The gallbladder is one of the organs from which you can expect not entirely pleasant surprises in the form of severe pain in the right hypochondrium. It functions as a reservoir for collecting and storing bile, which aids in digestion. Accumulation and stagnation (cholestasis) of this fluid causes changes in its composition and the formation of stones. This is usually due to:
- hormonal disorders;
- anatomical structural abnormalities;
- emotional and nervous stress;
- errors in nutrition - frequent overeating, consumption of fatty or fried foods, smoked foods;
- high cholesterol;
- taking certain medications;
- hereditary predisposition.
In what situations is the gall bladder removed?
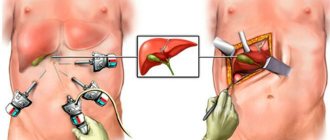
When an ultrasound examination reveals sand or small stones that do not cause attacks and can be crushed and dissolved, there is no need for surgical intervention. The indication for manipulation is damage to the organ itself. Most often, laparoscopic cholecystectomy is performed - a minimally invasive and low-traumatic operation using special instruments and modern technology. Pathologies for which it is performed:
- cholelithiasis leading to the formation of stones. During the period of inflammation, a pronounced pain syndrome occurs due to stones getting stuck, causing spasms of the bile ducts;
- acute cholecystitis is a complication of cholelithiasis that can lead to serious consequences in the form of sepsis (blood poisoning), damage and rupture of the walls of the gallbladder, followed by peritonitis;
- polyposis – benign growths of the mucous membrane, prone to malignancy (malignancy). Laparoscopy will be required if they increase in size, their number is more than two units, their diameter exceeds 10 mm, or the patient has clinical signs that worsen the quality of life;
- cholesterosis, associated with a slowdown in lipid metabolism in the body, which leads to the accumulation of cholesterol deposits on the walls of the organ and functional disorders. Surgery is necessary when diet and drug therapy do not produce positive results.
Medications after cholecystectomy
The gallbladder synthesizes bile, which, when it enters the duodenum, promotes the production of gastric juice. After cholecystectomy, this process is disrupted, which leads to malfunctions of the digestive system. To eliminate the lack of bile, abdominal pain, and attacks of nausea, medications are prescribed. Main groups of drugs:
- enzymes;
- antispasmodics;
- choleretic drugs.
Some medications must be taken in courses of 2-6 months. Other drugs - throughout life. Be sure to follow the dosage and other recommendations for taking medications.
Immediately after surgery, a course of antibiotics is prescribed for 7-10 days. This helps to avoid the development of purulent and inflammatory processes. Effective drugs - Furazolidone, Cefazolin, Biseptol.
Medicines with enzymes
These drugs help normalize the functioning of the digestive system when there is insufficient bile. These medications help break down proteins, fats and carbohydrates and promote better absorption of nutrients. Additionally, the products have a mild analgesic effect. List of enzymes:
- Mezim
. Contains pancreatin, amylase, lipase, proteases. Helps replenish pancreatic enzyme deficiency, improves digestion, prevents flatulence and intestinal disorders. Dosage - 1-2 tablets or capsules with meals. Do not chew, drink 200 ml of water. - Festal
. Active components - pancreatin, hemicellulose, bile components. The medicine has a choleretic effect, normalizes the functioning of the pancreas and liver. Take 1-2 tablets three times a day during or immediately after meals. - Creon
. The main ingredient is pancreatin in various dosages. The medicine eliminates pancreatic enzyme deficiency. Take capsules with meals. The dose depends on the severity of the postoperative condition.
Enzymes rarely cause adverse reactions. The most common concerns are lacrimation and rash, and disorders of the digestive system. Medicines should not be taken in case of hypersensitivity, acute or chronic pancreatitis in the acute stage, intestinal obstruction, severe liver pathologies.
Antispasmodic drugs
Promotes relaxation of smooth muscles, eliminates spasms in the bile ducts. Most often prescribed in tablets, in case of severe pain - in the form of intramuscular injections. The medications begin to work within 20 minutes. Name of drugs:
- No-shpa
. The main active ingredient is drotaverine. Daily dosage: 3-6 tablets, divided into 2-3 doses. Eating does not affect the effectiveness of the medicine. Possible adverse reactions are decreased blood pressure, sleep disturbances, headache, dyspeptic disorders. - Mebeverine
- antispasmodic and myotropic agent. Take the tablets 20 minutes before meals. Daily dosage: 400 mg, divided into 2-4 doses. Side effects include hives, swelling, constipation or diarrhea. - Duspatalin
- quickly eliminates spasms and colic. Take 1 capsule whole morning and evening, 20 minutes before meals. During treatment, attacks of dizziness and allergic reactions rarely occur.
Antispasmodics should not be taken if you are hypersensitive to the components of the drug. The main contraindications are severe forms of renal and liver failure, low cardiac output syndrome. You can take medications regularly, or only when pain occurs.
Choleretic drugs
Prescribed after cholecystectomy to protect the liver from bile stagnation and prevent the development of inflammatory processes. Additionally, the drugs prevent diarrhea and bloating and promote the absorption of beneficial microelements from food. Medicines have a small number of contraindications and side effects.
Allohol
A product based on dry cattle bile, nettle and garlic extract. Contains activated carbon as a sorbent. This substance prevents the development of rotting and fermentation processes in the intestines. Allochol has a complex effect:
- normalizes the functioning of the liver and intestines;
- improves the secretion and outflow of bile;
- eliminates flatulence, prevents bloating;
- reduces pain in the right hypochondrium.
Take 2 tablets three times a day after meals. The minimum course is 3-4 weeks. You can continue taking it after a three-month break.
Improvement in condition is observed 5-8 days after the start of treatment.
Contraindications: acute hepatitis, bile duct obstruction, subacute and acute liver dystrophy. You should not take the medicine for acute pancreatitis or ulcerative lesions of the gastrointestinal tract. Possible side effects are various allergic reactions, diarrhea.
Holenzym and Holosas
Cholenzym contains powder from the mucous membrane of the small intestines and pancreas of animals, and dry bile. The medicine has a choleretic effect, improves the digestion process, increases the level of bile acids, and reduces cholesterol. During treatment, it is possible that allergic reactions such as watery eyes, sneezing, rashes and redness of the skin may occur.
Dosage - 1 tablet 2-3 times a day. Take after meals without chewing, with plenty of liquid. Duration of therapy is 1-2 months.
With prolonged use of Cholenzym, iron absorption decreases.
The drug should not be taken if any of the components are intolerant. The main contraindications are the acute stage of pancreatitis or the period of exacerbation of the chronic form of the disease, obstructive jaundice, peptic ulcer, acute hepatitis. The medicine can be taken by pregnant women.
Holosas syrup contains rosehip extract. An effective choleretic, anti-inflammatory and hepatoprotective agent, saturates the body with vitamins A, C, E, P, group B. The medicine activates nonspecific immunity and takes part in the metabolism of carbohydrates.
Dosage - 1 tsp. 2-3 times a day half an hour before meals. Holosas should not be taken if you have allergies, and with caution if you have diabetes. During treatment, various allergic reactions may occur.
Means to improve liver function
Hepatoprotectors prevent the formation of stones in the bile ducts. Medicines effectively help in the postoperative period and improve the general condition of the body. Additionally, they have an antispasmodic, choleretic effect and protect the liver.
The most effective and safe hepatoprotectors are based on milk thistle extract.
Hepatoprotectors based on ursodeoxycholic acid dissolve gallstones and reduce cholesterol levels. Medicines prevent stagnation of bile and enhance the excretion of secretions. Additionally, they stimulate the secretion and renewal of T-lymphocytes.
Karsil
The medicine contains dry extract of spotted milk thistle fruits. The drug has a complex effect - it has a beneficial effect on the functioning of the liver, urinary and digestive systems, removes toxins, and normalizes the composition of bile. During treatment, appetite and general well-being improve, and dyspeptic disorders disappear.
Take 1-2 tablets three times a day, drink 100-150 ml of water. Eating does not affect the absorption of active substances. The average course duration is 3 months.
Karsil reduces the effectiveness of oral contraceptives and enhances the effect of anticoagulants and antihistamines.
Karsil has practically no contraindications; the medicine should not be taken in case of allergies or acute intoxication of any origin.
Adverse reactions - nausea, itching and rash, disturbances in the functioning of the vestibular system. They occur predominantly in people with hypersensitivity.
Essentiale Forte N and Enerliv
The capsules contain polyunsaturated fatty acids, which accelerate the recovery process of hepatocytes. Phospholipids in soybeans regulate fat metabolism, reduce the viscosity of bile, thereby accelerating the flow of secretions into the intestines. The medicine is prescribed to prevent the development of liver pathologies after removal of the gallbladder. Both drugs have similar therapeutic effects and rules of administration.
Dosage - 2 capsules three times a day. Take with meals, with plenty of water. The duration of the course of treatment is unlimited, but you need to take the medicine for at least 2 weeks.
Medicines based on bean phospholipids should not be taken if you are allergic to peanuts.
The main contraindication is increased susceptibility to the components of the drug, a history of antiphospholipid syndrome.
The drugs are well tolerated. Rarely during treatment, abdominal discomfort and diarrhea, allergic reactions, and bleeding in the middle of the cycle in women occur. Available analogues are Fosfontiale.
Ursosan, Urdoxa, Ursofalk
Preparations based on ursodeoxycholic acid. They protect liver cells, stimulate the flow of bile, and have an immunomodulatory effect. Additionally, medications dissolve cholesterol gallstones and prevent the formation of new stones. Admission rules:
- optimal dosage - 10 mg/kg;
- take the medicine once a day before bedtime;
- Duration of therapy is at least 6 months.
Contraindications: hypersensitivity, chronic hepatitis and pancreatitis, liver cirrhosis. Ursosan and analogues should not be taken for diseases of the bile ducts, inflammatory processes in the small and large intestines, renal and liver failure. Possible side effects are vomiting, nausea, stool upset, allergic reactions. Sometimes during treatment there is an exacerbation of psoriasis, and reversible alopecia develops. Some antacids reduce the degree of absorption of the active substances of the drug.
Consequences of deletion
According to statistics, in 90% of cases, patients are discharged from the hospital without presenting serious complaints. However, with the loss of the gallbladder, the transportation of bile is disrupted; the function of its storage and delivery to the duodenum falls entirely on the liver. In new anatomical conditions, there is a risk of stone formation in the hepatic ducts and the need for repeated surgery, installation of a stent, and drainage. To prevent this, it is imperative:
- visit a gastroenterologist or hepatologist once every 6-12 months to examine the hepatobiliary region;
- do an ultrasound of the abdominal organs annually;
- in accordance with the doctor’s prescriptions, regularly or in courses, take antispasmodics, drugs to thin bile and improve digestion.
Planned visits to specialists will also be needed because changes are also occurring in the work of other organs of the gastrointestinal tract.
In some cases, after the intervention, people may experience discomfort or pain in the right hypochondrium, which goes away on its own within a week. If this continues longer, then most likely the pathology is associated with postcholecystectomy syndrome (PCES), characterized by bacterial overgrowth, duodenogastric reflux, duodenal obstruction, etc. After making a diagnosis and determining the mechanism of development of the disease, treatment consists of diet and pharmacotherapy: anti-inflammatory and antibacterial agents, enzymes, motor regulators.
What do you need to remember?
Cholecystectomy is not a death sentence; you can live without a gallbladder. The quality and life expectancy after surgery are affected by nutrition and psychological attitude. To support the normal functioning of the digestive system, it is necessary to take medications - enzymes, hepatoprotectors, choleretic agents.
Diet after gallbladder removal is necessary. With improper and irregular nutrition, bile stagnates. As a result, inflammatory processes develop, stones form, and the functioning of the intestines, liver, and pancreas is disrupted.
Recovery in the first days after surgery
After laparoscopy, the person is under the supervision of medical staff for two days. If any unpleasant symptoms appear, they are easily relieved. The most common concerns:
- bitterness in the mouth;
- nausea;
- change in taste;
- feeling of heaviness in the right hypochondrium;
- bloating;
- diarrhea.
With strict adherence to the doctor’s recommendations, improvement in well-being is noted within a week, and full recovery takes six months. After some time, the entire body is rebuilt, but limitations still remain.
Further rehabilitation after gallbladder removal
To quickly return to your normal lifestyle and prevent the development of complications, you need to do the following within a month:
- follow the prescribed diet;
- avoid overheating, hypothermia, increased physical activity, lifting weights over 3 kg;
- refuse to visit baths, saunas, solariums, swimming and relaxing on the beach;
- exclude sexual contacts;
- refrain from drinking alcohol;
- perform light exercises every day without straining the abdominal muscles;
- use a belt-bandage made of elastic fabric.
After 7 days, you can go for half-hour leisurely walks.
The action of a unique technique used in our clinic by Dr. Borisov, called Selective Chronophototherapy (SPT), which is based on photodynamic therapy, is capable of activating a cascade of biochemical and cellular reactions to regulate the level of immune status indicators, demonstrates excellent results both when used independently and in combination with other methods. This significantly reduces the risk of relapse of cancer and the severity of side effects from cytostatic agents, while enhancing their effect on the affected cells.
Dr. Borisov’s gentle technique can be used repeatedly; a course of treatment is recommended. The number of procedures is regulated by the treatment regimen and achievement of the desired result.
We recommend taking VIALIFE capsules or VIALIFE solution, because they contain the highest possible concentration of chlorophyll, which:
- strengthens the immune system;
- enhances cell regeneration;
- saturates tissues with oxygen;
- has antioxidant, anti-inflammatory, detoxifying effects.
Nutrition
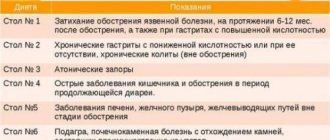
Since after the removal of the bile, the body is slowly rebuilt, which directly affects the functioning of the digestive tract, you will have to follow a special diet “table No. 5”, the purpose of which is to reduce the load on the liver and normalize the functions of the biliary system. It maintains optimal nutritional levels and satisfies the body's energy needs. The diet includes the required amount of proteins and carbohydrates, while reducing the amount of fat consumed.
The main principle is frequent, split meals every three hours in small portions. Food should be warm and taken at the same time. What is allowed:
- meat – lean beef, chicken, rabbit;
- fish - hake, cod, pike perch;
- cereals – rolled oats, rice, buckwheat, durum wheat pasta;
- low-fat fermented milk products;
- egg omelet or soft-boiled eggs;
- boiled, steamed, baked vegetables;
- fruits – sweet and semi-sweet apples, pears, bananas;
- desserts - puddings, casseroles, jellies, dried fruits, honey;
- drinks - pure water, non-acidic juices, jelly, compotes, fruit drinks, herbal decoctions.
No more than twice a week you can allow yesterday's bread, crispbread, crackers. Prohibited:
- fried, smoked, spicy foods and sauces;
- fast food, canned food, semi-finished products;
- fatty meats and fish, lard, offal;
- sausages;
- animal oil;
- pearl barley, millet, corn grains;
- rich soups with meat and fish broths;
- mushrooms, garlic, ginger, legumes;
- yeast baked goods, black bread;
- carbonated drinks;
- sour berries, citrus fruits.
This is a gentle and healthy diet, but its disadvantage is that some dishes may seem bland at first. However, they will bring maximum benefit, since they are easily digested, do not create a burden on the gastrointestinal tract and stimulate its normal activity.
Over time, the body physiologically fully adapts, and then the diet gradually changes towards the usual one used before cholecystectomy. The process must be controlled, the indicator will be good health and normal laboratory test results.
Dietary recommendations after cholecystectomy
After removal of the gallbladder, the consequences and life largely depend on nutrition. Men and women after cholecystectomy need to adhere to a special diet throughout their lives. Is it possible to eat pumpkin after removal of the gallbladder, as well as other vegetables and fruits? The doctor will tell you the basic rules for eating. The purpose of proper nutrition is to prevent stagnation of bile in the ducts. Basic rules of the diet for a removed gallbladder:
- Eat 5-6 times a day at regular intervals.
- Portions should be small so as not to cause constipation and heaviness in the stomach. The optimal size is about a handful.
- Peel any fruit before consumption, especially in the first month after cholecystectomy.
- It is necessary to completely exclude animal fats from the diet - bile is required to break them down.
- Food should not be very cold or hot - a temperature difference may cause a spasm in the bile ducts.
- The daily calorie intake is 2-3 thousand kcal.
- Dinner should be light, at least 2 hours before bedtime.
The basis of the diet is boiled, stewed and steamed dishes; there should be no half-raw foods. If the gallbladder has been removed, you should follow table number 5 in your diet. This will avoid the development of complications, and the body will not suffer from a lack of nutrients. After 1-1.5 years, a transition to table No. 15 is allowed.
Nutrition rules in the first week
In the first week after surgery, nutrition is aimed at adapting the body to new conditions. The basis of the diet is liquid food, it is easiest to digest and does not burden the digestive system. On the first day after cholecystectomy, you should not drink or eat.
Diet for the first week:
- Second day
. You can drink warm unsweetened rosehip decoction and alkaline water without carbon in small portions. The daily volume of liquid is up to 1 liter. Low-fat kefir, jelly, compote and tea without sugar are introduced into the diet. - 3-5 day
. You are allowed to eat mashed potatoes, boiled fish pate, pureed vegetable soups. Take food at intervals of 3-4 hours. Serving size: 150 g. - 6-7 day
. Dry bread, porridge made from crushed cereals with water or milk, steamed cutlets or meatballs, low-fat fermented milk products, and pureed vegetables are added to the menu.
To improve liver function, you must definitely drink medicinal mineral water - Narzan, Essentuki, Borjomi. Before use, be sure to release the gas and warm it up a little. Drink 30-50 ml half an hour before meals 3-4 times a day. The duration of the course is 4 weeks, then you need to take a break for 2-3 months.
Permitted and prohibited products
Solid foods can be consumed 2 weeks after cholecystectomy. New foods should be introduced into the diet gradually, no more than 1-2 per day, to monitor the body’s reaction. Nausea, diarrhea, pain and bloating in the abdomen indicate intolerance to any food.
| Prohibited | Allowed |
|
|
If it is difficult to completely give up sweets, you can eat marshmallows, marmalade, honey, and biscuits in small quantities. But only in the first half of the day. Drink at least 2 liters of water per day, not counting other liquids.
You can drink liquid at least 30 minutes after eating.
The most useful vegetables after removal of the gallbladder are pumpkin, carrots, zucchini, potatoes, and beets. Natural fermented milk products must be present in the diet. But you should choose products of medium fat content - when consuming completely low-fat kefir, yogurt, and yogurt, calcium is not absorbed.
Sample menu for the day
The first time after removal of the gallbladder, it can be difficult to switch to proper nutrition. To simplify the task, you need to immediately create a menu for the week. This way you can monitor the variety of your diet and calculate its calorie content.
Healthy meal options:
| Immediately after waking up |
|
| Breakfast |
|
| Dinner |
|
| Afternoon snack | Milk or fermented milk products, fruit jelly. |
| Dinner |
|
During the day you can drink milk, tea, juice, purified or medicinal water. Before going to bed, you can drink a glass of kefir or yogurt. Fermented milk products at night are very useful if you are prone to constipation.
Prognosis and recommended lifestyle
Every person undergoing surgery is concerned about the question of how his future existence will turn out. Will it be the same as before, or will it become less complete due to restrictions? It all depends on gender and age, the patient’s health status, the rate of tissue healing, and the presence of chronic diseases. Not only proper nutrition is of great importance, but also reasonable physical activity. Spending a long time in a chair or lying on the sofa leads to obesity and causes stagnation of bile. Gentle exercises, walks in the fresh air, measured work at home and in the garden help to increase its circulation. Short swimming in the pool several times a week improves metabolism and relaxes the spine. If you or your loved ones need professional support in rehabilitation after surgery, our specialists will help with this. Sign up for a free initial consultation to discuss further steps with your doctor that will make it possible to avoid post-operative complications and re-formation of stones, as well as reduce rehabilitation time.