Digestive enzymes act as catalysts that speed up the breakdown of nutrients and ensure healthy digestion. They break down food into simple compounds, facilitating their absorption in the intestinal walls. By their structure, enzymes are special proteins produced by living cells of the pancreas, stomach, and small intestine.
In some situations, there may be a lack of your own enzymes. This may manifest itself as heaviness after eating, abdominal discomfort, and bloating. Often such symptoms arise in everyday situations, for example, during feasts when a large amount of food has been eaten. If loss of appetite, prolonged diarrhea or weight loss are added to these symptoms, then the cause may be hidden in the functioning of the pancreas. If the organ's functioning is impaired, it may produce fewer enzymes than necessary, which can affect the quality of the digestive process.
What are Digestive Enzymes
Enzymes are protein molecules that help process protein, fat and carbohydrate particles. The key role of enzymes in digestion is to break down food into nutritional components for easier absorption. Without this process, the absorption of nutrients through the intestinal walls will be significantly lower, which will lead to a number of disorders. That is, in short, the role of enzymes in digestion is reduced to preparing and processing food to a state in which the body can extract maximum benefit from it, digest and assimilate without deteriorating the functioning of the gastrointestinal tract.
The production of enzymes is a rather complex process that consists of many reactions.
The synthesis of enzymes that help digestion is influenced by many factors, although the most significant role is played by:
- Diet and variety of foods;
- Condition of the gastrointestinal tract, presence/absence of chronic diseases;
- Lifestyle;
- Genetic characteristics;
- Hypovitaminosis.
The largest number of enzymes is located in three areas:
- Oral cavity;
- Stomach;
- Intestines.
All enzymes are divided into several types, depending on the tasks they perform. If we evaluate what function enzymes perform in the digestion process, then 4 main groups should be distinguished:
- Lipases - needed to break down fats;
- Nucleases - decompose nucleic acids into simple structures;
- Proteases and peptidases - break down protein structures into amino acids and peptides;
- Carbohydrases hydrolyze carbohydrates.
What task do enzymes perform?
Enzymes affect food already in the oral cavity. Therefore, the entire process is usually divided into several stages, depending on the passage of a particular area.
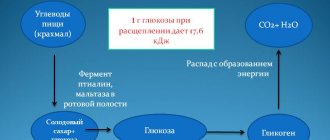
That is, the role of enzymes in digestion begins in saliva, when food is crushed by chewing. This is the primary stage. During the chewing process, it mixes with saliva, which also contains enzymes. Their main task is to process carbohydrates into simple sugars.
After initial processing, the food enters the stomach, where gastric juice begins to act on it. This is the second stage. The role of digestive enzymes in the stomach is to break down food into simpler components. During this process, hydrochloric acid triggers the production of lipase and pepsin. These are the main enzymes that are active in the stomach. Lipase is responsible for the breakdown of fats into fatty acids, and pepsin is responsible for protein structures (destroys them into peptone and albumin).
After passing through the stomach, food descends into the duodenum, where “local” enzymes, enterokinases, begin to influence it. They are necessary to launch the pancreatic secretion, which secretes a huge amount of enzymes. All of them are divided into 5 groups:
- Proteases are divided into trypsin, chymotrypsin elastase and carboxypeptidase. Responsible for the breakdown of plant and animal foods, as well as for the process of elastin hydrolysis;
- Nucleases - necessary to break the connection between RNA and DNA chains;
- Amylase - necessary for the creation of simple carbohydrates;
- Steapsin and lipase - destroy fatty structures.
After entering the small intestine, the 3rd and most extensive stage begins. Here the food begins to be affected by even more enzymes that improve digestion. Among them:
- Lipases;
- Peptidases;
- Erepsin;
- Sacrase;
- Isomaltase;
- Maltase;
- Lactase.
Once in the large intestine, food is also subjected to a large number of enzymes. They are produced by microorganisms to break down certain nutrients. The most active among them are:
- Enterobacteriaceae or Escherichia coli;
- Lactobacilli;
- Bifidobacteria.
Only after passing through all these stages do nutrients enter the blood.
The role of enzymes of non-animal origin in digestive disorders of various etiologies
It’s still strange how much our mind and feelings are subordinate to the digestive organs. Jerome Klapka Jerome
Digestion means the processing of complex substances (proteins, fats, carbohydrates) with the help of enzymes into simple ones for their subsequent absorption. The processing process is carried out as food masses move through the gastrointestinal tract (GIT). In the oral cavity, food is mixed with saliva, which has amylase activity, and is subjected to mechanical processing. The significance of the stomach is the deposition and liquefaction of food under the influence of hydrochloric acid and pepsin, denaturation and initial hydrolysis of proteins, and the creation of a food bolus for evacuation into the duodenum.
The main hydrolytic processes occur in the small intestine, where nutrients are broken down into monomers, absorbed and released into the blood and lymph. The process of processing nutrients in the small intestine has three successive interconnected stages, united by AM Ugolev (1967) into the concept of “digestive transport conveyor” [1]: cavity digestion, membrane digestion, absorption.
Cavity digestion includes the formation of chyme and hydrolysis of food components to an oligo- and monomeric state. A key role in cavity digestion is played by pancreatic enzymes. The short chains of proteins, carbohydrates and fats formed during cavity hydrolysis are finally broken down using membrane digestion mechanisms. Pancreatic enzymes adsorbed on nutrients continue to play an active role at this stage, which unfolds in the parietal layer of mucus. The final hydrolysis of nutrients occurs on the outer membrane of enterocytes with the help of intestinal hydrolases.
After this, the final stage begins—absorption, i.e., the transfer of broken down components of nutrients from the intestinal lumen into the internal environment of the body.
The most common complaints of patients with indigestion are dyspeptic manifestations. Translated from ancient Greek, “dyspepsia” means “indigestion” (from “δυσ” - denial, “π?ψις” - digestion). All types of dyspepsia are clinically divided into gastric, intestinal and biliary. Symptoms of gastric dyspepsia include heaviness, epigastric discomfort, early satiety, belching, heartburn, nausea, vomiting, and loss of appetite. Manifestations of intestinal dyspepsia include flatulence, rumbling, diarrhea, constipation, and unstable stools. Biliary dyspepsia syndrome is characterized by decreased appetite, a feeling of bitterness in the mouth, stool disorders (constipation, diarrhea or their alternation), flatulence, a feeling of discomfort, heaviness, and fullness in the right hypochondrium [2].
Digestive disorders are a manifestation of an underlying disease, for example, organic and functional diseases of the biliary system, gastritis, duodenitis, peptic ulcers, pancreatitis, hepatitis and cirrhosis of the liver, disorders of the intestinal flora, abdominal ischemic syndrome. Digestive disorders can be caused by various factors. Both functional and organic lesions of the gastrointestinal tract are accompanied by a disorder of their motor, absorption, secretory or excretory functions, disrupting the interconnected and complex process of food digestion. The main syndromes of digestive disorders include maldigestion, malabsorption and malnutrition. If we are talking about a disorder of cavity digestion, i.e., a violation of hydrolysis in the lumen of the digestive tract, then this condition is called maldigestion, and if we are talking about a violation of membrane digestion and absorption, then malabsorption and malnutrition. Traditionally, there are several groups of main causes for the formation of these syndromes [3]:
- Insufficiency of cavity digestion due to:
- pancreatic exocrine insufficiency in chronic pancreatitis (CP), subtotal pancreatectomy, pancreatic cancer and fistulas, cystic fibrosis;
- inactivation of digestive enzymes and reduction of enterokinase activity in the intestine with gastroduodenitis, duodenal ulcer (duodenal ulcer), small intestinal dysbiosis, Zollinger-Ellison syndrome;
- disturbances in the transit of intestinal contents and the mixing of enzymes with food chyme in irritable bowel syndrome, conditions after vagotomy and drainage operations, duodeno- and gastrostasis, intestinal pseudo-obstruction;
- decreased enzyme activity (as a result of “dilution”) in postgastrectomy syndrome, small intestinal dysbiosis and the condition after cholecystectomy;
- disturbances in the production of cholecystokinin, pancreozymin, secretin;
- deficiency of bile acids in the small intestine with biliary obstruction, hepatitis, primary biliary cirrhosis, pathology of the terminal portion of the small intestine and its dysbiosis, treatment with cholestyramine;
- gastrogenic insufficiency after gastrectomy and gastrectomy, with atrophic gastritis.
- Parietal digestive disorders:
- with a deficiency of disaccharidases (congenital, acquired lactase or other disaccharidase deficiency - invertase, trehalase, isomaltase);
- as a result of degeneration and death of enterocytes (Crohn's disease, celiac enteropathy, sarcoidosis, radiation, ischemic and other enteritis).
- Disturbances in the outflow of lymph from the intestines (obstruction of the lymphatic ducts) with lymphangiectasia, lymphoma, intestinal tuberculosis, carcinoid.
- Combined disorders in diabetes mellitus, giardiasis, hyperthyroidism, hypogammaglobulinemia, amyloidosis, AIDS.
Given the variety of causes of digestive disorders described by the author, disorders are most often caused by diseases of the pancreas with progressive insufficiency of its exocrine function (primary pancreatic insufficiency). In clinical practice, secondary or relative exocrine pancreatic insufficiency is also common.
Despite the above organic causes of digestive disorders and dyspepsia, functional diseases of the gastrointestinal tract are much more common, as well as banal dietary errors and “banquet” overeating. With the latter, as a rule, the ratio of the main components of normal nutrition is disrupted - fats (animal and vegetable) and carbohydrates, including indigestible fiber, predominate. Alcohol also often “interferes” with the digestion process, which in small doses (up to 50 ml 40%) stimulates the digestive process, and in higher doses sharply disrupts it, aggravating dyspepsia [4].
For all of the above digestive disorders, in addition to treatment aimed at normalizing motility, reducing pain, eliminating microbial contamination, restoring the intestinal microbial landscape, restoring vitamin and mineral status, enzyme therapy is necessary. Enzyme preparations (EP) were first used in medical practice more than 100 years ago. Digestive enzymes are currently widely used for various gastroenterological pathologies. Currently, a large number of enzyme preparations are used in clinical practice, characterized by different combinations of components, enzyme activity, production method and release form. When choosing an enzyme preparation in each specific case, the doctor must first of all pay attention to its composition and the activity of its components [5].
The therapeutic capabilities of enzymes show significant differences depending on their animal or plant origin. Today, “animal” enzymes are mainly produced from the pancreas of pigs. They contain the highest concentration of enzymes among all enzyme preparations known to date. These enzymes have been used since the early 1900s and have been very effective under certain conditions. Some enzymes are derived from plants, including bromelain from pineapple, papain from papaya, and nanokinase from fermented soybeans. Other plant enzymes are grown from various types of fungi and molds, sometimes in very high concentrations. Contrary to popular belief, such enzymes do not contain any remnants of the substances from which they were grown.
The enzyme industry that exists today began at the end of the 19th century. In 1894, Dr. Jokichi Takaminu was awarded U.S. Patent 525,823, “Method for the Preparation of Diastatic Enzyme,” which details the process and extraction of amylases from the fungus Aspergillus oryzae (A. oryzae). His patented digestive product Taka-diastase was marketed by Parke, Davis & Company worldwide. By 1932, Dr. E. Howell had established a company in Illinois to produce supplemental enzymes to replace those that were destroyed in the cooking and canning of the food industry. Dr. E. Howell's 1947 review of "The State of Food Enzymes in Digestion and Metabolism" cites the use of papain as a digestive aid and benefit for "digestive disorders of many different kinds." Fungal amylase is similarly cited in this treatise as a source of lipase and other pancreatic extracts used in the treatment of diseases of the digestive tract [6].
A. oryzae is a mushroom widely used in traditional Japanese fermentation industries, including soy sauce, sake, curd seasoning, and vinegar production. Filamentous fungi have the ability to produce various enzymes in very large quantities. It is known that A. oryzae among filamentous fungi has the most significant potential for producing various secretory enzymes. In addition, developments in the field of genetic engineering have led to the use of A. oryzae in the production of industrial enzymes in modern biotechnology [7].
Enzymes from the fungus A. oryzae have been studied in numerous studies evaluating their role in maintaining healthy digestion. Additionally, human studies have suggested that proteolytic enzymes derived from the fungus A. oryzae may play a role in anti-inflammatory and fibrinolytic therapy. Enzymes are relatively stable when heated and are active over a wide pH range (Fig.). This is important because most enzymes are deactivated in stomach acid. The described enzymes are synthesized from a fungus, but do not contain a fungal residue, being non-pathogenic. Modern filtration technologies allow these fungal enzymes to be effective and safe for humans.
Any oral enzymes must withstand stomach acidity to be therapeutically effective. Most animal-derived enzymes must be enteric-coated to protect them from stomach acidity. The enteric coating does provide some protection against acid, but the coating is often damaged in the stomach or does not dissolve completely in the small intestine. This affects the effectiveness of the enzyme preparation. On the other hand, fungal proteases are remarkably acid-resistant and do not require enteric coating [8].
Fermented microorganisms with many years of use in food products, microbial enzymes were specifically selected based on the unique characteristics of each enzyme. Another limiting factor in the use of animal enzymes such as pancreatin is the lack of variety. On the other hand, fungal enzyme mixtures can be custom-made to meet different enzymatic digestive needs. This is possible because mushroom sources not only contain proteases, amylases and lipases, but may also contain many other enzymes such as thylactase, cellulase, lactase, etc. [9].
Overall, fungal enzymes are superior to pancreatin in terms of pH range, acid stability, activity, diversity, and safety. In addition to the above benefits, fungal enzymes are suitable for a vegetarian diet.
According to Dr. Mark Percival (1985), adding digestive enzymes orally just before or during meals can aid digestion. Although most supplemental enzymes are labile and are inactivated by exposure to stomach acid, Mark Percival believes that some of the enzymes will remain active if taken with food or immediately before a meal. Mark Percival says that "the enzymes are physically protected" when eaten and allow enzymatic activity to occur in the stomach. pH plays an important role in enzymatic activity, so Aspergillus-derived enzymes “can be quite useful as they appear to be extremely stable even when exposed to an acidic environment.” Dr. Edward Howell adds that since enzyme activity begins before food is swallowed, the contents of this enzyme can be taken without a capsule with food to immediately begin the digestion process [10].
Ambient temperature plays a decisive role in enzyme activity. Fungal enzymes work best in the temperature range of 95–105°F (35.0–40.56°C). At a normal body temperature of 98.6°F, fungal enzymes are ideal.
To ensure lipolysis by animal lipase, the presence of bile acids is necessary to activate the enzyme and emulsify fats. Therefore, traditional PT may not be effective enough in case of deficiency of bile acids in the duodenum (hepatogenic pancreatic insufficiency in cholestatic liver diseases, hypomotility of the gallbladder, after cholecystectomy; in some cases, such deficiency is pathogenetically caused by low gastric secretion). A significant advantage of lipase of microbial origin is the absence of the need for its activation by bile acids [11].
In the early 1970s. researchers from the University of Illinois Leveille et al. found that enzyme activity in tissues becomes weaker with age. Leveille conducted experiments on rats and found that at 18 months of age ("old age" for rats), enzyme activity on an enzyme-free diet was reduced by more than 20% of the level observed at one month of age. E. Howell agrees that “the more actively a young organism refuses its enzymes, the faster a state of enzyme deficiency or old age is achieved.” According to E. Howell, we live a long time, and our well-being is determined by our enzymatic potential. E. Howell cites a study by Meyer and colleagues at Michael Reese Hospital in Chicago, which reported that the amount of enzymes in the saliva of young people was 30 times higher than that of people over 69 years of age [12].
Characteristics of individual digestive enzymes
Amylase (released in an active state) performs a strictly defined function - the breakdown of polysaccharides. It begins to “work” in the oral cavity, then in the stomach, in symbiosis with the enzymes of the small intestine maltase, invertase and lactase, it breaks down polysaccharides in the intestine. It is the action of this enzyme that determines the quality of carbohydrate catabolism. Amylase deficiency is physiological in the first half of life. In this case, the child is not able to digest starch. Amylase usually reaches normal activity by the 9th month of life. A genetically determined amylase deficiency is possible (the gene is localized on the first chromosome). With amylase deficiency, the following symptoms appear: intolerance to foods rich in carbohydrates; frequent, loose, bulky stools (mushy, watery - with excess starch in food); malnutrition; isolated decrease in amylase activity in pancreatic juice, in combination with normal lipase and trypsin activity during cholecystokinin-secretin stimulation with normal intraduodenal pH values; high contamination of the intestines with opportunistic microbial flora; malabsorption syndrome; weight loss
Proteases (activated in the lumen of the duodenum) are hydrolytic enzymes capable of breaking down the bonds of peptides and proteins and restoring beneficial bacteria in the intestines. These include pepsin, trypsin, elastase and carboxypeptidases. The first two substances break down proteins with a large molecular structure, and carboxypeptidases convert peptides with a low molecular structure into amino acids. In addition, chymotrypsin is released, which breaks down proteins that remain after exposure to trypsin. Protease deficiency results in mushy (smelly) stools; severe creatorrhea, moderate steatorrhea; impairment of physical development; progressive malnutrition; hypoproteinemic edema (up to anasarca); anemia, neutropenia, reticulocytosis, bone marrow hypoplasia; total atrophy of intestinal villi.
Lipase (activated in the lumen of the duodenum) breaks down neutral fat into fatty acids and glycerol. During bile emulsification, lipases interact with other enzymes to convert fats into fatty acids in a multi-step process. Lipase deficiency causes steatorrhea, which is a criterion for the severity of exogenous pancreatic insufficiency.
The human body does not have enzymes that break down plant fiber - cellulases and hemicellulases; they are “produced” by representatives of the intestinal microflora. Fiber is not broken down in the small intestine, so it enters unchanged into the large intestine, where it is hydrolyzed by microbial enzymes (cellulase), which destroy cell membranes. Cellulase and hemicellulase increase the nutritional value of cereals, fruits and vegetables. They bind toxins and cholesterol in the digestive tract by releasing soluble fiber, thus stimulating digestion, intestinal motility and the growth of beneficial microflora. Normal microflora in the cecum breaks down and ferments 300–400 grams of fiber per day, producing short-chain fatty acids, glucose and gases, which also stimulate intestinal motility and bowel movements.
The main intestinal enzymes involved in the parietal hydrolysis of carbohydrates are α-glucosidases (maltase, trehalase, etc.), lactase, glucoamylase, invertase, etc.
Lactase is one of the main enzymes of the small intestine that improves the absorption of dairy products. Breaks down lactose (milk sugar) into glucose and galactose. In the absence or deficiency of lactase in the intestines, fermentation processes intensify. The occurrence of osmotic (fermentative) diarrhea is associated with the accumulation in the lumen of the distal parts of the small intestine and in the large intestine of an undigested, osmotically active disaccharide - lactose (lactose content in feces - more than 2 g%) and products of its bacterial fermentation. This can cause bloating and intestinal cramps. Taking lactase eliminates intolerance to milk sugar (lactose), which is found in many foods. But eliminating all foods containing lactose is difficult, since it is a very common component in many of them. Lactase-based replacement therapy for AF is the principle treatment method for hypolactasia [4].
Glucoamylase is an enzyme that catalyzes the release of D-glucose from the unreduced ends of starch or related oligo- and polysaccharide molecules and plays an important role in intracellular glycogen metabolism and energy production. It is synthesized by many microorganisms and is formed in animal tissues, especially in the liver, kidneys, placenta, intestines, etc.
Pectinase is an enzyme that breaks down pectin, a polysaccharide found in the cell membranes of plants, mainly in fruits. Normalizes the functioning of the digestive system, promotes the growth of beneficial intestinal microflora and improves the passage of digestive chyme through the gastrointestinal tract.
Isolated deficiencies of pancreatic and small intestinal enzymes occur, as a rule, with genetic diseases.
But the most common cause of digestive problems, as mentioned above, is dietary errors - eating too much food and its “heavy” chemical composition. Often a large feast is accompanied by the consumption of significant doses of alcohol, which disrupts the functioning of the pancreas. In this case, despite the adequate secretion of enzymes and their normal activity, symptoms similar to gastrogenic insufficiency occur in the human body (Table).
Digestive insufficiency is dangerous because part of the incoming food remains unchanged in the intestinal cavity, which leads to a change in the internal environment of the intestine (shift in acidity, chemical composition, osmotic pressure). This causes damage to the intestinal mucosa and the development of pathogenic microflora - the formation of bacterial overgrowth syndrome in the small intestine.
At the end of 2022, the dietary supplement Gastromed appeared on the Russian market, which, due to its composition, is capable of replenishing the deficiency of digestive enzymes both in case of pancreatic, gastro- and enterogenous insufficiency, and in case of errors in the diet, including banquet overeating. This product contains 75 mg of Natenzym D - enzymes that are a digestive enzyme complex from the products of yeast fermentation Aspergillus oryzae, described above in this article, and three phytocomponents. The enzyme part of the dietary supplement Gastromed is represented by the following enzymes:
- amylase 2250 units;
- protease 6375 U;
- lipase 112.5 U;
- cellulase 450 units;
- lactase 750 units;
- synthesized protease 2656 U;
- pectinase not less than 100 units;
- glucoamylase not less than 100 units.
The phytopart includes:
- 25 mg of yellow gentian roots (Gentiana lutea);
- 25 mg of common dandelion roots (Taraxacum officinale);
- 25 mg dry extract of milk thistle (Silybum marianum) seeds.
The phytocomponents included in the dietary supplement Gastromed are characterized by the following properties.
Gentian yellow contains bitter iridoid glycosides genciopicrin, gentinin, amarogentin, amarosverin, amaropanin, gentiacaumol, trisaccharide gentianose, alkaloid gentianin, gentiosterol, ascorbic acid, flavonoids, catechins, trace elements of molybdenum, selenium, boron. Bitter substances contained in the roots and rhizomes of gentian stimulate the secretion and motor function of the gastrointestinal tract, increase appetite, improve digestion and absorption of food.
Common dandelion roots contain triterpene compounds, sterols, choline, nicotinic acid, nicotinamide, rubber, resins, wax, inulin, fatty oil, organic acids (oleanolic, linoleic, palmitic, etc.). Dandelion is one of the medicinal plants containing bitterness. It is used to stimulate appetite and improve digestion. The reflex action of dandelion preparations is carried out by irritating the taste buds of the tongue and the mucous membrane of the oral cavity, which leads to stimulation of the food center, and then to increased secretion of gastric juice and the secretion of the digestive glands. The biologically active substances of dandelion also have choleretic, diuretic, antispasmodic and laxative properties. Inulin, which contains dandelion root, is a prebiotic. It is successfully fermented by bifidobacteria of the colon, stimulating its growth and metabolic activity. In turn, the undigested part of inulin is excreted from the body, “taking” with it breakdown products, cholesterol, toxins and other harmful substances.
The achenes of milk thistle contain about 32% fatty oil, flavonoids, including quercetin, resins, mucus, vitamin K, traces of alkaloids, biogenic amines (tyramine, histamine), flavonol lignans: silybin, silydianin, taxifolin, silychristin. Domestic and foreign literary sources describe the following pharmacological effects of medicinal forms from milk thistle: improving digestion, antioxidant, antitoxic, hemostatic, hepatoprotective, detoxification, choleretic, anti-inflammatory, wound healing, reparative, laxative, tonic, cholekinetic, cholesecretory [13, 14].
Thus, Gastromed, which is an original combination of seven enzymes and herbal extracts, can be prescribed as part of complex therapy to patients with mild chronic pancreatitis with normal results of the fecal elastase test, intestinal dyspepsia of various etiologies, diabetes mellitus, irritable bowel syndrome, for the preparation for X-ray or ultrasound examination. Also, indications for prescribing the dietary supplement Gastromed are primary (congenital) and secondary (due to diseases of the small intestine) lactase deficiency. And of course, Gastromed will be necessary for people following various diets or overeating.
Literature
- Kalinin A.V. Disturbance of cavity digestion and its drug correction // Clinical perspectives in gastroenterology, hepatology. 2001; 3: p. 21–25.
- Mayev I.V., Kucheryavyi Yu.A. Diseases of the pancreas. GEOTAR-Media, 2009. 736 p.
- Dzhambekova O. B., Dolgenko N. V., Tleubaeva A. B. Clinical aspects of multienzyme replacement therapy // Bulletin of KazNMU. 2013; 4 (1): p. 252–256.
- Gubergrits N. B., Belyaeva N. V., Klochkov A. E., Lukashevich G. M., Fomenko P. G. Advantages and therapeutic capabilities of digestive enzyme preparations of non-animal origin // Bulletin of the Pancreatology Club. 2018; 1: p. 26–31.
- Griffin SM, Alderson D., Farndon JR Acid resistant lipase as replacement therapy in chronic pancreatic exocrine insufficiency: a study in dogs // Gut. 1989; 30: 1012–1015.
- Howell E. The status of food enzymes in digestion and metabolism. Chicago, Ill., National Enzyme Co. 1946.124 rub.
- Christensen T., Woeldike H., Boel E., Mortensen SB, Hjortshoej K., Thim L., Hansen MT High level expression of recombinant genes in Aspergillus oryzae // Bio/Technology. 1988; 6:1419–1422.
- Schneider M.U., Knoll-Ruzicka M.L., Domschke S. et al. Pancreatic enzyme replacement therapy: Comparative effects of conventional and enteric-coated microspheric pancreatin and acid-stable fungal enzyme preparations on steatorrhea in chronic pancreatitis // Hepatogastroenterol. 1985; 32:97–102.
- Rachman B. Unique features and application of non-animal derived enzymes // Clin. Nutr. Insights 1997; 5 (10): 1–4.
- Howell E. Food Enzymes for Health & Longevity, Lotus Press, Twin Lakes, WI, 1994, 2nd ed.
- The pancreas: an integrated textbook of basic science, medicine and surgery / Eds.: HG Beger., Malden: Blackwell Publishing, 2008. 1006 p.
- Howell E. Enzyme Nutrition: The Food Enzyme Concept 1986. Twin Lakes, WI: Lotus Press.
- Karpeev A. A., Kiseleva T. L., Korshikova Yu. I., Lesiovskaya E. E., Sakanyan E. I. Herbal medicine: Methodological recommendations of the Ministry of Health of the Russian Federation. In the book: Herbal medicine: normative documents / Ed. ed. A. A. Karpeeva, T. L. Kiseleva. M.: Publishing house FNKETS TMDL Roszdrav. 2006. pp. 9–42.
- Sokolov S. Ya. Herbal medicine and phytopharmacology: A guide for doctors. M.: Medical Information Agency, 2000. 976 p.
E. Yu. Plotnikova, Doctor of Medical Sciences, Professor
Federal State Budgetary Educational Institution of Higher Education Kemerovo State Medical University, Ministry of Health of the Russian Federation, Kemerovo
Contact Information
The role of enzymes of non-animal origin in digestive disorders of various etiologies / E. Yu. Plotnikova For citation: Attending physician No. 1/2019; Issue page numbers: 56-61 Tags: digestion, disorders, herbal supplements, digestive enzymes
What factors influence the production of enzymes
If we evaluate the role enzymes play in the digestion process, they can be compared to a huge mechanism for processing food. In a healthy body, all enzymes will normally be produced in sufficient quantities. But the process of their synthesis is quite complex, so the production of substances requires certain conditions. The key factors influencing the work and functionality of enzymes include:
- Acidity
- the stomach is predominantly acidic, while other parts of the digestive system are alkaline. When consuming large amounts of food with high acidity, dysbiosis and other disorders that affect pH, the functionality of enzymes may decrease; - Body temperature
- the usual body temperature in the gastrointestinal tract is 37 degrees. When the temperature changes above or below normal, food absorption will be disrupted. Also, with an increase in body temperature, denaturation of protein structures occurs, which is why the work of enzymes can completely stop; - Inflammatory processes
- disruption of the main tasks and role of digestive enzymes in the digestion process can cause pathologies. These include duodenitis, ulcers, pancreatitis, hepatitis and others; - Balanced diet and quality of nutrition
- disturbances can occur when one type of food is excessively predominant. This leads to an increase in the load on the gastrointestinal tract and a deterioration in the absorption of food; - Exposure to toxic substances
- when poisoned by certain poisons that inhibit protein synthesis.
Treatment of dyspepsia
Before starting treatment for intestinal dyspepsia, the type of disease is determined in order to select the right diet on the first day of therapy. In case of nutritional dyspepsia, the patient is advised to completely abstain from eating for two days. The transition to a normal diet should be gradual and consistent. In the case of fermentative dyspepsia, the patient should abstain from foods rich in carbohydrates. For fatty dyspepsia, a low-fat diet is prescribed; for putrefactive dyspepsia, the patient must limit the intake of protein foods. Treatment of enzymatic dyspepsia requires taking medications containing digestive enzymes.
Treatment of functional dyspepsia
Diet therapy and giving up bad habits play a very important role in the treatment of functional dyspepsia. Nicotine, alcohol, coffee, disrupting gastrointestinal motility, can provoke relapses of the disease. A balanced diet for patients in this case involves frequent and small meals, and it is recommended to significantly reduce the content of saturated fatty acids in their diet.
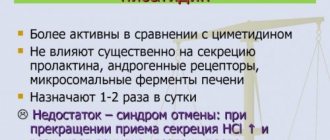
In the dyskinetic form of the pathology, the main drugs for the treatment of dyspepsia are prokinetics (metoclopramide and domperidone), which have a beneficial effect on the motor function of the gastrointestinal tract. It should be remembered that in 20-30% of patients, metoclopramide, especially with long-term use, causes undesirable side effects from the central nervous system in the form of drowsiness, fatigue and anxiety, therefore the drug of choice for the treatment of functional dyspepsia is domperidone, which does not cause such side effects.
Treatment of intestinal dyspepsia
Treatment of fermentative dyspepsia consists of limiting, or better yet completely eliminating, carbohydrates from the diet for 3-4 days. The general condition of patients with this form of dyspepsia suffers slightly. Acute fermentative dyspepsia can be quickly eliminated with the right diet. However, sometimes if the dietary regimen is not followed, dyspepsia can become chronic. The aggravating factor is achylia. Dyspepsia in some cases can develop into chronic enteritis and chronic enterocolitis. After 1-2 fasting days, you should prescribe an increased amount of proteins (cottage cheese, lean meat, boiled fish), meat broth with a small amount of white bread. In the future, water porridge, fruit purees and jelly are gradually included in the diet (see Diet No. 4 according to Pevzner). After 2-3 weeks, vegetables and fruits are allowed.
If diarrhea does not go away quickly, prescribe calcium carbonate 0.5-1 g 3-4 times a day, magnesium perhydrol 0.5 g 3 times a day. For a long time, the consumption of vegetables rich in coarse plant fiber is prohibited - cabbage, legumes, cucumbers, beets, etc.
Treatment of putrefactive dyspepsia also involves prescribing a diet. After one hungry day, they switch to a diet rich in carbohydrates. It is advisable to prescribe fruit juices and grated apples 1-1.5 kg per day for 2-3 days. Then the diet includes mucous infusions of rice, semolina porridge with water, crackers, and white bread. After 5-7 days, add butter, fresh lean fish, chicken, vegetable soups, mashed potatoes or carrots. Among medications, natural gastric juice, bismuth nitrate, pancreatin, and chloramphenicol are recommended.
Treatment of fatty dyspepsia comes down to limiting the amount of fat consumed in food. The diet includes complete animal proteins: lean meat, low-fat cottage cheese, boiled fish, etc. The consumption of carbohydrates is moderately limited. Medicines prescribed include calcium carbonate, bismuth, and vitamins - ascorbic acid, nicotinic acid, cyanocobalamin.
LDC "Neuron"
- < Back
- Forward >
Main signs of enzyme deficiency
To stay healthy, you don't need to fully understand the role enzymes play in digestion. But recognizing signs of enzyme deficiency will help you take timely measures: normalize your diet, add various supplements or medications, etc.
The most obvious and common signs of enzyme deficiency or dysfunction include:
- Belching;
- Heartburn;
- Frequent constipation or diarrhea;
- Flatulence;
- Increased fatigue, drowsiness, especially after eating;
- Aching pain.
It is also important to find the reasons for the shortage. Scientists classify two types of deficiency: primary or genetic and secondary (acquired). The primary deficiency cannot be corrected; it is a genetic problem. As a result, undigested products remain in the body, which in the case of protein structures can be life-threatening.
The secondary type includes any changes that occur as a result of disruption of the gastrointestinal tract, changes in diet and other problems. For example, one of the most common causes of enzyme deficiency is a lack of vitamin PP. This also happens with gastritis, pancreatitis, etc.
Enzyme deficiency is another chronic disease that occurs due to poor diet. With the predominance of certain foods, an abundance of fatty and fried foods, frequent overeating and other deviations, the work of enzymes will also be inhibited. This is also one of the main reasons for the spread of Helicobacter pylori, which is considered the main provocateur of gastritis and peptic ulcers. If such problems arise, long-term treatment is necessary, the key element of which will be the normalization of the diet.
Symptoms of dyspepsia
Symptoms of dyspepsia can manifest themselves in different ways, depending on the specific type of disorder, but there are signs that are simultaneously characteristic of all types of the disease.
Different types of dyspepsia have the following common symptoms:
- the appearance of unpleasant sensations in the so-called espiral area, that is, in the upper abdomen. The patient experiences feelings of bloating and heaviness, sometimes pain of varying intensity occurs;
- belching. Rare isolated cases of belching are not signs of the disease. Dyspepsia is indicated only by constant frequent belching;
- nausea, heartburn. The patient experiences an unpleasant burning sensation in the upper abdomen, as well as in the chest area. This sensation appears when aggressive stomach contents enter the esophagus. Normally, such phenomena should not happen;
- flatulence. A feeling of bloating, as well as increased gas production, can be caused by increased formation of gases in the intestines;
- bowel disorder. Patients who suffer from dyspepsia have irregular, usually frequent, bowel movements.
Dyspepsia, which is caused by a lack of digestive enzyme, has the following symptoms:
- nausea;
- unpleasant taste in the mouth;
- transfusion and rumbling in the abdomen, malaise, weakness;
Sometimes patients experience headaches and insomnia. Stool often contains large amounts of food that is poorly digested.
Functional dyspepsia is manifested by such unpleasant symptoms as pain, discomfort in the pancreas after eating, accompanied by heaviness, fullness, and early satiety.
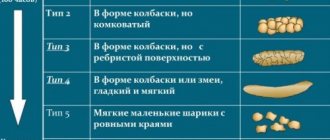
Fermentative dyspepsia. The main symptoms of fermentative dyspepsia are bloating of the intestines with the release of a large amount of gases, frequent liquid foamy stools with a sour odor. Abdominal pain is tolerable or absent. A very typical sign of fermentative dyspepsia is the nature of bowel movements. They are lightly colored, contain few gas bubbles, a large amount of starch grains, fiber, iodophilic microbes and organic acids.
Putrid dyspepsia is in many ways reminiscent of intoxication: the patient feels weakness and general malaise, feels nausea and a severe headache. The stool is dark and liquid, has an unpleasant and rather pungent odor, and stools are frequent.
Fatty dyspepsia , unlike other types of dyspepsia, is not characterized by frequent diarrhea. Patients suffering from fatty dyspepsia experience a feeling of fullness and heaviness in the abdomen, complain of flatulence and belching, as well as severe pain that begins half an hour after eating. Feces have a whitish color and a greasy sheen: these are the remains of fat that does not have time to be digested. The stool is plentiful.
Dyspepsia in young children manifests itself in regurgitation and bloating. The stool is frequent, more than six times a day, the stool is green, and there are whitish flakes. At the same time, the child is capricious, sleeps and eats poorly.
How to improve enzyme production
Strategies for normalizing the functioning and production of food enzymes may vary, but they all usually boil down to key aspects:
- Normalization of the diet - eliminating the causes of deficiency, controlling portions and the total amount of food consumed. Switching to healthier foods (minimizing fried, smoked, salted and other unhealthy foods);
- Restoration of intestinal microflora and consumption of supplements that affect the activity of microflora in the gastrointestinal tract.
Also, the use of supplements is an excellent way to prevent various diseases, improve food absorption, reduce the load on the digestive organs and avoid other problems.
Top Supplements for Enzyme Recovery:
- NOW Gr8-Dophilus
is a popular complex that includes 8 types of probiotics found in the gastrointestinal tract. They normalize microflora, improve peristalsis, restore the functioning and synthesis of enzymes; - Beta Glucans
is a supplement with comprehensive health benefits. Increases immunity, improves the functioning of the gastrointestinal tract, promotes the elimination of toxins and waste; - Stabilized Acidophilus Three Billion
from NOW is the latest complex with a powerful effect. It is adicophilus, restores intestinal microflora, normalizes the functioning of the stomach and other gastrointestinal organs. Inhibits harmful bacteria, suppresses inflammatory processes, fermentation and other diseases; - Super Digestawa enzyme mixture
is a complex that contains enzymes for the digestion of proteins, fats and carbohydrates. It is used not only as a prophylactic agent, but also restores microflora after various diseases. Also used in sports for better absorption of food; - NOW Super Enzymes is a complex that includes almost all types of enzymes. Provides comprehensive restoration of the gastrointestinal tract, improves digestion, promotes better absorption of fats, proteins and carbohydrates.
- Womens Probiotic
from MRM is a popular complex for women. Restores not only the microflora of the intestines and gastrointestinal tract, but also prevents diseases of the mucous membrane of the genital organs. It is also used to restore microflora after the use of antibiotics and other medications.