The digestive system of a newborn baby is not yet sufficiently developed. The internal organs are functionally defective, synthesize too few necessary enzymes, and the intestinal microflora is adapted only to the dairy type of diet.
An infant is still completely dependent on mother's milk. Any of the highest quality mixtures only approximate the composition, but do not replace it completely. Serious problems arise when feeding “artificial” babies.
Pediatricians judge the digestive process in a baby by the type and frequency of stool, appetite, and monthly weight gain. Gut bacteria perform many beneficial functions. To do this, a certain composition and ratio must be maintained. An imbalance (dysbacteriosis) in the direction of increasing or decreasing numbers leads to different symptoms.
Stool disorders are difficult for children to tolerate. Analysis for dysbiosis in infants helps to identify the causes of intolerance to nutritional mixtures and the nature of the disease.
Who is prescribed a stool test for dysbacteriosis?
Dysbacteriosis, not being a separate disease, accompanies various functional and pathological disorders. The doctor suspects dysbiosis if the child develops:
- too frequent loose stools with impurities uncharacteristic for age;
- bloating, delayed gases;
- regurgitation after eating a large volume of curdled milk;
- skin rash;
- connection with antibiotic treatment of various diseases;
- a tendency to frequent colds, indicating a weakened immune system.
The clinical symptoms are assessed by the doctor, but parents should know everything about normal bowel movements of the infant in order to notice abnormalities in time and get tested.
Decreased appetite and weight loss are a serious reason to check for dysbiosis
What is dysbiosis?
How to get tested for dysbacteriosis - an informative study
Dysbiosis, or (dysbiosis) is a microbial imbalance on or within the body. Usually, when dysbiosis is mentioned, the intestines are meant, but there may also be dysbiosis of the mucous membranes of other organs - the mouth, nose, vagina, etc.
Dysbiosis itself is not a disease, but it can accompany any disease. Such instability of the intestinal microflora may occur due to an inflammatory disorder or other pathologies. Dysbacteriosis depends on quantitative or qualitative changes in the microflora in the intestine.
The first symptoms of this condition are abdominal pain and diarrhea. To determine the state of the microflora, a stool test for dysbacteriosis is necessary. This study is prescribed for the following indications:
- Intestinal infections;
- Abdominal pain, flatulence, unstable stool
- Allergic reaction to certain foods;
- Long-term treatment with antibiotics and hormonal drugs.
Testing for dysbacteriosis is prescribed for infants with intestinal problems and adolescents prone to allergic manifestations and acute respiratory infections. To get tested for dysbacteriosis, you need to get a referral from your local or attending physician, who will issue a referral and advise which laboratory to contact.
But before sending you to the laboratory, the doctor will create a special diet that must be followed for a week. This diet will provide a state of the intestines in which the result of the state of the microbial flora will be as accurate as possible.
How does the baby's microflora change after birth?
The fetus in the womb is in sterile conditions. The intestines produce meconium (primary stool), which is passed in the first days of life. Already moving along the birth canal, the baby encounters the microflora of the mother’s body for the first time.
Normally, bifidobacteria, lactobacilli, and E. coli are present here. During breastfeeding, the baby acquires other microorganisms, and the intestines are colonized with their own microflora.
Ideal calculations show that a breast-fed baby should have almost 99% lactobacilli and bifidobacteria in its intestinal microflora. The rest is provided by opportunistic microorganisms.
What should parents of an infant remember?
Experienced pediatricians do not advise focusing on daily stool frequency. It is believed that this indicator is very individual and depends on:
- on the functional maturity of the digestive system;
- type of feeding;
- course of pregnancy and childbirth.
The main thing is to monitor the baby’s well-being, activity, regular bowel movements, and the absence of painful signs and pathological impurities in the stool. In the first month of life, defecation occurs after feeding. The frequency is allowed from once a day to 10–12. The main thing is that the child does not strain too much or scream. The consistency of the liquid mass is gradually replaced by the formed one. We should not forget that the liquid is absorbed into the diaper, so lumps remain on the surface.
The color of stool varies from golden yellow to yellow-green or yellow-brown. If breastfeeding is stopped, it becomes darker. The green tint is associated with the release of bilirubin from feces for up to six to nine months. The yellow discharge may turn green when the diaper is left exposed to air.
If the child has never had this symptom, but appeared against the background of other disorders, then a stool analysis should be checked. Both functional disorders (reaction to the introduction of complementary foods, lack of milk in the mother) and diseases of the baby that cause dysbacteriosis are possible.
When kissing, parents “share” their germs with their baby
The baby's stool may contain mucus and undigested white lumps. If the baby is feeling well, this indicates intolerance to complementary foods and a violation of the diet by the nursing mother. What inclusions are always alarming are: the presence of blood or pus. The symptom is considered dangerous. Parents should react appropriately and consult a doctor immediately.
Klebsiella (klebsiella)
| Klebsiella pneumoniae |
| Klebsiella oxytoca |
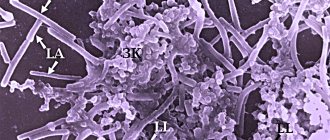
Klebsiella
(lat.
Klebsiella
) is a genus of gram-negative facultative anaerobic opportunistic bacteria.
They have the shape of short thick ellipsoidal rods measuring 0.6–6.0 by 0.3–1.0 microns. Klebsiella aerogenes
may have mobility ), do not form spores, have pronounced capsules, thanks to which Klebsiella are resistant to environmental influences and can survive for a long time in soil, in water, and on indoor objects. In dairy products, Klebsiella survives and multiplies both at room temperature and in the refrigerator. When heated to 65°C they die within an hour.
Most Klebsiella infections are caused by Klebsiella pneumonia
, in second place is
Klebsiella oxytoca
.
Klebsiella in the taxonomy of bacteria
According to modern classification, the genus Klebsiella
is included in the family Enterobacteriaceae (Latin
Enterobacteriaceae
), the order Enterobacteriales (Latin
Enterobacteriales
), the class Gamma-proteobacteria (Latin
γ proteobacteria
), the phylum Proteobacteria (Latin
Proteobacteria
), and the kingdom Bacteria.
Klebsiella belongs to the so-called coliform
bacteria.
According to the results of the latest revision, the composition of the Klebsiella genus has changed significantly. Now it includes species and subspecies:
- Klebsiella aerogenes
- Klebsiella granulomatis
- Klebsiella michiganensis
- Klebsiella milletis
- Klebsiella oxytoca
(Klebsiella oxytoca) - Klebsiella cf.
planticola B43 - Klebsiella pneumoniae
(Klebsiella pneumoniae), including subspecies: - Klebsiella pneumoniae subsp. ozaenae
- Klebsiella pneumoniae subsp. pneumoniae
- Klebsiella pneumoniae subsp. rhinoscleromatis
- Klebsiella quasipneumoniae subsp. quasipneumoniae
- Klebsiella quasipneumoniae subsp. similipneumoniae
Before the latest revision, the genus Klebsiella included the following species:
- Klebsiella pneumoniae
- Klebsiella ozaenae
(Klebsiella ozaena) subspecies
Klebsiella pneumoniae - Klebsiella rhinoscleromatis
(Klebsiella rhinoscleroma) - currently a subspecies of
Klebsiella pneumoniae - Klebsiella ornithinolytica
- currently
Raoultella ornithinolytica - Klebsiella oxytoca
- Klebsiella planticola
- currently
Raoultella planticola - Klebsiella terrigena
- currently
Raoultella terrigena
The species Klebsiella aerogenes
was previously included in the genus Enterobacter and was called
Enterobacter aerogenes.
The species
Klebsiella granulomatis
was formerly classified as
Calymmatobacterium granulomatis
, the only species of the now defunct genus Calymmatobacterium.
Species Klebsiella variicola
was recently isolated from the closely related species
Klebsiella pneumoniae
Genus Raoultella
, in which a number of species of the genus
Klebsiella have been reclassified,
also belongs to the family
Enterobacteriaceae
.
Klebsiella quasipneumoniae subsp. similipneumoniae
formerly called
Klebsiella alba.
Klebsiella michiganensis was isolated in 2013 from a household toothbrush holder.
Klebsiella in gastroenterology
Klebsiella (mainly Klebsiella pneumoniae
, but also
Klebsiella oxytoca , Klebsiella aerogenes
and others) is a representative of the normal microflora of the human intestine. At the same time, Klebsiella can cause a number of gastroenterological diseases. Klebsiella can cause acute gastritis - acute inflammation of the gastric mucosa that occurs due to the influence of an infectious factor directly on the gastric mucosa. This is usually associated with the consumption of poor quality food, improper storage of mixtures and products, and failure to comply with hygiene rules (Shabalov N.P.).
Klebsiella can begin to develop intensively, causing a pathological process in the gastrointestinal tract, in particular, after therapy with antibacterial drugs, the side effect of which is the suppression of the main representatives of the normal microflora of the gastrointestinal tract (bifidobacteria and others), inhibiting the excessive growth of Klebsiella (Shcherbakov P. L.).
In most patients, clebsibellosis occurs in the form of an intestinal infection and is characterized by an acute onset, nausea, vomiting, abdominal pain, diarrhea, fever and general weakness. The duration of the disease is 1–5 days. The sources of the infectious agent are a sick person and a bacteria carrier. The most common routes of transmission are foodborne, airborne and household contact. Transmission also occurs through contaminated food products, especially meat and dairy products. Klebsiellosis is one of the common nosocomial infections.
We recommend materials from Rospotrebnadzor “On the prevention of food poisoning and infectious diseases transmitted by food”
and WHO's
Guide to Safe Food for Tourists.
On the GastroScan.ru website in the “Literature” section there is a subsection “Microflora, microbiocenosis, dysbiosis (dysbacteriosis)”, containing publications for healthcare professionals that address the problems of microbiocenosis and dysbiosis of the human gastrointestinal tract.
Fecal analysis for Klebsiella
The number of Klebsiella in feces is counted when analyzing for dysbacteriosis.
This is usually a type of Klebsiella pneumoniae. The norm is no more than 105 Klebsiella per 1 g of feces. The presence of Klebsiella in the intestines does not always require antimicrobial therapy. According to the Helix laboratory service, the reference values for the content of Klebsiella in stool during microbiological examination of stool, both for patients under one year of age and for patients over one year of age, are:
- Klebsiella pneumoniaе
- less than 104 - Klebsiella oxytoca
- less than 104 - Klebsiella aerogenes
- less than 104
Klebsiella - pathogens of respiratory tract diseases
Representatives of the Klebsiella genus ( Klebsiella pneumoniae, Klebsiella quasipneumoniae
and other species) are the cause of a small number of community-acquired pneumonia - a few percent of all cases, but the mortality rate of such pneumonia caused by Klebsiella is very high - 35.7%.
Klebsiella rhinoscleromatis
is the causative agent of scleroma, granulomatous lesions of the nasal mucosa (rhinoscleroma) and the upper respiratory tract.
Klebsiella ozaenae
causes chronic diseases of the respiratory system, affecting the pharynx, larynx, and trachea.
Klebsiella aerogenes is isolated from the pharynx of patients with bronchial asthma and chronic nonspecific lung diseases
| Donovanosis (granuloma inguinalis), an infectious venereal disease, causative agent - Klebsiella granulomatis |
Klebsiella - causative agents of diseases of the genitourinary organs
Klebsiella, in particular Klebsiella pneumoniae, Klebsiella oxytoca, Klebsiella aerogenes,
can cause various diseases of the human genitourinary organs, in particular acute and chronic prostatitis, cystitis, pyelonephritis.
In chronic kidney disease, the titer of Klebsiella spp increases.
(Karpeeva Yu.S. et al.).
Klebsiella granulomatis
(oral
Calymmatobacterium granulomatis
) is the causative agent of donovanosis, transmitted sexually, and less commonly, through household contact. Donovanosis (other names: granuloma venereum or inguinal granuloma) is a long-term granulomatous lesion of the genitals and groin area with the formation of ulcers. They are found mainly in tropical and subtropical countries.
Other diseases caused by Klebsiella
Klebsiella variicola
causes bloodstream infections, and it is noted that the mortality rate from this species of Klebsiella is higher than from similar diseases.
caused by Klebsiella pneumoniae
. At the very end of the last century, Klebsiella caused 7 to 10% of all bloodstream infections.
Treatment of Klebsiella infections
Antibiotics are used to treat Klebsiella infections: ampicillin, aminoglycosides, tetracyclines, chloramphenicol, rifaximin, levofloxacin, norfloxacin, doxycycline and others, but recently antibiotic-resistant Klebsiella strains have become widespread. Also used are drugs whose active ingredients are bacteriophages: Bacteriophage Klebsiella pneumonia purified liquid
and
Bacteriophage Klebsiella polyvalent liquid purified, Pyobacteriophage
(combined drug; trade names of drugs: Pyobacteriophage complex liquid, Pyobacteriophage polyvalent, Piopolyphage, Sextaphage). Bacteriophages act selectively, only on Klebsiella (or, for combined bacteriophages, on a complex of bacteria), have no contraindications, but they are much less effective than antibiotics.
Klebsiella is resistant to nifuroxazide.
In case of excessive growth of Klebsiella pneumonia, Order of the Ministry of Health of the Russian Federation No. 231 dated June 9, 2003 On approval of the industry standard “Protocol for the management of patients. Intestinal dysbacteriosis”, the recommended bacteriophages are “Bacteriophage Klebsiella pneumoniae”, “Piobacteriophage polyvalent purified liquid” and “Bacteriophage Klebsiella polyvalent”. Bacteriophage is taken 3 times a day on an empty stomach 1 hour before meals. Single dose when taken orally:
- children under 6 months - 5 ml
- children from 6 months to 1 year - 10 ml
- children from 1 year to 3 years – 15 ml
- children from 3 to 7 years old - 20 ml
- patients aged 8 years and older - 30 ml
Instead of one oral dose, an enema once a day:
- children under 6 months - 10 ml
- children from 6 months to 1 year - 20 ml
- children from 1 year to 3 years – 30 ml
- children from 3 to 7 years old - 40 ml
- patients aged 8 years and older - 50 ml
Klebsiella is named after the German microbiologist Edwin Klebs (German: Edwin Klebs, 1834–1913).
Patient Materials
The GastroScan.ru website contains materials for patients on various aspects of gastroenterology:
- “Advice from doctors” in the “Patients” section of the site
- “Popular gastroenterology” in the “Literature” section
- “Popular gastroenterology” in the “Video” section
Back to section
How are tests for dysbacteriosis carried out in children?
The initial examination of stool is a coprogram. It can be called a review, since the result indicates the functional state (maturity) of digestion. In addition to identifying undigested food residues and an increase in fat components, the result shows:
- impurities of inflammatory elements (leukocytes, mucus growth);
- worm eggs;
- cystic form of parasites.
It takes one day to perform a coproscopy. An experienced laboratory technician needs a microscope with sufficient resolution.
Microflora is distinguished by:
- according to form;
- location of the core;
- the presence of flagella, pseudopods;
- possibilities of movement.
The second stage is bacteriological inoculation on a nutrient medium for growing colonies. This method allows you to significantly increase the concentration of micropathogens if their quantity in the stool is too small for microscopic detection.
Cultivation duration of at least five days
The laboratory can give a preliminary conclusion within a day, but the final decoding requires compliance with the research technology.
By the way, from a concentrated amount you can take a second analysis for microscopy; it is easier to examine microorganisms if they are concentrated in a small area. Biochemical studies of intestinal flora are based on the release of different types of organic acids by microorganisms. Based on their registration, the type and approximate number of bacteria are determined.
Bacteriological methods are more common due to the maximum information content, since they allow one to simultaneously identify the sensitivity of the identified pathogenic flora to antibiotics in order to prescribe the optimal drug for treatment. The result of the analysis depends on the parents' compliance with the rules for collecting stool.
Valuable properties of lactobacilli
Lactobacilli were discovered at the beginning of the twentieth century. Today science knows more than a hundred strains of such bacteria. The most common include cheese, lactic acid, Delbrück bacilli, as well as Bulgarian and acidophilus lactobacilli. They perform many useful functions:
- prevent the growth of pathogenic flora,
- improve metabolic processes,
- increase local immunity,
- stimulate the production of gastric juice,
- normalize the functioning of the gastrointestinal tract,
- destroy pathogens of ulcers and gastritis,
- reduce the risk of allergic reactions.
Lactobacilli with bifidobacteria form beneficial microflora. Their share in the intestines is about 98%.
How to correctly collect a stool sample from a baby?
To ensure that stool collection does not affect the reliability of the study, it is necessary to adhere to the recommendations for preparing a child for the test and the rules for collecting material.
For three to five days before stool collection, the baby is not allowed to:
- introduce new complementary foods;
- serve meat broths and dishes.
Use not recommended:
- any medications,
- rectal suppositories,
- laxatives.
If your child is prescribed permanent medications, you should consult your doctor about temporary withdrawal.
You need to try to choose the moment when the child has urinated first, so that the feces do not mix with urine
Additional tips:
- You should not give enemas if you are constipated.
- In the morning, the baby is given a regular toilet with thorough washing.
- The baby's feces are collected in a sterile container directly from the diaper.
- If the baby sits on the potty, then you need to first thoroughly treat the inner surface with soap, without disinfectants.
- The container can be a glass jar after washing and scalding with boiling water, but it must be tightly closed with a lid. It is best to purchase a ready-made special container with a spatula at the pharmacy.
- The volume of feces should be at least a teaspoon.
The collected material must be submitted to the laboratory within two hours. Storage in the refrigerator (not in the freezer) for 4 hours is allowed, but the analysis loses its reliability. This is due to the effect of oxygen from the air on some microorganisms, which quickly die.
The most accurate results are obtained when the child is in the hospital. A swab with a damp swab is taken for analysis. It is inserted shallowly into the anus and turned. If parents plan to check their infant’s stool for dysbacteriosis in a private medical institution, then they must first find out the laboratory’s work schedule.
What do the analysis results say?
You should not try to decipher the results yourself. The information is very specific, the indicators are unusual for clinical laboratories. The form shows the entire intestinal microflora by type and number. Quantification is carried out in CFU (colony-forming units) per gram of material (stool). This indicator reflects the potential of microorganisms to spread.
The quantity must be presented as a ten with an exponent or many zeros. For each type of microorganism, there are norms of lower and upper limits. Dysbacteriosis is judged by deviations. The presence or absence of pathogenic pathogens is marked (+) or (-).