENNI 1.2 with prebiotics) may be recommended [7].
Breastfeeding in the first year of life is the “gold standard” of nutrition. But, despite all the known benefits, breast milk cannot fully meet the child’s growing needs for energy, vitamins and microelements.
Complementary feeding is all types of products and dishes, except for human milk or its substitutes, which are included in the diet of children 1 year of age.
The timing of introducing foods and complementary foods to children with food allergies differs from those in healthy children. The first complementary feeding is recommended at 5.0 months, but no later than 6 months, the second - 1 month after the introduction of the first complementary feeding [10].
The first dish introduced into a child’s diet may be vegetable puree or porridge. The decision on where to start always remains with the doctor, who takes into account a number of associated factors: the presence of functional intestinal disorders, nutrition-related diseases, various forms of food intolerance, symptoms of hypovitaminosis and lack of microelements, weight and height indicators. Porridges - free buckwheat, corn, rice, oatmeal, pearl barley. As a “starter porridge”, we should recommend a product made from gluten-free cereals (buckwheat, corn, rice). In order to keep the child’s gastrointestinal tract healthy during the period of introducing complementary foods, it is recommended to use cereals with pre- and probiotics. Industrially produced dairy-free porridges that do not require cooking and contain prebiotics (low-allergenic corn with inulin, low-allergenic rice porridge with prebiotics, oat porridge, wheat with prunes, 5 grains with linden blossom) and probiotics (Oats, wheat with prunes, 5 grains) have proven themselves well. with linden blossom, 8 cereals with BL, Yoghurt-cereal with BL, Wheat-rice with L. Casei F19, Rice-corn with BL).
Vegetable puree (your choice of vegetables is individual): collard greens, light-colored pumpkin, zucchini, squash, cauliflower, broccoli, turnips, potatoes, rutabaga. As a debut, monocomponent purees from specialized baby food are chosen without the addition of cream and starch.
At 6.5-7 months, you can introduce second vegetable dishes or vegetable-cereals (for example, zucchini with corn grits, pumpkin with buckwheat ), jelly with fresh berry juice (cranberries, gooseberries, blueberries, rhubarb).
From 6 to 7 months, you can introduce meat puree from turkey, chicken, lamb, rabbit, beef, horse meat, lean pork, and venison.
Juices for children with allergic diseases should be introduced no earlier than 5.5 - 6 months from green and white apples (Antonovsky, Semerenko, white filling), plums, blueberries, gooseberries, rhubarb, yellow cherries, white currants with pulp.
Chicken egg yolk and fish are introduced into the diet of a child with food allergies much later than in healthy children.
A one-year-old child can be given vegetable puree from spinach, lettuce, vegetable salads from cucumbers and vinaigrettes containing vegetable oil.
Over the age of one year, food allergens remain important as leading trigger factors. When prescribing an elimination diet to a child, the basis for excluding a food product from the diet is anamnesis data confirmed by the results of an allergological examination and an oral provocative test. Therapeutic nutrition involves adherence to the regime, compliance of the daily volume of food, its qualitative composition with the age of the child (it is permissible to increase the number of meals by 1-2, which facilitates the digestion and absorption of nutrients). Dishes are prepared by stewing, boiling, steaming, in the form of soups, porridges, minced meat and purees. Salty and canned foods, spices, foods with dyes and preservatives are excluded. It is recommended to use special baby water for cooking, hypoallergenic (refined) vegetable oils, special mixtures of industrially produced cow's milk substitutes (“Nanny the Golden Goat”, “Frisopep”). These mixtures not only have reduced allergenicity, but are also characterized by an optimal (adapted) combination of food ingredients and are enriched with essential nutrients .
When organizing therapeutic nutrition for older children, the principles outlined (compliance with the diet, adequacy of the quantity and quality of food for the child’s age, exclusion of fried foods, spices, products with dyes and preservatives, elimination of identified causally significant allergens) retain their importance. The dynamics of sensitization in children should be taken into account: with age, sensitization becomes polyvalent, and allergies to household, medicinal and, most importantly, pollen allergens are added. Therefore, when choosing a diet, especially determining the list of plant products allowed for consumption, you need to keep in mind the possibility of cross-allergy. Significant changes occur in children's eating styles and eating habits during adolescence. During this period, the importance of such trigger factors as canned, flavored foods, carbonated drinks, and chips was noted. It is necessary to focus the attention of patients on this fact when drawing up individual treatment and rehabilitation programs.
Antihistamines are prescribed during periods of exacerbation of food allergies to reduce the severity of allergic inflammation, one of the main mediators of which is histamine.
At the “height” of exacerbation, especially in severe cases in young patients, 1st generation drugs that are available in injection form can be used: suprastin, tavegil. For less severe cases, you can use oral dosage forms of first-generation antihistamines: peritol, fenistil, fenkarol. The drug peritol, in addition to antihistamine, has anti-serotonin and anabolic effects, therefore it is most effective in children with appetite disorders. Fenkarol is a drug with a complex effect aimed at blocking histamine receptors and stimulating the synthesis of the histaminase enzyme in the liver. The duration of therapy with 1st generation drugs should not exceed 5-8 days due to the possibility of developing tachyphylaxis, while 2nd generation drugs, if necessary, can be prescribed for significantly longer periods: from 2 weeks to 2 years.
In older children who need to maintain fairly high physical and mental activity during the day, 2nd generation drugs are more preferable: Zyrtec, Xyzal, Erius, loratadine.
In severe forms of gastrointestinal food allergy, systemic glucocorticosteroids are indicated as emergency measures..
Enterosorbents are drugs that effectively bind endogenous and exogenous compounds, supramolecular structures and cells in the gastrointestinal tract for the purpose of treating and/or preventing diseases. An ideal enterosorbent should be non-toxic, non-traumatic for mucous membranes, with good evacuation from the intestines, and with a high sorption capacity in relation to the removed components of chyme. Enterosorbents are capable of directly absorbing poisons and allergens. The binding of these compounds by the sorbent in noticeable quantities begins in the acidic environment of the stomach. In the small intestine, substances taken orally and components of the secretions of the mucous membrane, liver and pancreas are sorbed. In those parts of the intestine in which bacterial microflora is located, enterosorbents are able to bind microbial cells and their toxins. The consequence of these effects is the suppression or weakening of toxic-allergic reactions, inflammatory processes and the prevention of somatogenic exotoxicosis.
Sorbents are taken 1-1.5 hours before or after taking other medications and food, the course of treatment is 10-14 days. In case of severe diarrhea syndrome, it is recommended to use smecta, in the absence of diarrhea - enterosgel, polysorb.
Thus, diagnosing the gastrointestinal form of food allergy presents certain difficulties. For timely recognition of the disease and successful rehabilitation of the patient, an assessment of risk factors for allergic damage to the digestive organs, a carefully collected anamnesis, a comprehensive examination using modern methods and adequate pathogenetic therapy, tailored to the age and individual spectrum of sensitization of the patient, are required.
Kaznacheeva L.F., Ishkova N.S., Kaznacheev K.S.
Novosibirsk State Medical University
Kaznacheeva Larisa Fedorovna - Doctor of Medical Sciences, Professor, Head. Department of Hospital Pediatrics
Literature:
1. Alferov V.P., Romanyuk F.P., Proyda L.N. Food intolerance in children. - St. Petersburg, 2007. - 68 p.
2. Baranov A.A., Balabolkin I.I., Subbotina O.A. Gastrointestinal food allergy in children. - M.: Dynasty, 2002. - 172 p.
3. Borovik T.E. Prevention of food allergies in children // Russian Pediatric Journal. - 2004. - No. 2. — P.61-63
4. Bulatova E.M., Pirtskhelava T.L., Bogdanova N.M. and others. Experience in using a modern formula based on goat’s milk in the nutrition of children in the first year of life // Issues of modern pediatrics. - 2005. - No. 4. — P.6-11.
5. Vorontsov I.M., Matalygina O.A. Diseases associated with food sensitization in children. - L.: Medicine, 1986. - 272 p.
6. Denisov M.Yu. Diseases of the digestive system in young children. - M., 2010. - 304 p.
7. Diet therapy for allergies to cow's milk proteins using an adapted formula "Nanny" based on goat's milk in young children: Guidelines for doctors / I.I. Balabolkin, S.N. Denisova, T.B. Sentsova, etc. - M. - 2004. - 16 p.
8. Clinical allergology and immunology: a guide for practicing physicians / Ed. L.A. Goryachkina and K.P. Kashkina. - M., 2009. — 432 p.
9. Clinical allergology / Ed. acad. RAMS, prof. R.M. Khaitova. - M.: "MEDpress - inform". - 2002. - 623 p.
10. National program for optimizing the feeding of children in the first year of life in the Russian Federation. - M., 2010. - 68 p.
11. Nogaller A.M. Food allergies. - M.: Medicine, 1983 - 192 p.
12. Pampura A.N., Khavkin A.I. Classification and clinical manifestations of food allergies // Children's gastroenterology and nutrition. - 2003. - No. 20. — P.1126 — 1129.
13. Food allergies in children: A manual for doctors / I.I. Balabolkin, S.N. Denisova, N.V. Yukhtina, etc. - M., 2006. - 53 p.
14. Modern technologies for the rehabilitation of children with allergic dermatoses / L.F. Kaznacheeva, M.Yu. Denisov, A.V. Molokova, etc. - Novosibirsk, 2000. - 196 p.
15. The effectiveness of natural feeding in the treatment of atopic dermatitis in children: Guidelines for doctors / I.I. Balabolkin, T.B. Sentsova, S.N. Denisova, etc. - M. - 2005. - 24 p.
16. Chiaramonte LT, Lifahitz AT, Sneider AT Food allergy: a practical approach to diagnosis and management. Ed: Marcel Dekker. 1988
17. Molkhow P. Food allergies. Brussels, USB, 2000
Symptoms of otitis media in adults
With external otitis, the most common complaints are:
- pulsation in the ear, sharp pain radiating to the neck, eye or teeth;
- increased pain when chewing food, talking, closing the jaw;
- redness of the ear canal and auricle;
- hearing loss if there is discharge of pus into the ear canal area.
Acute otitis media begins with a rise in temperature along with shooting pain inside the ear.
It increases as mucus and pus accumulate in the cavity; after 2–3 days, the membrane ruptures, pus flows out of the ear and the condition improves. The temperature drops and the pain subsides. Then the rupture of the membrane heals without a trace. In the chronic form, mesotympanitis may occur - inflammation is localized in the area of the Eustachian tube and the lower, middle part of the tympanic cavity. A hole is formed in the membrane, but the membrane itself is stretched.
Key complaints:
- hearing loss;
- periodic appearance of pus from the ear;
- noise in the ear;
- dizziness;
- during exacerbation - pain and fever.
With the development of epitympanitis, a sharp decrease in hearing occurs, the release of foul-smelling pus, pressure in the ear, pain in the temples, and dizziness. Periods of exacerbation are followed by remissions, but hearing does not improve completely.
Heart diseases in children
All nosologies in pediatric cardiology are divided into several large groups:
- Congenital heart defects. These are anomalies in the development of the heart, its valves and great (main) vessels that occur in the 2-8th week of intrauterine development. These include defects of the interventricular, interatrial and/or aortopulmonary septa, open atrioventricular canal, ductus arteriosus, stenosis (narrowing) or insufficiency (incomplete closure of the leaflets) of valves, incorrect location of vessels or pathological collaterals between them (connections), absence of an atrium or ventricle, etc. .
- Valvular heart defects. These are acquired pathologies of the valve apparatus - stenosis (narrowing) or insufficiency.
- Diseases of the endocardium - the inner lining of the heart.
- Diseases of the myocardium - the middle (muscular) layer of the heart.
- Pathologies of the pericardium - the cardiac connective tissue sac.
- Pathologies of coronary circulation. This group includes myocardial infarction, Kawasaki disease (vasculitis of medium and small arteries) and anomalies of the origin and number of coronary arteries.
- Pulmonary hypertension. This is an overload of blood in the pulmonary arteries due to increased pressure in the pulmonary arteries.
- Heart damage due to hereditary diseases. They are the result of errors in the genetic code of the parents' germ cells; these mutations are passed on to the offspring. They can appear from birth or already in adulthood.
- Heart tumors.
- Vascular damage. Most often we are talking about arterial hypertension (increased blood pressure) or hypotension (lowered blood pressure).
- Heart rhythm disturbances are disturbances in the regularity and sequence of heart contractions. If the heart muscle is damaged, its course is distorted, which leads to an abnormal rhythm of heart contraction.
- Heart failure is a syndrome caused by decompensated dysfunction of the myocardium. That is, the heart is so affected that it is no longer able to provide the necessary blood output and supply blood to all organs.
It is important to clarify that heart disease rarely occurs in isolation. One pathology progresses and leads to another. Thus, aortic stenosis will lead to pulmonary hypertension, and infective endocarditis destroys the valves, resulting in defects. After myocardial infarction or inflammation (myocarditis), the conduction of impulses through the affected area is disrupted, and as a result, the normal rhythm of contractions is disrupted.
Diagnostics
The diagnosis can be suspected based on typical complaints, but the doctor will ask in detail where and how the ear hurts, press on the tragus, pull the earlobe down to determine whether there is pain. In addition, the otorhinolaryngologist will examine the ear using instruments and lighting to specifically examine the ear canal, eardrum, and determine whether there is pus or perforation in it. To determine sensitivity to antibiotics, flora culture is performed. The doctor may also prescribe:
- blood tests (general, biochemistry) to determine the nature of inflammation;
- X-ray of the paranasal sinuses, if a connection with sinusitis is suspected;
- X-ray of the temporal bone in chronic otitis media.
All this data is needed in order to determine treatment tactics, the need for antibiotics, surgical interventions (membrane perforation or other interventions).
Diagnosis of heart diseases
At each appointment, the pediatrician conducts auscultation (listening with a phonendoscope) and examination of the chest to check the functioning of the child’s heart, even if the patient came in for ARVI. Pathological murmur is easily auscultated by a cardiologist. It indicates heart problems, even if the patient is not worried about anything or does not attach importance to some symptoms (in addition, children are sometimes afraid to report their problems and worries).
Basic diagnostic methods in cardiology:
- ECG (assessment of the conduction of electrical impulses through the heart muscle);
- Daily ECG monitoring;
- Ultrasound of the heart;
- Echo-CG (study of the morphology and functional state of the heart);
- Doppler echo-CG (study of blood flow in the chambers of the heart and great vessels);
- Plain radiography of the chest (determining the size and location of the cardiac shadow);
- Coronary angiography (study of coronary vessels);
- CT;
- MRI.
It is important to identify the disease in time: the earlier treatment is started, the better the effect. However, most violations can only be detected using special equipment. In addition, the baby is not able to voice complaints, so instrumental diagnostics in pediatrics cannot be avoided.
Modern methods of treatment
We asked otolaryngologist Svetlana Komarova to talk about how otitis in adults is treated today. According to her, drug therapy may include:
- drops in the ear containing the analgesic Phenazone and the local anesthetic Lidocaine - to relieve pain and reduce inflammation, if discharge from the ear appears, antibacterial drops containing Rifampicin or Ciprofloxacin should be used;
- vasoconstrictor drops containing Xylometazoline 0.1%, Oxymetazoline 0.05%, Naphazoline 0.1%, Phenylephrine 0.025% are instilled into the nose to reduce swelling of the nasopharyngeal mucosa around the mouth of the auditory tubes;
- if local drugs are ineffective, analgesics and non-steroidal anti-inflammatory drugs (Acetylsalicylic acid, Paracetamol, Tramadol, Ketoprofen, Ibuprofen) are prescribed orally;
- antipyretic drugs (Paracetamol) are used when the temperature rises above 38.5 C;
- antihistamines (Diphenhydramine, Clemastine, Chloropyramine) are prescribed to reduce swelling;
- broad-spectrum antibacterial drugs: penicillins, cephalosporins, macrolides, respiratory fluoroquinolones.
Non-drug treatment methods:
- procedures prescribed by an otolaryngologist: lavage of the external auditory canal, catheterization of the auditory tube, blowing of the auditory tubes according to Politzer, pneumomassage of the eardrum;
- physiotherapy: ultraviolet irradiation, UHF, microwave therapy, electrophoresis with anti-inflammatory drugs as prescribed by a physiotherapist.
Non-drug treatment methods help relieve pain, restore hearing and prevent complications.
In case of complicated otitis or the ineffectiveness of conservative therapy, surgical treatment (myringotomy, bypass of the tympanic cavity, radical surgery on the middle ear) is indicated, aimed at sanitizing the source of infection, restoring hearing, and preventing relapses.
What antibiotics are effective for otitis media?
“Systemic antibacterial therapy is indicated in all cases of moderate and severe acute otitis media,” says otolaryngologist Svetlana Kovaleva, “as well as in patients with immunodeficiency conditions.
If otitis is mild (no pronounced symptoms of intoxication, pain, hyperthermia up to 38 ° C), you can refrain from prescribing antibiotics. However, if there is no positive dynamics within 48 hours, antibiotic therapy should be resorted to. For otitis, broad-spectrum antibiotics are prescribed that are effective against typical pathogens: Streptococcus pneumoniae, Haemophilus influenzae, Moraxella catarrhalis, Streptococcus pyogenes, Staphylococcus aureus.
The drug of choice is Amoxicillin.
Alternative drugs for allergies to β-lactams are modern macrolides (Josamycin, Azithromycin, Clarithromycin). In case of ineffectiveness, as well as in patients who have received antibiotics for a month, for patients over 60 years of age, it is advisable to prescribe a complex - amoxicillin + clavulanic acid. Alternative drugs are II-III generation cephalosporins (Cefuroxime axetil, Ceftibuten) or fluoroquinolones (Levofloxacin, Moxifloxacin).
For mild to moderate cases, oral antibiotics are indicated. In severe and complicated cases of otitis, begin with intravenous or intramuscular administration of the drug, and then continue treatment orally.
The duration of antibacterial therapy is 7–10 days. For complicated otitis – 14 days or more.
You should not use antibiotics on your own; you should consult an otolaryngologist. Otitis media can be caused by fungal flora or herpes infection. The use of antibiotics in this case can worsen the course of the disease.
The article presents generalized scientific and clinical data on the pathogenesis, clinical picture and treatment of gastrointestinal manifestations of food allergies in children.
Gastrointestinal forms of food allergy in children
The article presents generalized of scientific and clinical data on pathogenesis, clinical manifestations and therapy of gastrointestinal manifestations of food allergy in children.
Food allergy is intolerance to benign food products, not associated with metabolic disorders, caused by immunological reactions [12]. Food allergies can be caused by different types of allergic reactions. Of the 5 known types, the most commonly observed are: I (IgE - mediated mechanisms) - 92% of allergic reactions; Type III (immune complex reactions) - 53%, IV (cell-mediated reactions) - 76%. In the pathogenesis of gastrointestinal symptoms of food allergy, non-IgE-mediated immunological mechanisms associated with the activation of lymphocytes and the recruitment of eosinophils and mast cells play a significant role [8].
According to the frequency of allergic reactions in children, food allergens are divided into 4 groups: Group 1 - food allergens responsible for 78% of allergic reactions (egg -36%, peanuts -24%, cow's milk -8%, mustard -6%, fish - 4%; Group 2 - 10% of allergic reactions to food: shrimp, kiwi, wheat, beef, peas, lentils, soybeans, lupine; Group 3 - 10% of allergic reactions: sesame, pork, almonds, crab, pepper, apple, cherry , banana, chicken, goat's milk, duck, hazelnuts; group 4 - 2,% allergic reactions: chestnut, peach, turkey, potato [17].
According to Russian authors, the most common allergy in young children is to cow's milk proteins [13]. In 0.5% - 1.5% of children under one year of age, sensitization to milk also occurs [3]. Milk allergenicity is mainly associated with alpha-lactalbumin, beta-lactoglobulin, seroalbumin, gammaglobulin and casein.
Chicken eggs are highly allergenic. The most significant allergens are egg white proteins: ovomucoid, ovalbumin, conalbumin, lysozyme. The most stable and active allergen from this list is ovomucoid. Allergic reactions can also develop to egg yolk protein - livetin.
Fish belongs to the group of foods with a high allergenic potential. The most studied allergen at present is cod M, which is a sarcoplasmic protein from the parvalbumin group. Some types of fish (mackerel and tuna) are low in parvalbumin and therefore less allergenic. Fish can also be an inhalant allergen for sensitized individuals. The development of sensitization of the body can be initiated by crustaceans (shrimp, crabs). Currently, two types of food allergens have been identified in shrimp and three in crabs.
The cause of allergic reactions to food can be legumes: ground nuts (peanuts), soybeans, green peas. There are three groups of peanut proteins, among which the main allergens are arachine - alpha and lectin - reactive glycoprotein. Systemic allergic reactions have been described after eating peanuts. In soybean proteins, glycinin (11S fraction), b - conglycinin (7S fraction) and 2S fraction have allergenic activity. Allergy to soy protein isolate is observed in 15%-20% of children fed soy formula [12].
Children with food allergies often exhibit sensitization to cereal allergens. In the composition of wheat proteins, allergies are caused by: albumin, globulin, gliadin and glutenin (gluten complex),
Meat (beef, chicken and turkey) is a rare cause of allergies in children.
Among the food additives that can induce true food allergies are: papain, alpha-amylase, red cochineal (carmine) and sulfites.
The food allergy clinic is extremely polymorphic. It would not be an exaggeration to believe that with this type of sensitization, damage to any organ or system of the body is possible. Most often, food allergies are accompanied by pathological symptoms from the skin, gastrointestinal and respiratory tracts [5, 8, 9, 13].
Allergic lesions of the digestive organs occur with the same frequency as allergic dermatitis, but are still rarely diagnosed [2, 4, 7]. The development of allergic reactions is greatly facilitated by the extensive surface of the mucosa, its constant direct contact with the allergen and background gastroenterological pathology, which facilitates antigen penetration of the intestinal epithelium. It is important to emphasize that there are no specific clinical symptoms for damage to the digestive organs that are characteristic exclusively of the allergic nature of the disease. In part, this is the basis of numerous diagnostic errors, as a result of which patients receive treatment for intestinal infections, intestinal dysbiosis, chronic gastroduodenitis, reflux disease for a long time, and in some cases undergo unnecessary surgical intervention.
Infants are characterized by acute symptoms and generalization of the process involving significant areas of the mucous membrane. At older ages, a subacute and chronic course is more often observed. An allergic reaction can manifest itself as a symptom complex of glossitis, esophagitis, gastritis, enterocolitis.
In case of an allergic lesion of the oral cavity, swelling of the lips, tongue, and buccal mucosa develops immediately after contact with a food allergen. Possible aphthous stomatitis, catarrhal gingivitis.
Acute gastritis, as a manifestation of food allergy, is observed with sporadic consumption of the allergen. In young children, a few minutes after feeding, against the background of satisfactory health and normal temperature, recurrent vomiting develops. Older children are characterized by nausea, hypersalivation, intense epigastric pain, severe pain in the epigastric and pyloroduodenal region. During endoscopy, swelling and hyperemia of the mucous membrane, a sharp increase in the secretion of gastric juice, increased gastric motility, pyloric spasm and antiperistaltic waves are observed.
With long-term regular consumption of food allergens, chronic gastritis and gastroduodenitis develop. The clinical picture of chronic gastritis is characterized by a connection between exacerbations and the intake of a causally significant allergen. The pain is intense, but short-lived, occurring during or after eating, accompanied by symptoms of gastric dyspepsia (nausea, vomiting). Characterized by a violation of the motor function of the stomach and duodenum, an increase in the acid-forming function of the stomach. An endoscopic examination reveals gastroesophageal reflux, cardia insufficiency, superficial degeneration of the epithelium, and villous subatrophy. Erosive and ulcerative lesions of the mucous membrane are rarely observed [14].
Allergic esophagitis most often develops in older children and adolescents. It is characterized by a clinical picture of gastroesophageal reflux, dysphagia, intermittent vomiting, decreased appetite, abdominal pain, irritability, sleep disturbance, and lack of effect from standard antireflux therapy [1].
Young children may experience intestinal colic as a manifestation of food allergy [1, 6]. The attack develops acutely. A loud, piercing cry is typical, the child winces, grunts, and his face turns red. The stomach is tense, the legs are pulled up to the stomach. The attack occurs shortly after feeding. Symptoms disappear when a hypoallergenic diet is prescribed.
Enteritis with food allergies can occur in the form of anaphylactic (acute), acute and chronic forms. Anaphylactic form is observed in children in the first months of life with intolerance to cow's milk. A sharp deterioration in the child’s condition is observed after repeated feeding with a formula based on cow’s milk. There is pallor, severe pain (crying, anxiety), regurgitation, vomiting, acetonemia, severe bloating, tension, frequent stools with mucus and blood. Laboratory examination reveals anemia, eosinophilia, thrombocytopenia, and hypoproteinemia. The coprogram contains mucus, eosinophils, neutral fat, and red blood cells. The acute form of enteritis is manifested by bloating, colicky pain, and frequent bowel movements. The chronic form of allergic enteritis develops during a long-term allergic process; it is characterized by persistent malabsorption syndrome, more often - impaired absorption of lactose, sucrose, and glucose.
Allergic colitis is more often observed in children of the first months. Clinical symptoms appear 2-5 weeks after introducing the allergen into the diet. Characterized by anxiety after feeding, colic, bloating, unstable, mucous stool mixed with blood. The coprogram contains leukocytes, eosinophils, epithelial cells, fibrin threads. Sigmoidoscopy reveals cyanotic, bleeding intestinal mucosa [1, 14].
The significant role of food allergies in the formation of colitis and proctitis in children, accompanied by chronic constipation, persistent itching of the anorectal area, has been proven; in the most severe cases, the development of intestinal bleeding and posthemorrhagic anemia is possible [12].
Diagnosis of food allergy is based on analysis of medical history, allergological and laboratory examination results. An allergic history allows us to establish a connection between allergic manifestations and the consumption of certain foods. Keeping a food diary and an elimination diet helps to find out the necessary data.
Important information during the examination is provided by skin tests with food allergens (scarification test, prick test). The results of skin testing are taken into account when confirmed by history or provocative testing.
The “gold standard” for diagnosing food allergies is oral provocative tests [16]. Provocative tests are carried out in older children using a double-blind, placebo-controlled (DSPCPT) method only in a hospital setting. In children under 3 years of age, an open provocation test is performed under the supervision of trained personnel (the suspected food product is prescribed in its normal, undisguised form). It is not recommended to perform a challenge test with fish, eggs, milk and peanuts due to the high risk of systemic allergic reactions.
For widespread allergic skin lesions, in vitro allergy diagnostics are recommended. Various types of immunological methods are used (fluorescent immunoenzyme methods, ELISE, MAST - CLA, RASTCAP). Immunological diagnostics makes it possible to identify allergen-specific IgE to suspected allergens. Studies in recent years have shown that the level of specific IgG only indicates the use of this product in the past and, therefore, is not significant for dietary recommendations to the patient [13].
Children with food allergies need a comprehensive examination of the condition and function of the digestive organs using laboratory, ultrasound and endoscopic methods.
The basis of pathogenetic therapy for food allergies is: maintaining breastfeeding, using medicinal mixtures, and using elimination diets.
For a child of the first year of life, when treating food allergies, natural feeding is of paramount importance. In this case, rational nutrition of the mother becomes of great importance. The principles of a hypoallergenic diet for nursing mothers assume full satisfaction of physiological needs for energy and all replaceable and essential nutrients. From a nursing woman's diet, it is necessary to completely exclude foods to which the child is allergic, foods with preservatives, flavors, and dyes. Excluded: marinades, smoked meats, spices, salty and spicy dishes, stone meat, chicken and mushroom broths, carbonated drinks, products with dyes and preservatives, cow's milk, eggs, fish, seafood, honey, chocolate, nuts, citrus fruits. You should avoid consuming large quantities of foods and dishes that contain histamine and have a histamine-liberating effect, as well as combining them in the same day’s menu. Allowed: fermented milk products (in the absence of an allergic reaction in the child) without fruit additives, cereals (buckwheat, rice, corn, oatmeal, pearl barley), vegetables and fruits (white cabbage, Brussels sprouts, cauliflower, zucchini, lettuce, rutabaga, Jerusalem artichoke, green apples varieties, plums, white currant berries, gooseberries, lingonberries, cranberries, honeysuckle), vegetarian soups, meat (low-fat varieties of beef, pork; horse meat, rabbit, venison, lamb, turkey fillet, chicken) boiled, stewed, as well as in the form of steam cutlets, drinks (tea without dyes, flavors, compotes, fruit drinks).
If food allergies develop in breastfed children, nursing mothers can replace cow's milk in the mother's diet with goat's milk (Amalthea) based on individual indications. The main whey protein of goat's milk, in contrast to cow's, is alpha-lactalbumin, and the content of the main allergenic determinants (as 1 - casein and b - lactalbumin) is significantly lower [15].
If an allergy to cow's milk occurs in formula-fed children, formula milk is replaced with medicinal formula..
For many years, formulas based on soy protein isolate have been used for therapeutic nutrition of children. An important problem in recent years has been the constantly growing level of sensitization to soy proteins, reaching 20%, which significantly reduces the effectiveness of diet therapy using soy mixtures. When treating diseases caused by food sensitization, mixtures based on high hydrolysis of cow's milk proteins are recommended. The domestic market offers a wide range of products containing complete hydrolysates of whey proteins and casein (Alfare, Pregestimil, Nutrilon Pepti TSC, Frisopep AS, Damil Pepti), a mixture of amino acids (Neocate). Since an allergy to cow's milk may lead to the development of sensitization to various types and fractions of protein, such a variety of mixtures makes it easier to choose the most adequate nutrition. The use of specialized products based on goat milk (a mixture of NENNI 1.2, NENNI 1.2 with prebiotics) may be recommended [7].
Breastfeeding in the first year of life is the “gold standard” of nutrition. But, despite all the known benefits, breast milk cannot fully meet the child’s growing needs for energy, vitamins and microelements.
Complementary feeding is all types of products and dishes, except for human milk or its substitutes, which are included in the diet of children 1 year of age.
The timing of introducing foods and complementary foods to children with food allergies differs from those in healthy children. The first complementary feeding is recommended at 5.0 months, but no later than 6 months, the second - 1 month after the introduction of the first complementary feeding [10].
The first dish introduced into a child’s diet may be vegetable puree or porridge. The decision on where to start always remains with the doctor, who takes into account a number of associated factors: the presence of functional intestinal disorders, nutrition-related diseases, various forms of food intolerance, symptoms of hypovitaminosis and lack of microelements, weight and height indicators. Porridges - free buckwheat, corn, rice, oatmeal, pearl barley. As a “starter porridge”, we should recommend a product made from gluten-free cereals (buckwheat, corn, rice). In order to keep the child’s gastrointestinal tract healthy during the period of introducing complementary foods, it is recommended to use cereals with pre- and probiotics. Industrially produced dairy-free porridges that do not require cooking and contain prebiotics (low-allergenic corn with inulin, low-allergenic rice porridge with prebiotics, oat porridge, wheat with prunes, 5 grains with linden blossom) and probiotics (Oats, wheat with prunes, 5 grains) have proven themselves well. with linden blossom, 8 cereals with BL, Yoghurt-cereal with BL, Wheat-rice with L. Casei F19, Rice-corn with BL).
Vegetable puree (your choice of vegetables is individual): collard greens, light-colored pumpkin, zucchini, squash, cauliflower, broccoli, turnips, potatoes, rutabaga. As a debut, monocomponent purees from specialized baby food are chosen without the addition of cream and starch.
At 6.5-7 months, you can introduce second vegetable dishes or vegetable-cereals (for example, zucchini with corn grits, pumpkin with buckwheat ), jelly with fresh berry juice (cranberries, gooseberries, blueberries, rhubarb).
From 6 to 7 months, you can introduce meat puree from turkey, chicken, lamb, rabbit, beef, horse meat, lean pork, and venison.
Juices for children with allergic diseases should be introduced no earlier than 5.5 - 6 months from green and white apples (Antonovsky, Semerenko, white filling), plums, blueberries, gooseberries, rhubarb, yellow cherries, white currants with pulp.
Chicken egg yolk and fish are introduced into the diet of a child with food allergies much later than in healthy children.
A one-year-old child can be given vegetable puree from spinach, lettuce, vegetable salads from cucumbers and vinaigrettes containing vegetable oil.
Over the age of one year, food allergens remain important as leading trigger factors. When prescribing an elimination diet to a child, the basis for excluding a food product from the diet is anamnesis data confirmed by the results of an allergological examination and an oral provocative test. Therapeutic nutrition involves adherence to the regime, compliance of the daily volume of food, its qualitative composition with the age of the child (it is permissible to increase the number of meals by 1-2, which facilitates the digestion and absorption of nutrients). Dishes are prepared by stewing, boiling, steaming, in the form of soups, porridges, minced meat and purees. Salty and canned foods, spices, foods with dyes and preservatives are excluded. It is recommended to use special baby water for cooking, hypoallergenic (refined) vegetable oils, special mixtures of industrially produced cow's milk substitutes (“Nanny the Golden Goat”, “Frisopep”). These mixtures not only have reduced allergenicity, but are also characterized by an optimal (adapted) combination of food ingredients and are enriched with essential nutrients .
When organizing therapeutic nutrition for older children, the principles outlined (compliance with the diet, adequacy of the quantity and quality of food for the child’s age, exclusion of fried foods, spices, products with dyes and preservatives, elimination of identified causally significant allergens) retain their importance. The dynamics of sensitization in children should be taken into account: with age, sensitization becomes polyvalent, and allergies to household, medicinal and, most importantly, pollen allergens are added. Therefore, when choosing a diet, especially determining the list of plant products allowed for consumption, you need to keep in mind the possibility of cross-allergy. Significant changes occur in children's eating styles and eating habits during adolescence. During this period, the importance of such trigger factors as canned, flavored foods, carbonated drinks, and chips was noted. It is necessary to focus the attention of patients on this fact when drawing up individual treatment and rehabilitation programs.
Antihistamines are prescribed during periods of exacerbation of food allergies to reduce the severity of allergic inflammation, one of the main mediators of which is histamine.
At the “height” of exacerbation, especially in severe cases in young patients, 1st generation drugs that are available in injection form can be used: suprastin, tavegil. For less severe cases, you can use oral dosage forms of first-generation antihistamines: peritol, fenistil, fenkarol. The drug peritol, in addition to antihistamine, has anti-serotonin and anabolic effects, therefore it is most effective in children with appetite disorders. Fenkarol is a drug with a complex effect aimed at blocking histamine receptors and stimulating the synthesis of the histaminase enzyme in the liver. The duration of therapy with 1st generation drugs should not exceed 5-8 days due to the possibility of developing tachyphylaxis, while 2nd generation drugs, if necessary, can be prescribed for significantly longer periods: from 2 weeks to 2 years.
In older children who need to maintain fairly high physical and mental activity during the day, 2nd generation drugs are more preferable: Zyrtec, Xyzal, Erius, loratadine.
In severe forms of gastrointestinal food allergy, systemic glucocorticosteroids are indicated as emergency measures..
Enterosorbents are drugs that effectively bind endogenous and exogenous compounds, supramolecular structures and cells in the gastrointestinal tract for the purpose of treating and/or preventing diseases. An ideal enterosorbent should be non-toxic, non-traumatic for mucous membranes, with good evacuation from the intestines, and with a high sorption capacity in relation to the removed components of chyme. Enterosorbents are capable of directly absorbing poisons and allergens. The binding of these compounds by the sorbent in noticeable quantities begins in the acidic environment of the stomach. In the small intestine, substances taken orally and components of the secretions of the mucous membrane, liver and pancreas are sorbed. In those parts of the intestine in which bacterial microflora is located, enterosorbents are able to bind microbial cells and their toxins. The consequence of these effects is the suppression or weakening of toxic-allergic reactions, inflammatory processes and the prevention of somatogenic exotoxicosis.
Sorbents are taken 1-1.5 hours before or after taking other medications and food, the course of treatment is 10-14 days. In case of severe diarrhea syndrome, it is recommended to use smecta, in the absence of diarrhea - enterosgel, polysorb.
Thus, diagnosing the gastrointestinal form of food allergy presents certain difficulties. For timely recognition of the disease and successful rehabilitation of the patient, an assessment of risk factors for allergic damage to the digestive organs, a carefully collected anamnesis, a comprehensive examination using modern methods and adequate pathogenetic therapy, tailored to the age and individual spectrum of sensitization of the patient, are required.
L.F. Kaznacheeva, N.S. Ishkova, K.S. Treasurers
Novosibirsk State Medical University
Kaznacheeva Larisa Fedorovna - Doctor of Medical Sciences, Professor, Head. Department of Hospital Pediatrics
Literature:
1. Alferov V.P., Romanyuk F.P., Proyda L.N. Food intolerance in children. - St. Petersburg, 2007. - 68 p.
2. Baranov A.A., Balabolkin I.I., Subbotina O.A. Gastrointestinal food allergy in children. - M.: Dynasty, 2002. - 172 p.
3. Borovik T.E. Prevention of food allergies in children // Russian Pediatric Journal. - 2004. - No. 2. — P.61-63
4. Bulatova E.M., Pirtskhelava T.L., Bogdanova N.M. and others. Experience in using a modern formula based on goat’s milk in the nutrition of children in the first year of life // Issues of modern pediatrics. - 2005. - No. 4. — P.6-11.
5. Vorontsov I.M., Matalygina O.A. Diseases associated with food sensitization in children. - L.: Medicine, 1986. - 272 p.
6. Denisov M.Yu. Diseases of the digestive system in young children. - M., 2010. - 304 p.
7. Diet therapy for allergies to cow's milk proteins using an adapted formula "Nanny" based on goat's milk in young children: Guidelines for doctors / I.I. Balabolkin, S.N. Denisova, T.B. Sentsova, etc. - M. - 2004. - 16 p.
8. Clinical allergology and immunology: a guide for practicing physicians / Ed. L.A. Goryachkina and K.P. Kashkina. - M., 2009. — 432 p.
9. Clinical allergology / Ed. acad. RAMS, prof. R.M. Khaitova. - M.: "MEDpress - inform". - 2002. - 623 p.
10. National program for optimizing the feeding of children in the first year of life in the Russian Federation. - M., 2010. - 68 p.
11. Nogaller A.M. Food allergies. - M.: Medicine, 1983 - 192 p.
12. Pampura A.N., Khavkin A.I. Classification and clinical manifestations of food allergies // Children's gastroenterology and nutrition. - 2003. - No. 20. — P.1126 — 1129.
13. Food allergies in children: A manual for doctors / I.I. Balabolkin, S.N. Denisova, N.V. Yukhtina, etc. - M., 2006. - 53 p.
14. Modern technologies for the rehabilitation of children with allergic dermatoses / L.F. Kaznacheeva, M.Yu. Denisov, A.V. Molokova, etc. - Novosibirsk, 2000. - 196 p.
15. The effectiveness of natural feeding in the treatment of atopic dermatitis in children: Guidelines for doctors / I.I. Balabolkin, T.B. Sentsova, S.N. Denisova, etc. - M. - 2005. - 24 p.
16. Chiaramonte LT, Lifahitz AT, Sneider AT Food allergy: a practical approach to diagnosis and management. Ed: Marcel Dekker. 1988
17. Molkhow P. Food allergies. Brussels, USB, 2000
Prevention of otitis in adults at home
To prevent otitis, it is necessary to avoid hypothermia, wash your hands after going outside, irrigate the nasal mucosa with sea water after visiting places with large crowds of people, exercise, exercise, and eat fresh fruits, vegetables, and dairy products every day.
If it so happens that you get sick and a runny nose begins to bother you, then you need to blow your nose extremely carefully, while freeing only one nostril, otherwise nasal discharge can get through the auditory tube into the ear and provoke otitis media.
Proper ear hygiene is essential. It is not recommended to use cotton swabs - they can introduce a bacterial or fungal infection into the ear. For ear hygiene, use drops consisting of a combination of surfactants (Allantoin, Benzetoin chloride) that clean, moisturize and protect the skin of the external auditory canal.