Digestion in the small intestine
Well-processed food gruel (chyme) in the stomach passes through the valve into the small intestine, which consists of three parts, the most important of which is the duodenum.
It is here that complete digestion of all food nutrients occurs under the influence of intestinal secretions, including pancreatic juices, bile and secretions of the intestine itself. People can live without a stomach (as happens after appropriate operations) on a strict diet, but they cannot live at all without this important part of the small intestine. Absorption of the foods we eat, broken down (hydrolyzed) to their final components (amino acids, fatty acids, glucose and other macro and micro molecules), occurs in two other parts of the small intestine. The inner layer lining them, the villous epithelium, has a total surface area many times greater than the size of the intestine itself (the lumen of which is as thick as a finger). This structure of this amazing layer of the intestine is designed for the passage of final monomers (absorption) into the intestinal space - into the blood and lymph (blood and lymphatic vessels pass inside each “papilla”), from where they rush to the liver, spread throughout the body and are embedded in its cells . Let's return to the processes occurring in the duodenum, which is rightly called the “brain” of digestion and not only digestion... This section of the intestine is also actively involved in the hormonal regulation of many processes in the body, in providing immune protection and many others, which we will talk about talk in further topics.
There should be an alkaline environment in the small intestine, but acidic chyme comes from the stomach, what happens? Abundant secretion of intestinal juices, pancreatic secretions and bile containing bicarbonates into the lumen of the duodenum can quickly neutralize the incoming acid in just 16 seconds (from 1.5 to 2.5 liters of each secretion is released during the day). Thus, the necessary slightly alkaline environment is created in the intestines, in which pancreatic enzymes are activated.
The pancreas is a vital organ. It not only performs a secretory digestive function, but also produces the hormones insulin and glucagon, which are not secreted into the intestinal lumen, but immediately enter the blood and play a critical role in the regulation of sugar in the body.
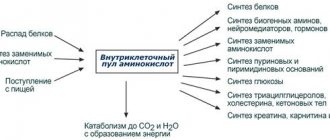
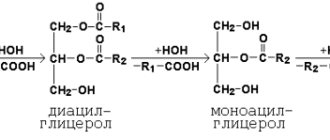
Pancreatic juice is rich in enzymes that hydrolyze (break down) proteins, fats and carbohydrates. Proteolytic enzymes (trypsin, chymotrypsin, elastase, etc.) break down the internal bonds of the protein molecule to form amino acids and low molecular weight peptides that can pass through the villous layer of the small intestine into the blood. Enzymatic hydrolysis of fats is carried out by pancreatic lipase, phospholipase, and cholesterol esterase. But these enzymes can only work with emulsified fats (emulsification is the splitting of large fat molecules into smaller ones by bile, preparation for processing by lipases). The final product of lipid hydrolysis is fatty acids, which then enter the lymphatic vessels in the intestinal space.
The breakdown of dietary carbohydrates (starches, sucrose, lactose), which began in the oral cavity, continues in the small intestine under the action of pancreatic enzymes in a slightly alkaline environment to the final monosaccharides (glucose, fructose, galactose).
Absorption is the process of transferring the products of hydrolysis of nutrients from the cavity of the gastrointestinal tract into the blood, lymph and intercellular space. As I mentioned, enzymes enter the intestinal lumen in an inactive form. Why? Because, if they were initially active, they would digest the gland itself, which is what happens in acute pancreatitis (from the word “pancreas” - pancreas), which is accompanied by unbearable pain and requires immediate medical attention. Fortunately, chronic inflammation of the pancreas is more common, occurring as a result of digestive disorders, resulting in insufficient production of enzymes, which can be regulated by diets and atraumatic (non-drug) treatment.
Let's pay a little more attention to the role of bile. Bile is produced by the liver, this process continues continuously both day and night (1-2 liters are produced per day), but it intensifies during meals and is stimulated by certain chemical compounds (mediators) and hormones. I will mention only one substance - cholecystokinin-pancreozymin - an important stimulator of bile secretion, produced by the cells of the small intestine and carried through the bloodstream to the liver. With inflammatory changes in the intestines, this hormone may not be produced. Of the products, the main stimulants of bile secretion are: oils (fats), egg yolks (contain bile acids), milk, meat, bread, magnesium sulfate. Through the bile ducts of the liver, bile enters the common bile duct, where along the way it can accumulate in the gallbladder (up to 50 ml), in which water is reabsorbed, leading to thickening of the bile (another reason to drink enough water). If the bile is thick, and there are also anatomical features of the location of the gallbladder (kinks, torsions), then its movement is difficult, which can lead to stagnation and the formation of stones.
What does bile contain? Bile acids; bile pigments (bilirubin); cholesterol and lecithin; slime; drug metabolites (if they are taken, the liver cleanses the body and removes them with bile). Bile must be sterile and have a pH of 7.8–8.2 (the alkaline environment allows it to have a bactericidal effect).
Functions of bile: emulsification of fats (preparation for further hydrolysis by pancreatic enzymes); dissolution of hydrolysis products (which ensures their absorption in the small intestine); increased activity of intestinal and pancreatic enzymes; ensuring the absorption of fat-soluble vitamins (A, D, E), cholesterol, calcium salts; bactericidal effect on putrefactive flora; stimulation of the processes of bile formation and excretion, motor and secretory activity; participation in programmed death and renewal of erythrocytes (apoptosis and proliferation of erythrocytes); removal of toxins.
How many functions it performs! What if, due to inflammation, thickening and other reasons, the secretion of bile is disrupted? What if the liver (the multifunctionality of which should be highlighted as a separate topic), with its toxic loads and disorders, does not produce enough bile? How many digestive mechanisms fail! And we, for the most part, do not want to pay attention to the signals with which the body notifies us about digestive disorders: increased gas formation, bloating after eating, belching, heartburn, bad breath, smell of discharge, pain and cramps, nausea and vomiting, and many other manifestations of malabsorption of food, the cause of which must be found and corrected, and not “suppressed” the symptoms by taking medications.
Anatomy of Human Bile – information:
Bile (Latin bilis, ancient Greek χολή) is a yellow, brown or greenish, bitter-tasting liquid with a specific odor, secreted by the liver and accumulated in the gallbladder.
Bile is secreted by hepatocytes - liver cells. Bile collects in the bile ducts of the liver, and from there, through the common bile duct, it enters the gallbladder and the duodenum, where it participates in the digestive processes.
The gallbladder acts as a reservoir, the use of which allows the duodenum to be supplied with the maximum amount of bile during the active digestive phase, when the intestine is filled with food partially digested in the stomach. Bile secreted by the liver (part of it goes directly to the duodenum) is called “hepatic” (or “young”), and bile secreted by the gallbladder is called “vesical” (or “mature”).
A person produces 1000-1800 ml of bile per day (about 15 ml per 1 kg of body weight). The process of bile formation - bile secretion (choleresis) - occurs continuously, and the flow of bile into the duodenum - bile secretion (cholekinesis) - occurs periodically, mainly in connection with food intake. On an empty stomach, almost no bile enters the intestines; it is sent to the gallbladder, where, when deposited, it concentrates and slightly changes its composition, so it is customary to talk about two types of bile - hepatic and cystic.
The doctrine of bile
In ancient times, bile was considered a liquid no less important than blood. But if blood for the ancients was the bearer of the soul, then bile was the bearer of character. It was believed that the abundance of light bile in the body makes a person unbalanced and impetuous. Such people were called choleric. But an excess of dark bile supposedly gives rise to a depressed, gloomy mood, characteristic of melancholic people. Please note: both words contain the syllable “chol”, translated from Greek chole means bile. Later it turned out that the nature of light and dark bile is the same, and neither one nor the other has anything to do with a person’s character (although irritable, sarcastic people are still called bile), but has a direct relationship with digestion.
Regardless of whether a person is good-natured or evil, his liver cells - hepatocytes - produce about a liter of bile per day. These cells are intertwined with blood and bile capillaries. Through the wall of blood vessels, the “raw materials” necessary for the production of bile enter the hepatocyte from the blood. Mineral salts, vitamins, proteins, microelements, and water are used to produce this bitter greenish-yellow liquid. Having processed all these components, hepatocytes secrete bile into the bile capillary. More recently, it has become known that specialized cells of the intrahepatic bile ducts also contribute to bile formation: as bile moves through these ducts to the common bile duct, some amino acids, trace elements, vitamins, and water are added to it. Bile passes directly from the liver into the duodenum through the common bile duct only during the digestion of food. When the intestines are empty, the bile duct closes, and the bile, which the liver secretes continuously, goes through the cystic duct, which branches off from the common bile duct, into the gallbladder. This reservoir has the shape of an elongated pear 8-12 centimeters long and holds approximately 40-60 cubic centimeters of bile.
In the gallbladder, bile becomes thicker, more concentrated, and takes on a darker color than that just produced by the liver. I. P. Pavlov believed that the main role of bile is to replace gastric digestion with intestinal digestion, destroying the effect of pepsin (the most important enzyme of gastric juice) as a dangerous agent for pancreatic enzymes, and that it is extremely beneficial for the enzymes of pancreatic juice involved in the digestion of lipids. When food that has already been partially processed there enters the duodenum from the stomach, pancreatic juice and bile flow here. Moreover, to the bile that flows evenly and slowly directly from the liver, bile from the gallbladder is also added.
Composition of human bile
Bile is not only a secretion, but also an excrement. It contains various endogenous and exogenous substances. This determines the complexity of the bile composition. Bile contains proteins, amino acids, vitamins and other substances. Bile has little enzymatic activity; The pH of liver bile is 7.3-8.0. When passing through the biliary tract and being in the gallbladder, liquid and transparent golden-yellow liver bile (relative density 1.008-1.015) is concentrated (water and mineral salts are absorbed), mucin of the bile ducts and bladder is added to it, and the bile becomes dark, viscous , its relative density increases (1.026-1.048) and pH decreases (6.0-7.0) due to the formation of bile salts and absorption of bicarbonates. The main amount of bile acids and their salts is contained in bile in the form of compounds with glycocol and taurine. Human bile contains about 80% glycocholic acids and about 20% taurocholic acids. Eating foods rich in carbohydrates increases the content of glycocholic acids; if protein predominates in the diet, the content of taurocholic acids increases.
Bile acids and their salts determine the basic properties of bile as a digestive secretion. Bile pigments are products of the breakdown of hemoglobin and other porphyrin derivatives excreted by the liver. The main bile pigment in humans is bilirubin, a red-yellow pigment that gives liver bile its characteristic color. Another pigment, biliverdin (green), is found in trace amounts in human bile, and its appearance in the intestines is due to the oxidation of bilirubin. Bile contains a complex lipoprotein compound, which includes phospholipids, bile acids, cholesterol, protein and bilirubin. This compound plays an important role in the transport of lipids into the intestine and takes part in the hepatic-intestinal circulation and general metabolism of the body.
Bile consists of three fractions . Two of them are formed by hepatocytes, the third by epithelial cells of the bile ducts. Of the total volume of bile in humans, the first two fractions account for 75%, the third - 25%. The formation of the first fraction is associated, but the second is not directly related to the formation of bile acids. The formation of the third fraction of bile is determined by the ability of the epithelial cells of the ducts to secrete fluid with a sufficiently high content of bicarbonates and chlorine, to reabsorb water and electrolytes from the tubular bile.
The main component of bile, bile acids, are synthesized in hepatocytes. About 85-90% of bile acids released into the intestine as part of bile are absorbed into the blood from the small intestine. Absorbed bile acids are transported in the blood through the portal vein to the liver and are included in the composition of bile. The remaining 10-15% of bile acids are excreted from the body mainly in feces. This loss of bile acids is replenished by their synthesis in hepatocytes. In general, the formation of bile occurs through active and passive transport of substances from the blood through cells and intercellular contacts (water, glucose, creatinine, electrolytes, vitamins, hormones, etc.), active secretion of bile components (bile acids) by hepatocytes and reabsorption of water and a number of substances from bile capillaries, ducts and gallbladder. The leading role in the formation of bile belongs to secretion.
Functions of bile The participation of bile in digestion is diverse. Bile emulsifies fats, increasing the surface area on which they are hydrolyzed by lipase; dissolves lipid hydrolysis products, promotes their absorption and resynthesis of triglycerides in enterocytes; increases the activity of pancreatic and intestinal enzymes, especially lipase. When bile is excluded from digestion, the process of digestion and absorption of fats and other lipid substances is disrupted. Bile enhances the hydrolysis and absorption of proteins and carbohydrates. Bile also plays a regulatory role, being a stimulator of bile formation, bile secretion, motor and secretory activity of the small intestine, proliferation and desquamation of epithelial cells (enterocytes). Bile is able to stop the action of gastric juice, not only by reducing the acidity of gastric contents entering the duodenum, but also by inactivating pepsin. Bile has bacteriostatic properties. Its role in the absorption of fat-soluble vitamins, cholesterol, amino acids and calcium salts from the intestine is important.
Regulation of bile formation Bile formation occurs continuously, but its intensity changes due to regulatory influences. The act of eating and food intake increase bile formation. Bile formation changes reflexively with irritation of the interoceptors of the digestive tract, other internal organs and conditioned reflex effects. Parasympathetic cholinergic nerve fibers (impacts) increase, and sympathetic adrenergic ones reduce bile formation. There is experimental evidence of increased bile formation under the influence of sympathetic stimulation.
The humoral stimulators of bile formation (choleretics) include bile itself. The more bile acids that enter the bloodstream of the portal vein (portal bloodstream) from the small intestine, the more of them are released in the bile, but the less bile acids are synthesized by hepatocytes. If the entry of bile acids into the portal bloodstream decreases, then their deficiency is compensated by increased synthesis of bile acids in the liver. Secretin enhances the secretion of bile, the release of water and electrolytes (bicarbonates) in its composition. Bile formation is weaker stimulated by glucagon, gastrin, CCK, and prostaglandins. The effects of different stimulants of bile formation are different. For example, under the influence of secretin, the volume of bile increases mainly; under the influence of the vagus nerves and bile acids, its volume and the release of organic components increase; the high content of complete proteins in food increases the release and concentration of these substances in the bile. Bile formation is enhanced by many foods of animal and plant origin. Somatostatin reduces bile formation.
Bile secretion
The movement of bile in the biliary apparatus is caused by the difference in pressure in its parts and in the duodenum, and the state of the sphincters of the extrahepatic bile ducts. The following sphincters are distinguished in them: at the confluence of the cystic and common hepatic duct (Mirissi sphincter), in the neck of the gallbladder (Lutkens sphincter) and the terminal section of the common bile duct and the ampulla sphincter, or Oddi. The muscle tone of these sphincters determines the direction of bile movement.
Pressure in the biliary apparatus is created by the secretory pressure of bile formation and contractions of the smooth muscles of the ducts and gallbladder. These contractions are coordinated with the tone of the sphincters and are regulated by nervous and humoral mechanisms.
The pressure in the common bile duct ranges from 4 to 300 mmH2O. Art., and in the gallbladder outside of digestion it is 60-185 mm of water. Art., during digestion, due to the contraction of the bladder, it rises to 200-300 mm of water. Art., ensuring the release of bile into the duodenum through the opening sphincter of Oddi. The sight, smell of food, preparation for its intake and the actual eating of food cause a complex and different change in the activity of the biliary apparatus in different individuals, while the gallbladder first relaxes and then contracts. A small amount of bile exits through the sphincter of Oddi into the duodenum. This period of the primary reaction of the biliary apparatus lasts 7-10 minutes. It is replaced by the main evacuation period (or the period of emptying the gallbladder), during which contraction of the gallbladder alternates with relaxation and bile passes into the duodenum through the open sphincter of Oddi, first from the common bile duct, then the cystic duct, and subsequently the hepatic bile. The duration of the latent and evacuation periods and the amount of bile secreted depend on the type of food taken.
Strong stimulators of bile secretion are egg yolks, milk, meat and fats. Reflex stimulation of the biliary apparatus and cholekinesis is carried out conditionally and unconditionally reflexively with irritation of the receptors of the mouth, stomach and duodenum with the participation of the vagus nerves. The most powerful stimulator of bile secretion is CCK, which causes strong contraction of the gallbladder; gastrin, secretin, bombesin (through endogenous CCK) cause weak contractions, and glucagon, calcitonin, anticholecystokinin, VIP, PP inhibit contraction of the gallbladder.
Pathologies of bile secretion and bile formation
Gallstones
Bile that is unbalanced in composition (so-called lithogenic bile) can cause the prolapse of some gallstones in the liver, gallbladder, or bile ducts. The lithogenic properties of bile can arise as a result of an unbalanced diet with a predominance of animal fats to the detriment of plant fats; neuroendocrine disorders; disorders of fat metabolism with weight gain; infectious or toxic liver damage; physical inactivity.
Steatorrhea
In the absence of bile (or lack of bile acids), fats cease to be absorbed and are excreted in feces, which, instead of the usual brown color, becomes white or gray with a fatty consistency. This condition is called steatorrhea, its consequence is the lack of essential fatty acids, fats and vitamins in the body, as well as pathologies of the lower intestines, which are not adapted to chyme so saturated with undigested fats.
Reflux gastritis and GERD
In pathological duodenogastric and duodenogastroesophageal refluxes, bile in the refluxate enters in noticeable quantities into the stomach and esophagus. Long-term exposure to bile acids contained in bile on the gastric mucosa causes dystrophic and necrobiotic changes in the surface epithelium of the stomach and leads to a condition called reflux gastritis. Conjugated bile acids, and, first of all, conjugates with taurine, have a significant damaging effect on the esophageal mucosa at an acidic pH in the esophageal cavity. Unconjugated bile acids, present in the upper digestive tract, mainly in ionized forms, penetrate more easily through the mucous membrane of the esophagus and, as a result, are more toxic at neutral and slightly alkaline pH. Thus, bile entering the esophagus can cause different types of gastroesophageal reflux disease.
Bile research
To study bile, the method of fractional (multi-stage) duodenal intubation is used. There are five phases during the procedure:
- Basal secretion of bile, during which the contents of the duodenum and common bile duct are released. Duration 10 - 15 minutes.
- Closed sphincter of Oddi. Duration 3 - 6 minutes.
- Bile discharge portion A. Duration 3 - 5 minutes. During this time, 3 to 5 ml of light brown bile is secreted. It begins with the opening of the sphincter of Oddi and ends with the opening of the sphincter of Lutkens. During phases I and III, bile is secreted at a rate of 1 - 2 ml/min.
- Discharge of gallbladder bile. Portion B. Begins with the opening of the Lutkens sphincter and emptying of the gallbladder, which is accompanied by the appearance of dark olive bile (portion B), and ends with the appearance of amber-yellow bile (portion C). Duration 20 - 30 minutes.
- Hepatic bile secretion. Portion C. The phase begins from the moment the secretion of dark olive bile ceases. Duration 10 - 20 minutes. Serving volume 10 - 30 ml.
Normal bile levels are as follows:
- Basal bile (phases I and III, portion A) should be transparent, have a light straw color, density 1007-1015, and be slightly alkaline.
- Cystic bile (phase IV, portion B) should be transparent, have a dark olive color, density 1016-1035, acidity - 6.5-7.5 pH.
- Liver bile (phase V, portion C) should be transparent, golden in color, density 1007-1011, acidity - 7.5-8.2 pH.
Bile acids
Bile acids are tetracyclic monocarboxylic hydroxy acids from the class of steroids. By chemical nature they are derivatives of cholanic acid. They are the main end product of cholesterol metabolism. Bile acids are formed in the liver and excreted in bile, both in free form and as paired compounds (paired or conjugated bile acids) with glycine and taurine. Glycine and taurine are linked to bile acids by peptide bonds. Human bile mainly contains cholic, deoxycholic and chenodeoxycholic. In addition, lithocholic, allocholic and ureodeoxycholic acids are present in small quantities. In hepatocytes, primary bile acids are synthesized directly from cholesterol: chenodeoxycholic and cholic acids. After the release of bile into the intestine, under the action of enzymes of the intestinal microflora, secondary bile acids are formed from primary bile acids: lithocholic and deoxycholic acids. They are absorbed from the intestine, enter the liver with the blood of the portal vein, and then into the bile. It should be noted that intestinal microorganisms form about 20 different secondary bile acids, but only deoxycholic acid and, to a lesser extent, lithocholic acid are absorbed in noticeable quantities; the rest are excreted from the body. Due to the presence of α-hydroxyl groups in the structure, bile acids and their salts are amphiphilic compounds and have detergent properties. The main functions of acids are to form micelles, emulsify fats and solubilize lipids in the intestine, which increases the effectiveness of pancreatic lipase and promotes lipid absorption. Bile acids are also involved in the regulation of cholesterol synthesis, minimizing the increase or deficiency of cholesterol in the body, and the regulation of the formation and secretion of bile. Their pronounced influence on the functional state of various parts of the nervous system was discovered. It has been determined that they act as surfactants in the internal environment of the body: they do not pass through membranes, but regulate membrane processes of cells and intracellular structures.
If bile formation or bile secretion is impaired (for example, due to blockage of the bile duct with a gallstone), the conditions for the digestion of fats and the absorption of hydrolysis products worsen, and a significant part of them is excreted from the body. Fat-soluble vitamins are also not absorbed, which leads to the development of hypovitaminosis. A blood test is indicated for patients with impaired liver excretory function. An increase in the amount of bile acids is possible even with mild deviations. The level increases with cholestasis (primarily with a long course), which develops against the background of primary biliary cirrhosis. Another reason for an increase in titer is insufficient bile secretion during treatment with pharmaceuticals; tests can also confirm or exclude:
- subhepatic jaundice,
- alcoholic liver damage,
- hepatitis-like syndrome in infants,
- viral or toxic hepatitis,
- cystic fibrosis,
- congenital obstruction of the bile ducts,
- acute cholecystitis.
Gastric and intestinal juices. Structure and functions of the liver and pancreas
The stomach is the expanded part of the digestive tube. Its capacity is 1.5-3 liters.
The stomach is divided into an inlet, or cardiac part, a fundus, a body, and an outlet, or pyloric part. The stomach has two surfaces: anterior and posterior, passing into each other at the edges. The concave edge of the stomach is called the lesser curvature, the convex edge is called the greater curvature.
The mucous membrane of the stomach contains tubular glands that produce gastric juice (2-3 liters per day).
They consist of main, accessory and parietal cells. The main cells secrete digestive enzymes hydrochloric acid components , and the accessory cells secrete mucus (mucin) . In addition to the glands, the gastric mucosa contains endocrine cells that produce the hormone gastrin.
Gastric juice contains hydrochloric acid HCL and is acidic. Hydrochloric acid:
- has a bactericidal effect;
- activates pepsin;
- causes denaturation and swelling of proteins, facilitating their breakdown by enzymes;
- regulates the closure of the cardiac and pyloric sphincters.
Pepsin:
- breaks down proteins into oligopeptides, which are further digested into amino acids in the intestine. Gastric mucus contains mucoids and protects the stomach wall from chemical and mechanical influences, and also adsorbs enzymes, thereby increasing the surface of their contact with food masses.
Works by I.P. Pavlova on the study of digestion
To study the regulation of gastric secretion I.P. Pavlov developed a method of placing a fistula on a dog’s stomach in combination with cutting the esophagus. In such a dog, while eating, food did not enter the stomach (imaginary feeding). The use of this method made it possible to establish that gastric secretion occurs reflexively.
The secretion of gastric juice is associated with the sight and smell of food, as well as irritation of the oral cavity receptors by food. Gastric juice, separated by the smell and type of food, was named I.P. Pavlov’s “appetizing” one , i.e. preparing the stomach in advance for food intake.
Digestive regulation
Nervous regulation
Excitation from receptors along sensory fibers reaches the centers of juice-secreting reflexes located in the diencephalon and hypothalamus, and from them through the fibers of the vagus nerve it enters the glands of the stomach, causing the separation of gastric juice.
Humoral regulation
Of great importance in digestion are also humoral influences that enhance or weaken the activity of the gastric glands. These influences are carried out by biologically active substances formed in the mucous membrane of the duodenum and stomach, as well as various nutrients absorbed into the blood from the intestines. For example, fat breakdown products inhibit gastric secretion.
The transition of food gruel (chyme) from the stomach to the duodenum occurs periodically, in separate portions, which is associated with alternating relaxation and contraction of the pyloric sphincter in response to changes in the environment in the duodenum.
Irritation of the receptors of the duodenal mucosa by hydrochloric acid leads to a reflex contraction of the pyloric sphincter muscles and its closure.
After the acid is neutralized by intestinal juice, the muscles reflexively relax and the sphincter opens.
Reflexive defensive reactions
In some cases - with irritation of the root of the tongue, pharynx, or gastric mucosa - vomiting may develop - the involuntary release of stomach contents through the mouth. This reflex protective reaction occurs as a result of stimulation of the vomiting center in the medulla oblongata. When vomiting, the contents of the upper intestines, as a result of antiperistaltic contractions of the small intestine, enter the stomach and, together with its contents, thanks to antiperistalsis and contractions of the abdominal muscles and diaphragm, are expelled through the esophagus into the oral cavity.
Vomiting can also be caused by poor quality food and toxic substances that act on the vomiting center through the humoral route.
From the stomach, food enters the duodenum, into the lumen of which the ducts of the liver and pancreas open.
The liver is the largest gland in the human body. Its mass is about 1500-1700 g. It consists of hepatic lobules separated by layers of connective tissue.
The hepatic lobule is the main structural and functional unit of the liver. The lobules are formed by liver cells, between them there are blood and bile capillaries. In the center of the lobule lies a vein, and vessels and nerves pass through the interlobular connective tissue. There are approximately 500 thousand lobules in the liver.
The hepatic artery and portal vein enter the porta hepatis, and the hepatic vein and common hepatic duct exit. The common hepatic duct, merging with the duct of the gallbladder, forms the common bile duct, which, connecting with the pancreatic duct, opens into the lumen of the duodenum.
The branches of the portal vein in the lobule pass into the capillaries of the portal system - sinusoids. Sinusoids have a wide lumen, which causes blood to flow slowly through them. In the center of the lobule they flow into the central vein, which collects blood from the lobule. All central veins, connecting with each other, form 3-5 hepatic veins, which flow into the inferior vena cava. Thus, the peculiarity of the blood supply to the liver is the presence in it of a capillary network formed by the portal vein.
Bile is produced by liver cells constantly, regardless of the presence of food in the digestive canal. Approximately 0.5-1.0 liters of bile are produced per day. Outside the digestion process, it enters the gallbladder, where it accumulates. The secretion of bile increases during meals.
Bile is alkaline and contains:
- bile acids (taurocholic and glycocholic);
- cholesterol;
- bile pigments (bilirubin and biliverdin).
The liver plays an important role in the digestion process:
- supports the alkaline reaction of the small intestine;
- activates the action of digestive enzymes;
- emulsifies fats;
- promotes the absorption of fatty acids and fat-soluble vitamins (A, D, E, K);
- enhances the secretion of pancreatic juices;
- stimulates intestinal motility;
- many blood proteins, lipids and carbohydrates are synthesized in the liver;
- serves as a depot for glucose, which is stored in the form of glycogen;
- performs a barrier function - neutralizes toxic substances formed in the intestines.
About 1.5 liters of blood flows through the liver of an adult in 1 minute.
The pancreas is located behind the stomach, adjacent to the posterior abdominal wall. It consists of a head, body and tail.
The gland consists of:
- the exocrine (exocrine) part, which produces pancreatic juice, which enters the duodenum through the excretory duct;
- intrasecretory (endocrine) part that secretes the hormones insulin and glucagon into the blood.
Pancreatic juice - pancreatic juice:
- has an alkaline reaction;
- contains digestive enzymes that play a key role in the digestion of proteins, fats and carbohydrates;
- trypsin, chymotrypsin, collagenase and others act on proteins and oligopeptides, sequentially breaking them down into amino acids.
Enzymes are produced in an inactive form in the form of proenzymes, which are activated under the influence of other enzymes in the lumen of the duodenum:
- trypsin is formed from the proenzyme trypsinogen with the participation of enterokinase contained in intestinal juice;
- chymotrypsin - from chymotrypsinogen, under the influence of trypsin - amylase, maltase and lactase - break down carbohydrates into monosaccharides;
- lipase breaks down fats emulsified by bile into glycerol and fatty acids;
- Nucleases break down nucleic acids into nucleotides.
1.5-2.0 liters of pancreatic juice are secreted per day.
The secretion of pancreatic juice is regulated reflexively, as well as through the hormones secretin and cholecystokinin, secreted by the endocrine cells of the duodenum after food gruel enters it.
Without bile, lipids will not be digested
Bile is a complex liquid with an alkaline reaction. It contains a dry residue - about 3% and water - 97%. Two groups of substances are found in the dry residue:
- sodium, potassium, bicarbonate ions (HCO3¯), creatinine, cholesterol (CS), phosphatidylcholine (PC) that got here by filtration from the blood
- bilirubin and bile acids actively secreted
Normally, the ratio between the main components of bile Bile acids: Phosphatidylcholine: Cholesterol is 65: 12: 5 .
About 10 ml of bile per kg of body weight is produced per day, so in an adult this is 500-700 ml. Bile formation occurs continuously, although the intensity fluctuates sharply throughout the day.
The role of bile
1. Along with pancreatic juice, neutralization of acidic chyme coming from the stomach. In this case, HCO3¯ ions interact with HCl, carbon dioxide is released and the chyme is loosened, which facilitates digestion.
2. Provides fat digestion:
- emulsification for subsequent action by lipase, a combination of [bile acids + fatty acids + monoacylglycerols] is required,
- reduces surface tension , which prevents fat droplets from merging,
- formation of micelles capable of absorption.
3. Thanks to paragraphs 1 and 2, it ensures the absorption of fat-soluble vitamins (vitamin A, vitamin D, vitamin K, vitamin E).
4. Strengthens motility .
5. Excretion of excess cholesterol, bile pigments, creatinine, metals Zn, Cu, Hg, drugs. For cholesterol, bile is the only route of excretion; 1-2 g/day can be excreted with it.
The formation of bile ( choleresis ) occurs continuously, not stopping even during fasting. Increased choleresis occurs under the influence of n.vagus and when eating meat and fatty foods. Decrease - under the influence of the sympathetic nervous system and increased hydrostatic pressure in the bile ducts.
Bile secretion ( cholekinesis ) is ensured by low pressure in the duodenum, enhanced by the n.vagus and weakened by the sympathetic nervous system. Contraction of the gallbladder is stimulated by bombesin , secretin , insulin and cholecystokinin - pancreozymin . Relaxation is caused by glucagon and calcitonin .
Bile acid synthesis
The formation of bile acids occurs in the endoplasmic reticulum with the participation of cytochrome P450, oxygen, NADPH and ascorbic acid. 75% of cholesterol produced in the liver is involved in the synthesis of bile acids.
Reactions of bile acid synthesis using the example of cholic acid
Primary are synthesized in the liver :
- cholic acid (3α, 7β, 12α, hydroxylated at C3, C7, C12),
- chenodeoxycholic (3α, 7α, hydroxylated at C3, C7).
Then they form paired bile acids - conjugates with glycine (glyco derivatives) and with taurine (tauro derivatives), in a ratio of 3:1, respectively.
Structure of bile acids
In the intestine, under the influence of microflora, these bile acids lose the OH group at C7 and are converted into secondary bile acids:
- cholic to deoxycholic (3α, 12α, hydroxylated at C3 and C12),
- chenodeoxycholic to lithocholic (3α, hydroxylated only at C3) and 7-ketolithocholic (7α-OH group is converted to a keto group) acids.
Tertiary bile acids are also secreted These include
- formed from lithocholic acid (3α) – sulfolithocholic acid (sulfonation at C3),
- formed from 7-ketolithocholic acid (3α, 7-keto) by reducing the 7-keto group to an OH group - ursodeoxycholic acid (3α, 7β).
Ursodeoxycholic acid is an active component of the drug Ursosan and is used in the treatment of liver diseases as a hepatoprotective agent. It also has choleretic, cholelitholytic, hypolipidemic, hypocholesterolemic and immunomodulatory effects.
Regulation of synthesis
The regulatory enzyme is 7α-hydroxylase . There are two ways to regulate
- Covalent modification by phosphorylation-dephosphorylation. Glucagon , through the adenylate cyclase mechanism, leads to phosphorylation and activation of the enzyme. insulin has the opposite effect.
- Genetic regulation, i.e. change in the amount of enzyme:
- it can be hormonal: thyroid hormones induce transcription and increase the synthesis of the enzyme, estrogens repress and suppress the synthesis of this enzyme.
- with the participation of metabolites: cholesterol increases, and bile acids reduce enzyme synthesis.
Enterohepatic circulation
The circulation of bile acids consists of their continuous movement from hepatocytes into the intestinal lumen and the reabsorption of most of the bile acids in the ileum, which conserves cholesterol resources. 6-10 such cycles occur per day. Thus, a small amount of bile acids (only 3-5 g) ensures the digestion of lipids received during the day. Losses of about 0.5 g/day correspond to the daily de novo synthesis of cholesterol.
Enterohepatic recirculation of bile acids
0
Physiology of child digestion
Monday, 28 June 2021
Formation of skills in organizing healthy nutrition among parents (legal representatives of children), as well as persons engaged in the field of care and supervision of children
Physiology of child digestion
For children of early and preschool age, healthy nutrition is of great importance in the formation of health, functionality, and development of cognitive functions.
Preschool age is characterized by intensive processes of growth and development, a period of improving the functions of many organs and systems, incl. nervous system, intensive metabolic processes, development of motor skills and functions.
In the preschool age period, children confidently learn with pleasure, run, and love active and role-playing games. Children are impressionable, emotional and inquisitive, which allows them to successfully develop and consolidate the necessary skills of a healthy lifestyle and nutrition in a playful way.
In order to replenish large energy expenditures, children urgently need a constant supply of energy and all nutrients (proteins, fats, carbohydrates, vitamins, mineral salts and microelements), the only source of which is a complete, age-appropriate diet for children.
You should pay attention to the features of the child’s digestive system at this age. Despite the fairly well-developed masticatory apparatus (20 milk teeth, including four pairs of chewing teeth), the digestive functions of the stomach, intestines, liver and pancreas have not yet reached full maturity; they are labile and sensitive to inconsistencies in the quantity, quality and composition of nutrition, disorders eating regimen. Therefore, it is often at this age that various chronic diseases of the digestive system in children begin, their general physical development is disrupted, and their ability to master educational programs decreases.
Consequently, a properly organized daily routine, a healthy diet and adherence to personal hygiene rules will significantly reduce the risks of their occurrence.
For normal functioning, the body needs plastic and energy material, vitamins and microelements. There are six essential components of food that a child needs to maintain metabolism, the functioning of organs and tissues, for the growth and renewal of body cells - these are water, proteins, fats, carbohydrates, minerals and vitamins. Before the body assimilates them, they undergo splitting into simpler elements. This occurs due to the processes of digestion.
Digestion is the sum of the implementation of physical, chemical and physiological processes.
As a result, under the influence of enzymes, nutrients are broken down into simpler chemical compounds that have the ability to be absorbed through the wall of the gastrointestinal tract and enter the bloodstream, where they are then absorbed by the body’s cells.
Digestion processes are carried out in a certain sequence in all parts of the digestive tract (oral cavity, pharynx, esophagus, stomach, small and large intestines with the participation of the liver and gallbladder, pancreas).
Mineral salts, water and vitamins are absorbed by humans in the form in which they are found in food.
Proteins, fats and carbohydrates enter the body in the form of complex complexes. In order for them to be absorbed, complex physical and chemical processing is required. In addition, food components must first lose their species specificity, otherwise they will be accepted by the immune system as foreign substances.
Digestion begins with the grinding of food in the oral cavity, moistening it with saliva, primary metabolism and transformation under the influence of salivary enzymes (amylase, proteinase, lipase, phosphatase, RNase).
The average duration of food stay in the mouth should be about 15-20 seconds. If the time spent by food in the mouth is reduced, the digestive processes corresponding to this part of the digestive tract are disrupted (grinding, breakdown of starch into simple sugars).
Therefore, it is important to pay attention to the child so that he does not rush and chews his food thoroughly.
This is followed by the stage of movement of the food bolus due to peristaltic movements of the muscles of the pharynx and esophagus into the stomach.
The act of swallowing includes the oral (voluntary), pharyngeal (fast involuntary), and esophageal (slow involuntary) phases. The average duration of time for a bolus of food to pass through the esophagus is 2-9 seconds, and depends on the density of the food. To prevent the backflow of food, as well as to limit the impact of digestive enzymes on it, the digestive tract is equipped with special valves.
The bolus of food, once in the stomach, is subjected to mechanical and chemical treatment for three to five hours (under the influence of gastric juice and hydrochloric acid present in it, which provides an acidic environment in the stomach, causes denaturation and swelling of proteins, activates pepsinogens, and has a bactericidal effect; pepsin - digests protein-containing foods).
The lipolytic activity of gastric juice promotes the breakdown of emulsified milk fats.
Mucus formed in significant quantities in the stomach, on the one hand, performs a protective function, protecting the gastric mucosa from the action of hydrochloric acid, and also serves as a source of endogenous proteins for their subsequent utilization by colon microorganisms. There is also a special factor in the stomach that ensures the further absorption of vitamin B12.
After the stomach, the food bolus enters the small intestine. Intestinal juice in this section of the digestive tract has an alkaline environment. In the small intestine, the bulk of the resulting simple chemical fragments of food are absorbed.
Undigested food remains then enter the large intestine, where they can remain for 10 to 15 hours. In this section of the digestive tract, the processes of absorption of water and mineral salts take place, and the main processes of microbial metabolization of nutrient residues take place.
The liver plays an important role in the digestion process, where bile is formed. Bile promotes the emulsification of fats, the absorption of triglycerides, activates lipase, stimulates peristalsis, inactivates pepsin in the duodenum, has a bactericidal and bacteriostatic effect, enhances the hydrolysis and absorption of proteins and carbohydrates, stimulates the proliferation (proliferation of body tissue by cell multiplication by division) of enterocytes, the processes of formation and bile secretion.
The digestive tract in the human body performs several functions:
1) secretory (characterized by the formation of digestive juices - saliva, gastric, pancreatic, intestinal juices and bile);
2) motor (characterized by the movement of food through the digestive tract);
3) absorption (characterized by the flow of breakdown products of proteins, fats and carbohydrates, water, salts, and medications from the cavity of the gastrointestinal tract into the bloodstream);
4) intrasecretory (characterized by the production of hormones);
5) excretory (characterized by the production of metabolic products, which are then removed from the body).
Also, the digestive tract is the habitat of symbiotic associations of microorganisms. Representatives of normal microflora are present in the human body in the form of microcolonies fixed to certain receptors and enclosed in a biofilm. Biofilm, like a glove, covers the skin and mucous membranes of the cavities of a healthy person exposed to the environment.
From a functional point of view, the biofilm regulates the relationship between the macroorganism and the environment. As a result of microbial transformation, the food substrate entering the body is transformed into an intermediate or final product with one or another biological activity.
Normal microflora and products of its metabolism:
1) participate in the regulation of the gas composition of the intestines and other body cavities; metabolism of proteins, carbohydrates, lipids and nucleic acids; water-salt metabolism (Na, K, Ca, Mg, Zn, Fe, Cu, Mn, P, CI, etc.); ensuring colonization resistance, preventing the engraftment and reproduction of foreign organisms in the intestines or the colonization of certain areas of the digestive tract by species of microorganisms unusual for them); recycling of steroid compounds and other macromolecules (including drugs); detoxification of exogenous and endogenous substrates;
2) have a morphokinetic effect (stimulate the growth of epithelial cells, the rate of their renewal on the mucous membranes, peristalsis, affect the amount of food consumed, etc.);
3) perform an immunogenic function (strengthen humoral and tissue immunity, stimulate phagocytosis, production of immunoglobulins, interleukins, cytokines);
4) serve as a source of energy (formation of fatty acids);
5) produce a variety of biologically active compounds (vitamins, lipopolysaccharides, peptidoglycans, amines, antibiotics and other compounds with antimicrobial activity, neuropeptides, NO, indoles).
The composition of microflora in a biofilm can change under the influence of both various stress agents and the physiological state of a person.
Medical and drug interventions, including instrumental, surgical or drug treatments, can alter the integrity of the existing biofilm, leading to loss of some of its functions.
As a result of a violation of normobiocenosis, a condition arises, the most popular name of which is dysbacteriosis.
Intestinal dysbiosis is one of the factors contributing to the protracted, recurrent course of a number of diseases (dyspepsia, allergies, frequent colds, hypovitaminosis B).
The main forms of manifestations of dysbiosis:
1) impaired immune status;
2) impaired digestion and absorption of food, characterized by lack of appetite and decreased synthesis of B vitamins;
3) decreased tolerance of the intestinal mucosa to the action of pathogenic microflora;
4) reduction in the detoxification ability of microflora.
In practice, all these forms tend to occur together.
The successes achieved in the field of microbiological study of human intestinal microflora served as a prerequisite for the development and use as medicines, biologically active food additives, dietary and therapeutic and preventive fermented milk products based on Lactobacillus, Bifidobacterium and Streptococcus of animal and human origin.
The main purpose of the mass consumption of fermented milk products was the suppression of intestinal putrefactive bacteria, the elimination of dysbiotic disorders in the digestive tract due to the introduction of large quantities of living antagonistic lactic acid bacteria into the human body.
Dysbacteriosis, depending on the nature of changes in the composition of the microflora of the large intestine, is divided into 3 degrees.
Dysbacteriosis, as a rule, is combined with other pathological syndromes, therefore measures to correct the disturbed microbiocenosis are carried out simultaneously with the treatment of the underlying disease.
Positive effects for dysbiosis are achieved by using probiotic preparations or products with probiotic properties.
According to their action, probiotic preparations used for dysbiosis are divided into 7 classes:
1) classic probiotics (from the obligate flora of the human body: coli-, bifidum-, lactobacterin);
2) self-eliminating antagonists (from strains not typical for the body - bactisubtil, biosporin, sporobact);
3) combined probiotics (bifilong, bificol, acipol, linex, biobacton, kipacid);
4) live bacteria immobilized on a sorbent (bifidumbacterin-forte);
5) combined with lysozyme (bifiliz);
6) drugs - metabolic products of normal microflora (hilak-forte);
7) recombinant - subalin (Subtilis bacteria that control the synthesis of a2-interferon).
The most effective means of preventing and treating dysbacteriosis are bifidumbacterin preparations. A good effect of primary and secondary prevention is achieved by using domestic fermented milk products and bio-ice cream.
The effectiveness of using bio-ice cream in the prevention of dysbacteriosis in preschool children was studied on the basis of budgetary preschool institutions in Omsk. The study was carried out in three stages: the first stage - assessing the health of children before the experiment; the second stage - experimental, included the distribution of bio-ice cream (6 weeks) with subsequent monitoring of the children's health and mood - 3 months; the third stage - experimental, included repeated distribution of bio-ice cream (6 weeks) with subsequent observation of the children's health and mood - 3 months.
The study included 179 children who attended preschool organizations, of which 92 children made up the “main” group (children who received bio-ice cream with their diet), 87 – the “control” group (children who ate the regular menu). The groups did not differ in age (p>0.05).
The results of the study indicated the high effectiveness of bio-ice cream included in the menu in the prevention of dysbacteriosis and normalization of intestinal microflora in children.
The positive results of the experiment include a significant reduction in complaints of allergic reactions, dermatitis, and gastrointestinal tract disorders in children. Also, all parents, without exception, noted an improvement in the psycho-emotional state of their children on the days when the children were given ice cream.
Thus, the findings allow us to recommend, in order to prevent dysbiosis and its manifestations in children, the inclusion of bio-ice cream in the main diet of children.
Thus, understanding the physiology of a child’s digestion is the foundation for building a menu that fully provides the body with food and biologically active substances.
Information prepared on the basis of open Internet sources
Department for the organization of hygienic education and training