Symptoms Classification Diagnostics Treatment Information block
Chronic gastritis is an inflammation of the gastric mucosa that occurs under the influence of factors of various etiologies (bacterial, chemical, thermal and mechanical).
THE INSTITUTE OF ALLERGOLOGY AND CLINICAL IMMUNOLOGY has:
- range of services for accurate diagnosis of diseases
- special treatment programs
- consultations
- carried out by doctors with academic degrees.
When identifying concomitant diseases, consultations are held with specialists in related fields (otorhinolaryngologists, endocrinologists, neurologists, gastroenterologists, dermatovenerologists), consultations with Doctors of Medical Sciences.
Attention! The same symptoms can be signs of different diseases! Do not self-medicate, consult a gastroenterologist!
Symptoms
| With increased acidity | With low acidity |
| Heartburn Belching sour Dull aching pain in the epigastrium after eating. Feeling of heaviness, pressure in the epigastrium after eating. Constipation. Decreased appetite | Belching air Nausea, vomiting Burning pain in the epigastrium after eating Diarrhea Flatulence, rumbling in the stomach. |
Forms of acute gastritis
The catarrhal form of gastritis is considered the simplest. It is the most common. In order to diagnose the disease, it is enough to perform a gastroscopy. This disease occurs after mild food poisoning, any allergic reactions, overeating or stress. Often the symptoms of the described illness are as follows: vomiting, weakness, increased body temperature, bad breath, and a constant feeling of thirst.
Toxic-chemical (necrotic) illness occurs after chemicals enter the body. Scars appear in the intestines. They greatly influence the vital processes of all organs. The following symptoms are typical: pain, weakness, pale skin, nausea, vomiting and thirst.
The phlegmonous form is the most dangerous of the types described above. It begins to develop after the onset of catarrhal gastritis. With this disease, all layers of the stomach walls are destroyed. If a person has been diagnosed with the described illness, then surgical intervention cannot be avoided.
Classification
Sydney classification system for chronic gastritis
| Type of gastritis | Synonyms (former classifications) |
| Non-atrophic | Superficial Chronic antral Gastritis type B Hypersecretory gastritis |
| Atrophic autoimmune | Type A gastritis Diffuse gastritis of the gastric body associated with B12-deficiency anemia and decreased secretion |
| Atrophic multifocal | Mixed gastritis type A and B |
| Chemical | Reactive gastritis type C Reactive reflux gastritis |
| Radiation | |
| Lymphocytic | Gastritis associated with celiac disease |
| Granulomatous | Isolated granulomatosis |
| Eosinophilic | Allergic |
| Other infectious | Bacteria (except Helicobacter pylori) Fungi, Parasites |
| Giant hypertrophic | Ménétrier's disease |
According to the clinical picture
| chronic gastritis type A | gastritis type B | type C |
| primary autoimmune gastritis of the fundus of the stomach (fundic) | antral gastritis of bacterial origin | reflux gastritis |
| By origin | According to the state of secretory function | According to histological picture | According to the anatomical location of the inflammation zone |
| bacterial, autoimmune, endogenous, iatrogenic, reflux gastritis | decreased increased normal | superficial, atrophic, hyperplastic | antral fundamental |
Chronic abdominal pain is pain that is present for more than 3 months. It can bother you constantly or periodically (recurrent). Can come from any system, including the genitourinary, gastrointestinal and gynecological. (Continued. Start of material here.)
Classification of gastritis
Diagnostic assessment of dysplasia. Conventional white light endoscopy cannot accurately differentiate and diagnose preneoplastic conditions of the stomach - antral nodularity, absence of folds, visible vessels/thinning of the mucosa, white patches on the mucosa.
Antral nodularity may be an endoscopic sign (>90% of cases) for H. pylori infection. However, with the exception of children, it is present in a minimal number of patients with Helicobacter pylori gastritis among adults (Loffeld R., 1999; Bah A. et al., 1995; Calabrese C. et al., 1999).
Newer high-definition endoscopes are no more reliable. Magnifying chromoendoscopy and narrow spectrum endoscopy (NBI) with/without magnification and staining with methylene blue, indigo carmine, acetic acid, hematoxylin improve the diagnosis of preneoplastic conditions/gastric pathologies. However, magnifying chromoendoscopy cannot be recommended for routine use, and NBI is not used in daily clinical practice.
Atrophic gastritis and intestinal metaplasia often spread unevenly throughout the stomach. To diagnose dysplasia, at least 4 non-targeted biopsies must be taken from 2 topographic places (from the lesser and greater curvature of the body and the antrum of the stomach), additionally - specifically from the pathology zone. The OLGA and OLGIM histopathological staging systems may be useful in determining the risk of progression to gastric cancer. Histological findings allow the diagnosis of neoplastic epithelium without evidence of tissue invasion. Correct diagnosis and staging is critical. There is great variability in histological protocols.
Histological data according to WHO classification:
- negative data for intraepithelial neoplasia/dysplasia;
- unspecified intraepithelial neoplasia/dysplasia;
- low grade intraepithelial neoplasia/dysplasia;
- high grade intraepithelial neoplasia/dysplasia;
- intramucosal invasive neoplasia/intramucous carcinoma.
(Negative intraepithelial neoplasia/dysplasia - chronic atrophic gastritis, intestinal metaplasia. Indeterminate intraepithelial neoplasia/dysplasia - doubt about neoplastic or non-neoplastic pathology (reactive or regenerative); requires additional biopsy.)
Patients with widespread atrophic gastritis and/or intestinal metaplasia should undergo endoscopic examinations every 3 years. There is no evidence of patients with mild to moderate atrophy/intestinal metaplasia limited to the antrum.
Patients with low-grade dysplasia in the absence of endoscopic pathology require examination every year. If endoscopically defined pathology is present, endoscopic resection should be considered to obtain a more accurate histological diagnosis.
Patients with high-grade dysplasia in the absence of endoscopic pathology need to repeat the endoscopic examination with an extended biopsy (“gastric mapping”); observation at intervals of 0.5–1 year is indicated (Dinis-Ribeiro M. et al., 2012).
Helicobacter and non-Helicobacter gastritis. Because H. pylori is the most common cause of gastritis and is probably easily treated, non-Helicobacter gastritis ( see Figure 3 ) should be diagnosed with special care. H. pylori infection is usually missed due to the low number of pathogens. This situation may occur, for example, when patients have recently taken antibiotics or proton pump inhibitors, or the infection is caused by intestinal metaplasia in the stomach. Therefore, in addition to taking biopsies for urease testing and histology, the physician should perform serological testing for H. pylori, which can confirm the absence of the pathogen.
Figure 3. Non-Helicobacter gastritis.
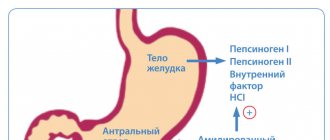
Autoimmune metaplastic atrophic gastritis is an inherited autoimmune disease that affects parietal cells, resulting in hypochlorhydria and decreased production of intrinsic factor. Consequences include atrophic gastritis, B12 malabsorption, and often pernicious anemia. The risk of gastric adenocarcinoma increases 3 times.
Patients with autoimmune metaplastic atrophic gastritis have antibodies to parietal cells and their components, which include intrinsic factor and proton pump H+/K+ ATPase. This gastritis is inherited in an autosomal dominant manner. Some patients may also develop Hashimoto's thyroiditis and 50% have thyroid peroxidase antibodies. On the other hand, antibodies to parietal cells are found in 30% of patients with thyroiditis.
Lack of intrinsic factor contributes to vitamin B12 deficiency, which can lead to megaloblastic anemia (pernicious anemia) or neurological symptoms (subacute combined degeneration). Hypochlorhydria is associated with G-cell hyperplasia and elevated serum gastrin levels (often >1000 mU/mL). Elevated gastrin levels lead to hyperplasia of enterochromaffin-like cells, which sometimes undergo transformation into carcinoid tumors. In some patients, autoimmune metaplastic atrophic gastritis may be associated with chronic H. pylori infection, although the relationship is unclear. Gastric resection and chronic acid suppression with PPIs cause similar deficiencies in intrinsic factor secretion.
Diagnosis is carried out using a paraendoscopic method for determining the pH of gastric juice, then a Congo red test and endoscopic biopsy. Serum vitamin B12 values should be obtained. Antibodies to parietal cells can be detected but are not routinely measured. The issue of endoscopic surveillance during cancer screening is unresolved, apparently, as with Helicobacter pylori atrophic gastritis. Treatment consists of replacement therapy and parenteral vitamin B12 replacement.
Reactive gastritis is caused by chemical irritants such as alcohol, NSAIDs and bile. The antrum is usually involved.
Lymphocytic gastritis is characterized by a dense infiltrate in the body of the stomach and antrum. It is associated with celiac disease as well as lymphatic colitis. Some patients benefit from PPIs. A gluten-free diet leads to improvement.
Hypertrophic gastritis (Menetrier's disease). Occasionally, the folds of the stomach are greatly increased in size due to hyperplasia and hypertrophy of the specialized acid-producing mucosa. Excessive mucus secretion leads to a syndrome of hypoalbuminemia with diarrhea, edema, or hypercoagulable status. One of the reasons is H. pylori. In children - cytomegalovirus (CMV). Other causes are idiopathic.
Portal hypertensive gastropathy and angiodysplasia. Angiodysplasia caused by portal hypertension gives a picture of a “snake skin” and a “watermelon” stomach. They can cause blood loss in the gastrointestinal tract. If necessary, treatment is carried out with argon plasma coagulation.
NSAID-induced erosive gastritis. Aspirin and NSAIDs are corrosive drugs that inhibit the synthesis of prostaglandin, which is necessary for the formation of mucus and the alkaline barrier in the stomach. The resulting erosions are often asymptomatic, but sometimes lead to gastric or duodenal ulcers. The harmful effects of NSAIDs and H. pylori are not synergistic because infection increases prostaglandin levels, partially counteracting the damaging effects of NSAIDs. Eradication of H. pylori before or at the start of NSAID therapy is warranted.
Viral gastritis is usually caused by CMV and occurs in patients with AIDS or those who have undergone organ transplantation. Ganciclovir is used to treat CMV, but after its discontinuation there are frequent relapses. A Herpes simplex infection may be detected by chance.
Bacterial gastritis is caused by other infections (Streptococcus, Staphylococcus, Klebsiella and E. coli). Being in the lumen of the stomach, such microorganisms cause problems only in the presence of severe ischemia or immune suppression. Phlegmonous gastritis occurs when such pathogens contribute to purulent necrosis of the stomach wall. Emphysematous gastritis develops when pathological organisms produce gas.
Fungal gastritis itself is rare, although colonization of gastric ulcers by Candida fungi is common. Severe necrotizing gastritis can be caused by opportunistic fungi in immunosuppressed patients.
Parasitic gastritis is rare and can be caused by, for example, Strongyloides stercoralis and Cryptosporidium.
Granulomatous gastritis is caused by infections or toxins (eg, tuberculosis, syphilis, histoplasmosis) and non-infectious causes (eg, sarcoidosis, Crohn's disease and Wegener's granulomatosis). Tuberculosis infection can occur in the presence of AIDS and disseminated tuberculosis. Syphilitic gastritis occurs in the second or third stages of syphilis.
Eosinophilic gastritis is characterized by intense eosinophilic infiltration of the antrum, and to a lesser extent the body or vault of the stomach. May occur due to hypersensitivity to medications or certain foods, or as a result of a parasitic infection. Patients experience abdominal pain, nausea, or vomiting. The stool is tested for the presence of an infectious pathogen. But in most cases, the causes cannot be found. Treatment with corticosteroids is effective.
Vascular ectasia of the gastric antrum, also known as watermelon stomach, is predominantly seen in women and is associated with achlorhydria and gastric atrophy. Patients with acute and chronic gastrointestinal bleeding leading to anemia are presented. Endoscopically visible red stripes converging towards the pylorus. Histology is pathognomonic and is characterized by vascular ectasia, spindle cell proliferation, and fibrohyalinosis. Most patients respond to treatment with Nd:YAG laser or argon plasma coagulation. Surgery in the form of anthrumectomy is the last hope.
Portal hypertensive gastropathy is noticeable in patients with liver disease. The mosaic pattern of the mucosa is mainly observed in the body and vault of the stomach. Treatment includes nonselective beta blockers (propranolol or nadolol), transjugular portosystemic shunt, or portal decompressive surgery. Local laser treatment or argon plasma coagulation may worsen the situation.
There is no correlation between microscopic inflammation (histological gastritis) and the presence of gastric symptoms (abdominal pain, nausea, vomiting). In fact, most patients with histological evidence of acute gastritis are asymptomatic.
Diagnosis usually occurs during endoscopy performed for symptoms of dyspepsia. A patient with acute gastritis may experience discomfort that is difficult to describe in words. The diagnosis can be suspected based on history and confirmed endoscopically and histologically in biopsies taken during the procedure. Macroscopic diagnosis of atrophic gastritis by routine endoscopy is impossible; it is performed only using dyeing techniques (see Fig. 4).
Figure 4. Endoscopy using dye techniques. A - normal fine-mesh microrelief of the antrum of the stomach. Study with methylene blue + espumizan.
B - atrophic antral gastritis. The phenomenon of “cracked earth”.
B - atrophic fundal gastritis. Study with Congo red (the pH indicator did not change the color in the body of the stomach).
G - nodular (hyperplastic) antral (Helicobacter) gastritis.
Causes
| Type of gastritis | Etiological factors |
| Non-atrophic | Helicobacter pylori Other factors |
| Atrophic autoimmune | Immune mechanisms |
| Atrophic multifocal | Helicobacter pylori Nutritional disorders Environmental factors |
| Special forms | |
| Chemical | Chemical irritants: bile (DGR), NSAIDs |
| Radiation | Radiation damage |
| Lymphocytic | Idiopathic Immune mechanisms Gluten |
| Granulomatous | Crohn's disease Sarcoidosis Granulomatosis Wegener's Foreign bodies Idiopathic |
| Eosinophilic | Food allergies Other allergens |
| Other infectious diseases | Bacteria (except Helicobacter pylori) Fungi, Parasites |
| Giant hypertrophic | Ménétrier's disease |
| Exogenous (external) | Endogenous (internal) |
| 1. Diet disorder: large gaps between meals, late and night dinners, fast food, swallowing poorly chewed food. 2. Intake of foods that irritate the gastric mucosa: spicy, smoked, sour, salty, rough food, strong coffee, alcohol, scalding hot or cold food, consumption of poor quality products. 3. Chemicals and drugs. 4. Smoking. 5. Psychologically severe, stressful conditions. 6. Harmful production (high smoke or dusty atmosphere in the workplace). | 1.Helicobacter pylori (HP) 2.Parasitic infections 3. Severe infectious diseases (tuberculosis, etc.). 4.Endocrine pathologies (diabetes mellitus, thyroid pathologies). 5.Immunity disorders. 6. Impaired breathing or pathologies of the circulatory system. 7. Duodenogastric reflux. |
Diagnostics
Urease breath test is the most innovative and accurate test for Helicobacter pylori! The best method for quality control of treatment!
THE INSTITUTE OF ALLERGOLOGY AND CLINICAL IMMUNOLOGY has a fundamental base that allows it to carry out a full range of diagnostic and therapeutic measures that meet the level of international standards. Many of the diagnostic and treatment methods were developed by the staff of our Institute.
The diagnosis is established on the basis of the patient’s clinical picture and history, physical examination, laboratory diagnostics, endoscopy (gastroscopy), biopsy and other studies.
If necessary, you can be advised by related specialists and experienced doctors who are developing new diagnostic and treatment methods in these areas of medicine.
Every patient with chronic gastritis must remember that gastritis is the cause of the development of other pathologies of the gastrointestinal tract!
Laboratory diagnostics are aimed at identifying the cause of chronic gastritis, determining the level of gastrin, pepsinogen (the ratio of pepsinogen I and pepsinogen II) in the blood, and the content of vitamin B12 in the serum. Bacteriological examination, biochemical examination and other studies may be carried out.
Useful video
Is poor nutrition always the cause of gastritis? We invite you to watch the video and find out what factors can provoke the development of the disease.
The classification of gastritis is complex and multifaceted. In most cases, there is no need for the patient to thoroughly understand all variants of the course of the disease. It is important to find out what reason provoked the development of gastritis in his case, and direct all efforts to combat this factor. Therefore, you need to promptly seek medical help and follow all doctor’s instructions.