Everyone experiences constipation sooner or later. Difficulties with bowel movements cause a lot of troubles, anxiety, and deterioration in well-being. To eliminate this problem, you can use medications and traditional medicine. Laxatives, the main active ingredient in which is lactulose, are very popular. They are in demand because they have a number of advantages:
- safety;
- soft impact;
- efficiency;
- a minimum set of unpleasant side effects.
In addition, the body does not get used to drugs of this group, so there is no need to fear that intestinal motor functions will decrease.
Features of lactulose-based laxatives
Duphalac is a drug that helps the intestines.
Lactulose is considered a synthetic disaccharide; such a substance does not exist in nature; it is a product of human industrial activity. The absorption of lactulose begins only in the large intestine.
Until this moment, the substance passes through the gastrointestinal tract without changes. In the large intestine, lactulose is broken down under the influence of lactic acid bacteria and bifidobacteria.
The product of this process is certain organic acids, the osmotic activity of which promotes rapid bowel movement.
Evacuation occurs due to the softening of stool. After all, the organic acids mentioned above promote the flow of fluid into the intestines.
The presence of fluid not only helps to moisten the intestinal contents, but also increases the volume of feces. Expanding in volume, they begin to put pressure on the intestinal walls, stimulating its motor functions. As a result, peristaltic contractions begin, which lead to quiet bowel movements.
This feature of the action of lactulose-based drugs helps to quickly get rid of constipation and ease bowel movements.
Emollients
Softening laxatives include oils, glycerin and sodium docusate3. They help relieve constipation by reducing the surface tension of stool, which facilitates the penetration of water and helps soften it8.
In general, the use of this group of laxatives during pregnancy is possible only for occasional constipation, since with long-term use, medications can accumulate in the intestinal wall and interfere with the absorption of fat-soluble vitamins2,3, the deficiency of which can negatively affect the formation of the fetus7.
to come back to the beginning
Reception features
The auxiliary agent of the drug is only water.
Another feature of all these drugs is the need to wait for the onset of the effect within a day or two.
The specific time is determined individually, it depends on the activity of bacteria populating the intestines. They must destroy the shell of the drugs so that the active substance begins to “work”.
The products mentioned above have one active ingredient - lactulose. However, Dinolak also contains simethicone. This active substance is an indispensable component for increased gas formation.
Use of the drug Lactulose
Hepatic encephalopathy - adults are prescribed 20-30 g orally 3-4 times a day. If necessary, administer 30 g hourly until a laxative effect is achieved. After achieving a laxative effect, the dose is reduced so that the frequency of bowel movements is 2-3 times a day. Children are prescribed 27–60 g orally in 3–4 doses. The dose is adjusted every 1–2 days until the stool has a soft consistency with a bowel movement frequency of 2–3 times a day. If the initial dose of lactulose causes diarrhea, it is reduced; if diarrhea persists, discontinue lactulose. Young children are prescribed 0.67–6.67 g of lactulose per day in 3–4 doses. It is prescribed rectally for patients in a state of hepatic coma or precomatosis; for adults, 300 ml of lactulose solution in 700 ml of water or isotonic saline solution is administered through a rectal balloon catheter and held for 30–60 minutes. Repeat every 4–6 hours if necessary. If the bowel movement is too rapid, the administration can be repeated. Constipation - adults are prescribed 15-30 ml orally (at the rate of 10 ml - 6.67 g of lactulose), increasing to 60 ml once a day if necessary. The effect develops after 24–48 hours. Children - 7.5 ml orally once a day, usually after breakfast. For elderly people - 15–30 ml orally once a day. If lactulose is prescribed to facilitate bowel movements in patients after hemorrhoidectomy, the dose is 15 ml orally 2 times a day from the day before surgery until 5 days after surgery. To speed up the evacuation of intestinal contents when barium suspension is retained after an X-ray examination, 5–10 ml is prescribed orally 2 times a day. Duration of use: 1–4 weeks.
Contraindications, side effects
The presence of sugars makes these drugs undesirable in the treatment of patients with diabetes. If a person suffers from liver failure, these medications must be prescribed with extreme caution. There are other contraindications, including the following:
- intestinal obstruction;
- possible inflammation of the appendix;
- disruptions in glucose metabolism, sugar intolerance;
- bleeding of unknown etiology;
- intolerance to components (allergy).
Bibliography
- Sokolova M.Yu. Constipation in pregnant women. Medical advice. 2013; 4:28-31. — URL: https://www.med-sovet.pro/jour/article/view/1073/1053#
- Antonenko O.M. Treatment and prevention of constipation in pregnant women. Medical advice. 2012; 1:52-55.
- Turchina S.V. Intestinal dysfunction in pregnant women: gestational constipation. Experimental and clinical gastroenterology. 2016; 132 (8): 88-92.
- Eremina E. Yu. Constipation in pregnant women. Medical alphabet 2015. T. 2. No. 15. P. 48-52. URL: https://www.elibrary.ru/item.asp?id=24896586
- Verghese TS, Futaba K, Latthe P. Constipation in pregnancy. The Obstetrician & Gynecologist 2015; 17:111–5.
- Longo SA, Moore RC, Canzoneri BJ, Robichaux A. Gastrointestinal Conditions during Pregnancy. Clin Colon Rectal Surg. 2010;23(2):80-89 - URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2967327/
- Van Tonningen M. Constipation during pregnancy. In: Schaefer C PP, Miller RK, editors. Drugs During Pregnancy and Lactation: Treatment Options and Risk Assessment. 2nd edn. London: Academic Press; 2007. - URL: https://pharmacy.frigoplus.co.rs/wp-content/uploads/2015/04/Drugs-During-Pregnancy-and-Lactation-2nd-Edition-Treatment-Options-and-Risk-Assessment .pdf
- Wald, A. (2003). Constipation, diarrhea, and symptomatic hemorrhoids during pregnancy. Gastroenterology Clinics of North America, 32(1), 309–322. — URL: https://pubmed.ncbi.nlm.nih.gov/12635420/
- Turchina M.S. The use of a complex laxative in the treatment of chronic constipation in patients who have been using irritating laxatives for a long time. Medical Council No5, 2022. - URL: https://www.med-sovet.pro/jour/article/viewFile/1796/1736
- Erdes S.I., Matsukatova B.O. Modern protocols for the management of children with constipation and experience with the use of osmotic laxatives in their treatment. Issues of modern pediatrics. 2014 - URL: https://cyberleninka.ru/article/n/epizodicheskie-i-hronicheskie-zapory-u-detey-poshagovyy-podhod-k-terapii-v-ramkah-iv-rimskih-kriteriev/viewer
- Instructions for use of the drug MICROLAX® // Registration number N011146/01 // RF GRLS. – URL: https://grls.rosminzdrav.ru/Grls_View_v2.aspx?routingGuid=f052fb31-5426-4bc1-958f-9fce793aa43f&t=(access date: 09.19.2021)
Normal microflora of the gastrointestinal tract and its functions
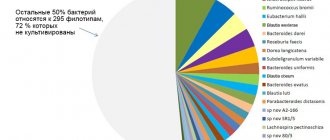
Normal human microflora is considered as a collection of many microbiocenoses that occupy numerous ecological niches (biotopes) on the skin and mucous membranes of all body cavities communicating with the external environment [3, 7]. The total number of microorganisms in the adult human body reaches 1015, which is more than 10 times the number of host cells [2]. There is no longer any doubt that the normal human microflora performs numerous functions to maintain homeostasis [1, 3, 7, 15, 19]. In this sense, the importance of microflora for humans is no less than the importance of any vital organ. The huge biomass, combined with the importance of its functions, allows us to consider the microflora as an independent organ [7]. More than 400 species of bacteria, representatives of 17 different families, live in the gastrointestinal tract (GIT) alone [3, 7]. The species and quantitative composition of microbial populations in different biotopes of the gastrointestinal tract is heterogeneous, but each biotope is an ecosystem, all components of which (macroorganism + microflora) perform mutually beneficial functions and are in a state of symbiosis, maintaining dynamic balance in this system.
Violation of the species and quantitative composition of microorganism populations and the growth of opportunistic microflora, leading to an imbalance in a given biotope, is called dysbacteriosis. The process may not end there, however. A change in the biocenosis in one biotope entails the movement of microorganisms into uncharacteristic biotopes and a decrease in colonization resistance of both individual biotopes and the entire human-microflora ecosystem. A manifestation of such microflora translocation can be excessive growth of bacteria in the small intestine, for example, with blind loop syndrome. Different biotopes of the gastrointestinal tract are unevenly populated by bacteria (see table).
The density of microflora is highest in the large intestine. About 400 species of microorganisms with a total biomass of about 1.5 kg live here [7]. Due to such a high population of microflora, the large intestine bears the greatest functional load compared to other biotopes of the gastrointestinal tract.
The main (resident) microflora of the colon consists of 90% bifidobacteria, bacteroides and lactobacilli. These bacteria are anaerobes. Resident microflora also include enterococcus and propionobacteria, but their share in the total microbial biomass is small [3]. The accompanying (facultative) microflora is represented mainly by aerobes: Escherichia, eubacteria, fusobacteria, cocci, a total of about 10%. Less than 1% accounts for numerous representatives of residual microflora, including aerobes and anaerobes. Thus, 90% of the colon microflora are anaerobes [1, 3].
Based on the nature of their metabolism, colon bacteria are divided into two groups: proteolytic and saccharolytic. Proteolytic species (bacteroides, proteas, Escherichia, clostridia, etc.) use the products of intestinal hydrolysis of proteins as a nutrient substrate and, as a result of their metabolism, form toxic substances, including aromatic amino acids, endogenous carcinogens, and sulfides. These substances contribute to the development of diarrhea, inflammation, and neoplasms. Most proteolytic microorganisms are opportunistic.
Saccharolytic flora (bifidobacteria, lactobacilli, some cocci, propionobacteria) use carbohydrate substrates entering the large intestine and polysaccharides of intestinal mucus. The metabolic functions performed by saccharolytic microbes are beneficial for the host organism, maintain homeostasis and neutralize the negative effects of proteolytic microflora.
The bulk of bacteria in the colon are bifidobacteria and lactobacilli. The dominance of these bacteria determines their greatest importance for humans. The beneficial functions of normal gastrointestinal microflora can be divided into 3 main groups: a) metabolic, b) protective and immune, c) antimutagenic and anticarcinogenic.
The metabolic functions of microflora are aimed at maintaining the optimal level of metabolic processes, digestive and motor functions of the gastrointestinal tract and include increased activity of gastrointestinal enzymes, regulation of lipid (cholesterol) levels, participation in the conjugation and recycling of bile acids, as well as the synthesis of:
- amino acids (arginine, tryptophan, tyrosine, cysteine, etc.);
- vitamins (groups B and K);
- short-chain fatty acids (SCFA), including acetic, butyric, lactic, propionic;
- biogenic amines (histamine, serotonin, piperidine, GABA);
- hormonally active substances (norepinephrine, steroids);
- antioxidants (vitamin E, glutathione).
The protective and immune functions of microflora are aimed at maintaining colonization resistance and antagonism towards pathogenic and opportunistic microorganisms. This is ensured by the antitoxic and sorption effects of microflora, as well as by the synthesis of:
- KZHK;
- other organic acids that regulate pH in the intestinal cavity;
- lysozyme (muramidase), hydrogen peroxide and antibiotic-like peptides-microcins, which have a wide spectrum of antibacterial activity and constitute a group of “natural” antibiotics [2, 3];
- secretory IgA in the human body.
In recent years, the immunomodulatory properties of normal intestinal microflora have been well studied. Bifidobacteria and lactobacilli affect various parts of the immune system, regulating nonspecific and specific cellular and humoral immunity, inducing the synthesis of immunoglobulins, lysozyme, interferon [3, 4, 17, 18].
The antimutagenic and anticarcinogenic activity of microflora is realized through the hydrolysis of metabolic products of proteins, lipids, carbohydrates, deconjugation of bile and hydroxylation of fatty acids, inactivation of histamine, xenobiotics and carcinogens. SCFAs also participate in the implementation of the anticarcinogenic potential of microflora.
The role of SCFA in the regulation of intestinal microbiocenoses and maintaining body homeostasis
A special role among microbial metabolites is played by SCFAs with a carbon chain length of 2 to 4 atoms (acetic, oily, lactic, propionic). SCFAs are the end products of metabolism of saccharolytic and proteolytic microflora and are used for an integral assessment of its condition [1]. The breakdown of SCFA produces a lot of energy, so they serve as an additional autonomous source of energy for the intestinal epithelium. Propionic acid regulates microcirculation in the mucous membrane and supports trophic processes in it, participates in gluconeogenesis and the synthesis of biogenic amines, and blocks the adhesion of pathogens. Butyric acid is an important regulator of proliferation and differentiation of the colon epithelium and thus determines the anticarcinogenic activity of microflora. Acetic acid provides an antimicrobial effect, regulates pH in the intestinal cavity and gastrointestinal motility. Lactic acid is involved mainly in the regulation of pH and local immunity and in lipogenesis. The lipid-lowering effect of microflora and vasoactive influences are provided by the metabolic effects of SCFA. Maintaining the pool of SCFAs in the colon by restoring normal microflora or through additional substrates for the formation of SCFAs (dietary fiber, oligosaccharides) is necessary for the normal functioning of the macroorganism, the prevention of atherosclerosis, colorectal cancer [14, 15].
Ways to correct microflora disorders
The species and quantitative composition of microflora and its functions can be disrupted under the influence of many exogenous and endogenous factors: natural and man-made toxins, medications (antibiotics, laxatives, sorbents, steroids, psychotropic drugs), stress. A huge negative role is played by the widespread use of diets for weight loss and the abuse of so-called methods of cleansing the body of toxins. Almost all chronic diseases of the gastrointestinal tract can lead to an imbalance of microflora due to a weakening of the protective properties of the mucous membranes.
Microflora disturbances are always secondary, so to correct them it is necessary, first of all, to eliminate the causes that cause them or to treat the underlying disease. If these measures are not enough, then three groups of agents with different mechanisms of action are used to restore the microflora: probiotics, prebiotics and synbiotics.
Probiotics are food products, medicines or dietary supplements in the form of monocultures or combined cultures based on living representatives of resident microflora (bifidobacteria, lactobacilli, enterococci) or non-pathogenic spore-forming microorganisms and saccharomycetes. Examples of probiotics: Baktisubtil ( B. cereus ), Sporobacterin (B. subtilis), Enterol.
Prebiotics are natural or synthetic agents of non-microbial origin. These are medicines, food products and dietary supplements that selectively stimulate the growth and/or metabolic activity of one or more types of microflora [12, 14]. Prebiotics are not absorbed in the small intestine and undergo bacterial fermentation in the colon. Most prebiotics are oligo- or polysaccharides (fiber). Oligosaccharides, in turn, can be natural (fructozooligosaccharide - inulin and galactoseoligosaccharide - lactitol) and synthetic (lactulose; drug - Duphalac). Prebiotics also include lysozyme, para-aminomethylbenzoic acid and calcium pantothenate.
Synbiotics are an optimal combination of probiotics and prebiotics. Synbiotics include Biovestin-lacto (B. bifidum, B. adolescentis, L. plantarum and bifidogenic factors), Maltodophilus (B. bifidum, L. acidiphilus, L. bulgaricus and maltodextrin), Bifido-bak (a complex of lactobacilli and bifidobacteria and fructose-oligosaccharides from Jerusalem artichoke), Laminolact (E. faecium L-3, amino acids, pectins, sea kale).
A separate group of drugs consists of microbial metabolites, such as Hilak forte.
Lactulose
The main group of prebiotics consists of oligosaccharides with 2–10 carbon atoms. Oligosaccharides are not hydrolyzed or absorbed in the small intestine because there are no enzymes in the brush border to break them down. Unchanged, they enter the large intestine, where they undergo bacterial fermentation. This group of prebiotics includes Duphalac (lactulose), a synthetic disaccharide consisting of fructose and galactose. Lactulose realizes its effect only in the large intestine. It is hydrolyzed mainly by bifidobacteria (to a lesser extent by lactobacilli), for which lactulose serves as a nutrient substrate, which leads to an increase in their biomass. Thus, this disaccharide is a bifido- and lactogenic prebiotic that normalizes the balance and restores the functions of microflora [12, 14, 15]. The end products of lactulose metabolism are formic acid and SCFA. Antagonism of bifidobacteria and lactobacilli and a decrease in pH in the intestinal cavity due to acidic metabolites leads to suppression of the growth of opportunistic proteolytic microflora. In addition to other biological effects (hypolipidemic, antiproliferative), SCFAs have an osmotic effect. The increase in microflora biomass and the osmotic effect of SCFA lead to an increase in stool volume, stimulation of motility and a corresponding laxative effect. Thus, lactulose combines the properties of a prebiotic and a mild osmotic laxative. These unique features can be successfully used for constipation of various origins, accompanied by microflora disorders. Thanks to the synthesis of SCFA and, above all, butyric acid, lactulose has an antiproliferative potential, which is realized in patients with constipation when taking the drug systematically.
The effect of lactulose on the growth of microorganisms in the colon in adult healthy volunteers was studied in a double-blind, controlled study using two methods: the traditional method of culturing intestinal microflora on selective media and the in situ hybridization method [20]. The use of molecular genetic analysis made it possible to assess the dynamics of both cultivated and uncultivated bacterial strains. To stimulate microbial growth, Duphalac was used at a dose of 10 g/day for a month. Microbiological examination of stool was carried out before the start of treatment, immediately after the end of taking the drug and 4 weeks after the end of its use. When cultivated on selective media, a significant increase in the growth of bifidobacteria, lactobacilli, enterococci, coliforms and an increase in the total number of aerobic bacteria was found in the group of subjects taking Duphalac. In a molecular genetic study, significant differences were identified only in relation to the growth of bifidobacteria. Thus, an increase in the growth of bifidobacteria when taking Duphalac was proven by two methods. The effect was more pronounced with an initially low content of bifidobacteria in the feces. Under the influence of treatment, there was a tendency towards a decrease in the number of clostridia.
Increased growth of bifidobacteria under the influence of lactulose was also proven in a 6-week study conducted by Bouchnic Y. [11]. Another test on healthy volunteers showed that when taking lactulose, the population density of bifidobacteria increases by 1.5 times compared to the initial level, and the population density of clostridia decreases in parallel by almost 3 times [10]. In the same study, when comparing the prebiotic effects of lactitol and lactulose, the advantage of the latter in stimulating the growth and enzymatic activity of bifidobacteria was shown [10].
The huge advantage of lactulose over probiotics is the possibility of its use together with antibacterial drugs in patients who need repeated courses of antibiotic therapy for other diseases (chronic nonspecific lung diseases, chronic pyelonephritis, etc.). In these cases, the prebiotic effect of lactulose is realized not only as a restorer in relation to the disturbed microbiocenosis of the colon, but also as a preventative, preventing the suppression of normal microflora. The effectiveness of probiotics in such cases is very low, which is quite natural, since the live strains of bacteria included in their composition are also negatively affected by antibiotics.
Lactulose also exhibits a preventive effect in the antibiotic therapy of intestinal infections. Moreover, it has been established that lactulose has an indirect antimicrobial effect due to the restoration of bifido- and lactobacilli and their antagonism against pathogens of intestinal infections. Thus, it has been shown that Duphalac, by stimulating the growth of bifidobacteria, leads to a decrease in pH in the colon by more than 2 times (due to acidic metabolites of normal microflora) and thereby inhibits the growth of salmonella, shigella and fungi of the genus Candida [6]. Lactulose suppresses the excretion of Salmonella, Shigella and Yersinia in feces during corresponding infections [9, 13, 16].
Recent studies have demonstrated disruption of the colon microflora in patients with hematologic malignancies during high-dose chemotherapy. The use of Duphalac led to an improvement in the microbial and metabolic status of the intestine. At the same time, the ratio of anaerobic and aerobic microflora was restored, as evidenced by the normalization of SCFA profiles in feces [5].
It is well known that normal microflora is involved in maintaining immunity. From the first days of life, intestinal microflora participates in the formation of the immune system [18]. On the contrary, disruption of the microbiocenosis of the gastrointestinal tract leads to perverted immune reactions, reduces the body’s resistance to viral and bacterial infections (not only intestinal), contributes to the development of atopic diseases, allergic dermatitis, neurodermatitis [3, 8, 17, 18].
Lactulose has been shown to restore cellular and humoral immunity [4]. As it turned out, its 2-week intake leads to a significant increase or complete normalization of the levels of IgA, T-helpers and T-suppressors in different categories of patients.
The powerful stimulating effect of lactulose on bacterial growth and metabolism has been successfully used in the treatment of hepatic encephalopathy. Reproducing acidophilus bacteria suppress the growth of proteolytic flora and absorb the ammonia and other nitrogen-containing toxins it produces, using them for protein synthesis [3]. Other prebiotics (including inulin and lactitol) have not found use in hepatic encephalopathy, apparently due to an insufficient stimulating effect on microbial growth.
Since Duphalac has the properties of a prebiotic and osmotic laxative, the choice of dose of the drug depends on the disease and the purpose for which it is used. Treatment of hepatic encephalopathy requires a high dose, which is 60–100 ml/day (Duphalac release form is syrup), which corresponds to approximately 40–70 g of lactulose. To achieve a laxative effect, the dose is on average 15–40 ml/day (may be higher in the elderly). The dose of Duphalac as a prebiotic is lower than laxative and is selected in such a way as not to change the frequency of bowel movements. Most studies of the prebiotic effect of lactulose used a dose of no more than 10 g/day [10, 20]. The recommended dose of Duphalac (3, 5 or 10 ml/day) is selected individually. The correct selection of the dose ensures that only the prebiotic or complex prebiotic and laxative effect of Duphalac is manifested, which allows it to be used for various purposes both for constipation and diarrhea caused by a violation of the microflora of the colon.