General description of the disease
This is an acute inflammation of the perirectal cellular tissue. Approximately 30% of all diseases of the rectum occur specifically in it. In most cases, paraproctitis is caused by polymicrobial flora. During inoculation of purulent contents, staphylococci, Escherichia coli, gram-positive and gram-negative bacilli are usually detected. As a rule, the disease begins abruptly and is accompanied by pronounced symptoms, discomfort, and severe pain. Requires urgent and immediate treatment.
Causes that provoke the occurrence of paraproctitis
The cause of paraproctitis is an infection that, when it gets into the soft tissues located around the anus, causes inflammation and abscesses. The infection enters through wounds caused by diarrhea or constipation, hemorrhoids, and anal injuries. Sometimes it is quite difficult to establish the exact cause of a disease in a particular person. Even an accidentally swallowed bone or egg shell, which comes out along with the feces, can injure the intestines.
Among other common causes of paraproctitis, doctors also name the following:
- dilation and inflammation of hemorrhoidal veins;
- anal fissure;
- inflammatory diseases of the rectum and other parts of the intestine;
- bowel disorders (diarrhea, constipation);
- immunodeficiency;
- chronic inflammation in any system of the body.
Types of paraproctitis
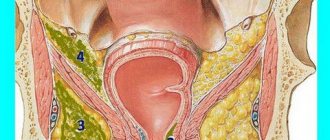
Depending on the location, there are several classifications of the disease.
- 1 Subcutaneous paraproctitis . An abscess appears directly under the skin, signs of the disease are noticeable even just upon examination; this is the most common type of disease.
- 2 Submucosal paraproctitis . Purulent paraproctitis occurs in the rectum under the mucous membrane.
- 3 Ischiorectal . The inflammation spreads to the muscle that is responsible for raising the anus.
- 4 Pelviorectal . The inflammation spreads to the levator ani muscles and acts through it on the pelvic muscles. Due to its wide distribution, this type of paraproctitis is the most dangerous.
In addition, inflammation can be deep or superficial.
Symptoms of paraproctitis
This disease begins suddenly and is characterized by rapid clinical manifestations. Here are the common symptoms that may appear in the first hours after the onset of the disease:
- pain around the rectum and anus. Pain can penetrate into the groin and perineum, as well as into the abdominal cavity; It intensifies during defecation.
- frequent and false urge to defecate, but constipation is also possible.
- painful urination;
- signs of intoxication such as fever, weakness, pallor, loss of appetite and dizziness; the temperature can rise to 39 degrees.
These symptoms appear in all types of paraproctitis and do not depend on its location. However, each type of pathology develops its own typical symptoms, which help determine where exactly the inflammation has occurred.
With subcutaneous paraproctitis , when the abscess is located near the anus under the skin, the symptoms are most noticeable: painful swelling in the anus, with redness of the skin above it. The pain gradually increases, acquiring an intense pulsating character, bringing enormous discomfort when sitting or defecating. These processes are accompanied by severe pain. This form of abscess is the most common.
A submucosal abscess is located under the mucous membrane of the rectum. The symptoms of this type of location are similar to a subcutaneous abscess, but the pain and skin changes are less pronounced.
With an ischeorectal abscess, the purulent focus is located above the muscle that lifts the anus. Due to the deep abscess, local symptoms are more vague: dull throbbing pain in the pelvis and rectum, which intensifies during bowel movements. Redness of the skin and swelling occurs 5-6 days after the onset of pain. The general feeling is heavy: the temperature can rise to 38 degrees, and severe intoxication is observed.
The most difficult is considered to be pelviorectal abscess . This is a rare form of acute abscess, when the purulent focus is located above the muscles that form the pelvic floor, it is separated from the abdominal cavity by a thin layer of peritoneum. The onset of the disease is accompanied by high fever, chills, and joint pain. Local symptoms: pain in the hip joint and abdominal cavity. After 10-12 days, the pain intensifies, stool and urine retention occurs.
Some people are diagnosed with isolated necrotizing paraproctitis . This form is characterized by the rapid spread of the abscess, accompanied by extensive necrosis of the soft tissues and requiring their removal, after which large scars remain, requiring the intervention of a plastic surgeon.
Paraproctitis in children
Most often, paraproctitis occurs in people over 20 years of age, but children are also at risk. Symptoms in children are the same as in adult patients, but diagnosing the disease is more difficult, since children cannot always describe what exactly is bothering them.
Parents should pay special attention to fever, frequent crying of the baby, especially during bowel movements, and constipation. As a rule, children suffer from subcutaneous paraproctitis, hence the skin around the anus is red and swollen.
Causes of paraproctitis in children:
- abnormalities of the glands in the rectum;
- decreased immunity;
- inflammation of the intestines and respiratory system;
- intestinal dysbiosis.
Complications with paraproctitis
If purulent paraproctitis does not break out in time, dangerous complications may arise:
- purulent formation can damage the intestinal walls and vaginal walls in women;
- with subcutaneous localization, the destruction of the abscess can be external, which leads to additional infections;
- damage to fatty tissue in the pelvic area;
- damage to the urethra caused by purulent infiltration;
- peritonitis due to the rapid spread of inflammation to the abdominal cavity;
The postoperative period can also be difficult. Even if the surgeon follows all the rules of surgery, bleeding, infectious complications and other postoperative problems may occur.
Prevention of paraproctitis
There are no specific preventive measures for this disease. It is necessary to promptly and correctly treat all rectal disorders. Chronic infections of other body systems should not be ignored. Proper intimate hygiene is very important. It is necessary to regularly visit a doctor for preventive examinations, and not to delay going to a specialist when the body begins to show alarming signs: pain, discomfort, weakness, etc.
Diagnostics
The diagnosis of paraproctitis is usually made on the basis of studying the clinical picture, as well as after conducting a digital examination of the rectum. During such an examination, a physician wearing special gloves inserts a finger into the anus and easily feels the walls of the rectum. In this case, the patient can lie on his side or on his back, in a gynecological chair. This is most often quite enough.
In rare cases, especially in very advanced or complicated forms of the disease, an instrumental examination using rectoscopy (endoscopic examination) or ultrasonography (insertion of an ultrasound sensor into the rectum) is prescribed.
Treatment of paraproctitis in official medicine
Acute paraproctitis is an emergency disease and requires surgical treatment.
Anesthesia plays a very important role in the treatment of acute paraproctitis. The operation is performed under general anesthesia, and doctors must make the patient's muscles as relaxed as possible. Surgery for paraproctitis requires compliance with some important rules to remove purulent inflammation:
- abscess incision;
- abscess drainage;
- detection of the affected area of the intestine and its removal.
Sometimes inexperienced doctors only perform an incision and drainage of the abscess to treat paraproctitis, which can lead to either relapse or anal fistulas.
During the postoperative period, the patient must take antibiotics to prevent recurrence of paraproctitis. They also prevent infection of other body systems and complications such as sepsis or peritonitis.
During the recovery period, it is very important to maintain proper intimate hygiene. The rectal area is washed twice a day in the morning and evening and after each bowel movement to prevent infection of the postoperative wound.
General rules
A common proctological disease is paraproctitis - purulent inflammation of the tissue surrounding the rectum. The reason is infection by various microorganisms. They can penetrate into the cellular spaces from the rectum during anal fissures, hemorrhoids , traumatic manipulations or anal sex. The infectious factor enters the perirectal tissue and causes acute inflammation ( abscess ), which, if treated inappropriately, can become chronic.
In a chronic course, prolonged inflammation leads to the formation of fistula tracts. In some cases, there are several passages opening outwards or into the rectum. The onset of the disease is acute: high fever, chills , pain in the anus, pain during bowel movements. Acute paraproctitis is treated surgically - opening the abscess and draining the cavity. In case of a chronic disease with a fistula tract, the operation is more complex and extensive, since it is necessary to identify and excise the fistulous tract. Often the operation is performed in two stages.
Rehabilitation treatment lasts at least a month (sometimes it lasts for 6 months - it depends on the volume of the operation) since the surgical wound is subject to daily infection and traumatization by feces. The main task is to carry out daily wound care, baths, microenemas, local anti-inflammatory treatment and the use of agents that promote tissue repair. Treatment after surgery also includes proper nutrition and changes in diet. 12 hours after opening the abscess, you can only drink water and then start eating. In this case, it is necessary to fulfill the general requirements:
- Eating according to the schedule, 4-5 times a day in small portions.
- Mandatory inclusion of liquid food in the form of vegetable puree soup or broth.
- Meat, fish, lean poultry, cooked by boiling or steaming. At first, it is prepared in pureed form or as minced meat.
- Light dinner without meat dishes (porridge, dairy products).
- Elimination of foods that cause bloating (legumes, grapes, raw apples, grapes, raisins, kvass).
- Limiting simple carbohydrates (sugar, jam, buns and other yeast baked goods, bread, sweets).
- Exclusion of salty, hot, smoked, sour and spicy foods.
- Drinking alcohol is not allowed.
The diet for paraproctitis after surgery in the first three days is very limited and contains:
- Liquid pureed porridges (oatmeal, buckwheat, rice are excluded for constipation).
- Broths (vegetable and weak meat).
- Omelettes or soft-boiled eggs.
- Mashed cottage cheese.
- Steamed cutlets made from lean meat and fish.
- Vegetable fiber in the form of vegetable purees or grated beets, steamed prunes. This point is very important in nutrition, since its main task is to normalize stool and achieve easy bowel movements.
- In addition to this, the patient should drink a lot of regular filtered water (at least one and a half liters per day), prune decoctions, excluding carbonated drinks and juices, which can cause bloating.
From day 4, the diet expands, however, it should not contain spicy and fried foods, unprocessed fruits and vegetables, carbonated drinks, strong tea and coffee. The products must be dietary, and the preparation must be fully consistent with a healthy diet. If independent stool is not restored within three days, yogurt with bran is introduced into the diet. Most often, from the first day it is recommended to take Vaseline oil, which promotes easy emptying. In severe cases, they resort to a cleansing enema.
The diet after surgery for 3 months should not contain irritating foods:
- spicy;
- sour;
- canned food;
- spices;
- peppers of any kind, onions, garlic;
- alcohol.
The patient's diet is adjusted depending on intestinal function (tendency to constipation or diarrhea ). For constipation, the patient should have daily bowel movements, and the stool should have a soft consistency - this will eliminate the risk of injury to the mucous membrane and speed up the healing process.
Products containing dietary fiber are introduced into the diet in large quantities - they enhance peristalsis and help soften stool. Therefore, it is necessary to consume more cereals, vegetables (beets, carrots, pumpkin), boiled or baked fruits, seaweed and dried fruits (primarily figs, prunes), and dried fruit compotes.
White bread is replaced with whole grain bread and additional bran (wheat, oat) or psyllum (plantain seed shell) is introduced. Juices with pulp (beetroot, carrot, pumpkin) can be used as drinks. It is worth paying attention to kefir, fermented baked milk, yogurt.
In case of diarrhea, on the contrary, dried fruits, vegetables and fruits are significantly limited, and jelly made from fruits that have a tanning effect (quince, bird cherry, dogwood) is recommended.
How to treat rectal fistula?
The tactics and composition of therapy are determined by the type and stage of the disease, as well as the patient’s physical health.
Thus, information about the number of fistulas, their size and characteristics, the nature of the discharge from them, as well as the presence of cicatricial changes in the intestinal wall carries important diagnostic significance.
Before prescribing a course of therapy, differential diagnosis must be carried out, since the choice of treatment method is directly dependent on the data obtained.
Often the examination includes:
- probing the fistula tract to determine its direction, the presence of purulent pockets and branches in it;
- fistulography (x-ray contrast study);
- anoscopy to assess the shape and length of the fistula canal;
- sigmoidoscopy to identify concomitant pathologies of the sigmoid and rectum;
- sphincterometry to determine the tone of the sphincter and the degree of its closing function;
- Ultrasound of pararectal tissue spaces;
- use of methylene blue (dye test);
- cytological scraping and histological analysis of the fistula tract, etc.
The only effective way to treat rectal fistula is surgery. Depending on the characteristics of the pathology and the duration of its course, certain methods of removing a rectal fistula are used.
Among the methods of excision of a fistula there are:
- an incision followed by suturing of the sphincter muscles (especially when deep tissues are affected);
- dissection;
- laser cauterization;
- excision followed by plastic surgery;
- filling with biomaterials;
- application of ligatures, etc.
A ligature is a silk thread that is inserted along the fistula and tied, completely covering the muscle layer of the anus. During dressings, the ligature is gradually tightened, which leads to dissection of the sphincter muscles, maintaining its functionality.
But the most popular and effective method of surgical treatment is minimally invasive intervention, since it not only successfully eliminates pathology, but also reduces postoperative risks and shortens the recovery period.
Today, the Austrian disposable instrument FiXcision is used to simultaneously excise the fistula and restore the integrity of the rectum.
The advantages of using FiXcision during minimally invasive surgery are its ability to:
- probing;
- tissue compression;
- excision of the fistula with a circular blade (followed by histological examination of the material).
The use of FiXcision can significantly speed up the surgical procedure; it lasts about 30 minutes and does not require general anesthesia or hospitalization of the patient.
However, there are a number of contraindications for the procedure, including:
- serious diseases of the kidneys, cardiovascular and respiratory systems;
- blood diseases;
- diabetes;
- acute infectious process;
- presence of tumors;
- an episode of acute paraproctitis less than 8 months before the procedure, etc.
According to clinical data, opening and draining the abscess without closing the fistula itself leads to the re-formation of a rectal fistula, so subsequent surgery is necessary for a complete recovery and prevention of relapse.
Authorized Products
The diet for paraproctitis should include:
- Soups only contain vegetable broths (or weak meat broths) with the addition of cereals and vegetables. In the first days after surgery, soups are pureed or prepared in the form of pureed soups. This will not be necessary later. Soups are prepared without frying vegetables.
- Dried bread - wheat, rye, if there is no bloating, or with bran for constipation.
- The only condition is to eat stale bread, as it does not cause bloating.
- The amount of baked goods should be reduced in case of constipation.
- Dishes made from beef, turkey, rabbit or chicken, boiled or steamed.
- Immediately after the operation they are prepared as minced meat or chopped, and subsequently consumed in pieces.
- Low-fat sea or river fish. The cooking methods are the same. The fish can be baked. The amount of meat consumed is limited if you are prone to constipation.
- Omelettes or soft-boiled eggs.
- Porridge - buckwheat, oatmeal, wheat, a lot of cereals. Rice porridge is excluded if you are prone to constipation, and oatmeal should not be boiled and turned into a slimy, sticky porridge, since in this form it can cause constipation. Pasta and noodles (including those made from buckwheat and rice flour) may be present in the diet, however, it is worth remembering that all flour and pasta products are undesirable for constipation.
- Low-fat dairy products, including fermented milk. Milk is consumed as tolerated. Low-fat cottage cheese can be eaten in its natural form or added to various dishes (casseroles, cheesecakes, puddings).
- Vegetables are initially introduced in boiled or stewed form (puree). You can use zucchini, pumpkin, beets, potatoes, cauliflower and Brussels sprouts. Legumes and white cabbage should be excluded if they cause bloating. With the transition to a common table (after 1.5-2 months), vegetables can be consumed raw, and their quantity should be increased if there is constipation. Vegetable oil is added to salads.
- Non-acidic fruits and berries are first consumed in processed form (baked, boiled, stewed), and then raw. For constipation, it is advisable to include dried apricots, prunes, cherries, plums, cherries, peaches, apricots and bananas in your diet.
- Sweets are limiting. Honey and homemade jam are allowed for tea and in dishes with cottage cheese.
- Drinks: herbal teas, still water, bran decoction, vegetable juices (for constipation, plum, apricot, peach, carrot, pumpkin), rosehip infusion.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| eggplant | 1,2 | 0,1 | 4,5 | 24 |
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| broccoli | 3,0 | 0,4 | 5,2 | 28 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| salad pepper | 1,3 | 0,0 | 5,3 | 27 |
| parsley | 3,7 | 0,4 | 7,6 | 47 |
| iceberg lettuce | 0,9 | 0,1 | 1,8 | 14 |
| tomatoes | 0,6 | 0,2 | 4,2 | 20 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
| dill | 2,5 | 0,5 | 6,3 | 38 |
Fruits | ||||
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Nuts and dried fruits | ||||
| raisin | 2,9 | 0,6 | 66,0 | 264 |
| dried figs | 3,1 | 0,8 | 57,9 | 257 |
| dried apricots | 5,2 | 0,3 | 51,0 | 215 |
| dried apricots | 5,0 | 0,4 | 50,6 | 213 |
| prunes | 2,3 | 0,7 | 57,5 | 231 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| oat groats | 12,3 | 6,1 | 59,5 | 342 |
| rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| pasta | 10,4 | 1,1 | 69,7 | 337 |
| noodles | 12,0 | 3,7 | 60,1 | 322 |
| buckwheat noodles | 14,7 | 0,9 | 70,5 | 348 |
Bakery products | ||||
| bran bread | 7,5 | 1,3 | 45,2 | 227 |
| whole grain bread | 10,1 | 2,3 | 57,1 | 295 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
Dairy | ||||
| kefir 1.5% | 3,3 | 1,5 | 3,6 | 41 |
| Ryazhenka | 2,8 | 4,0 | 4,2 | 67 |
Cheeses and cottage cheese | ||||
| cottage cheese 1% | 16,3 | 1,0 | 1,3 | 79 |
Meat products | ||||
| beef | 18,9 | 19,4 | 0,0 | 187 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken breast | 29,8 | 1,8 | 0,5 | 137 |
| boiled chicken drumstick | 27,0 | 5,6 | 0,0 | 158 |
| boiled turkey fillet | 25,0 | 1,0 | — | 130 |
Eggs | ||||
| soft-boiled chicken eggs | 12,8 | 11,6 | 0,8 | 159 |
Fish and seafood | ||||
| flounder | 16,5 | 1,8 | 0,0 | 83 |
| pollock | 15,9 | 0,9 | 0,0 | 72 |
| cod | 17,7 | 0,7 | — | 78 |
| hake | 16,6 | 2,2 | 0,0 | 86 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| olive oil | 0,0 | 99,8 | 0,0 | 898 |
| sunflower oil | 0,0 | 99,9 | 0,0 | 899 |
Non-alcoholic drinks | ||||
| water | 0,0 | 0,0 | 0,0 | — |
| mineral water | 0,0 | 0,0 | 0,0 | — |
| green tea | 0,0 | 0,0 | 0,0 | — |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| peach juice | 0,9 | 0,1 | 9,5 | 40 |
| plum juice | 0,8 | 0,0 | 9,6 | 39 |
| tomato juice | 1,1 | 0,2 | 3,8 | 21 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| rose hip juice | 0,1 | 0,0 | 17,6 | 70 |
| * data is per 100 g of product | ||||
Rehabilitation after paraproctitis removal
You need to spend several days in the hospital. In the early postoperative period after removal of a rectal fistula, there is a pronounced pain syndrome, an increase in body temperature and a deterioration in general health are possible. If possible, unpleasant symptoms are relieved. A course of antibiotics is required, usually intramuscularly.
One of the main aspects is hygiene. The wound healing process can be complicated by hair growing in the anal area. They need to be shaved or cut off so that there are no problems with treating the wound. Depilatory creams cannot be used. After each bowel movement, you need to thoroughly clean the anal area not only with toilet paper, but also with a disinfectant. You can do sitz baths with disinfectants or herbs. When going to the toilet there may be minor discharge and slight bruising. If the bleeding is severe, you should immediately consult a doctor.
An important part of rehabilitation is nutrition. Salty and spicy foods, sour foods, fresh fruits, alcohol, and sweet carbonated drinks should be excluded from the diet. There should not be “harmful” foods in the diet, that is, semi-finished products, chips, fast food. To improve the digestion process, you need to eat as much cereal as possible, dishes high in dietary fiber, and drink more clean water.
Every day after surgery to remove a rectal fistula, it is necessary to clean the sutures and make dressings. Sutures are usually treated with Chlorhexidine or antibacterial ointments. One of the best is Levomekol. Additionally, agents that accelerate healing are used. In some cases, physical therapy is prescribed to speed up recovery. These are magnetic therapy and UV irradiation.
Our surgery center features:
- more than 15 highly qualified surgeons on staff;
- the latest equipment;
- postoperative recovery of patients within 1 day.
Fully or partially limited products
- Spicy seasonings, dishes and sauces: horseradish, Tabasco, mustard, any pepper, ketchup.
- Garlic, onion, radish, radish.
- Legumes, white cabbage, kvass, black bread, any fresh bread and baked goods if you are prone to flatulence .
- Fatty meat and fish, sausages, smoked meat and fish, goose and duck meat, salted fish, canned food (meat, fish, vegetables).
- Strong black coffee and tea (especially for constipation), chocolate, cocoa.
- Limit animal fats, full-fat milk and cream.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| canned vegetables | 1,5 | 0,2 | 5,5 | 30 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| peas | 6,0 | 0,0 | 9,0 | 60 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| chickpeas | 19,0 | 6,0 | 61,0 | 364 |
| radish | 1,2 | 0,1 | 3,4 | 19 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| beans | 7,8 | 0,5 | 21,5 | 123 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Berries | ||||
| grape | 0,6 | 0,2 | 16,8 | 65 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
| marinated mushrooms | 2,2 | 0,4 | 0,0 | 20 |
Nuts and dried fruits | ||||
| nuts | 15,0 | 40,0 | 20,0 | 500 |
| almond | 18,6 | 57,7 | 16,2 | 645 |
Snacks | ||||
| potato chips | 5,5 | 30,0 | 53,0 | 520 |
Cereals and porridges | ||||
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
Flour and pasta | ||||
| vareniki | 7,6 | 2,3 | 18,7 | 155 |
| dumplings | 11,9 | 12,4 | 29,0 | 275 |
Bakery products | ||||
| buns | 7,9 | 9,4 | 55,5 | 339 |
Confectionery | ||||
| pastry cream | 0,2 | 26,0 | 16,5 | 300 |
| shortbread dough | 6,5 | 21,6 | 49,9 | 403 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Chocolate | ||||
| chocolate | 5,4 | 35,3 | 56,5 | 544 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
Dairy | ||||
| milk 4.5% | 3,1 | 4,5 | 4,7 | 72 |
| cream 35% (fat) | 2,5 | 35,0 | 3,0 | 337 |
| whipped cream | 3,2 | 22,2 | 12,5 | 257 |
Meat products | ||||
| fatty pork | 11,4 | 49,3 | 0,0 | 489 |
| salo | 2,4 | 89,0 | 0,0 | 797 |
| bacon | 23,0 | 45,0 | 0,0 | 500 |
Sausages | ||||
| smoked sausage | 9,9 | 63,2 | 0,3 | 608 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
| salmon | 19,8 | 6,3 | 0,0 | 142 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
| salmon | 21,6 | 6,0 | — | 140 |
| trout | 19,2 | 2,1 | — | 97 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Alcoholic drinks | ||||
| dry red wine | 0,2 | 0,0 | 0,3 | 68 |
| vodka | 0,0 | 0,0 | 0,1 | 235 |
| beer | 0,3 | 0,0 | 4,6 | 42 |
Non-alcoholic drinks | ||||
| soda water | 0,0 | 0,0 | 0,0 | — |
| cola | 0,0 | 0,0 | 10,4 | 42 |
| instant coffee dry | 15,0 | 3,5 | 0,0 | 94 |
| sprite | 0,1 | 0,0 | 7,0 | 29 |
| * data is per 100 g of product | ||||
Menu (Power Mode)
The duration of the diet depends on the patient’s condition and the reparative capabilities of the tissues. Paraproctitis is usually accompanied by chronic proctitis (recurrent inflammation of the rectal mucosa), in which constant gentle nutrition is important, excluding spicy and fried foods.
The menu is quite varied and it is important to monitor the alternation of protein dishes and cereals during the week. If you are prone to constipation, add a salad of grated boiled beets with vegetable oil, seaweed, prunes or figs daily. You can drink an infusion of ground flax seed (up to 1 tbsp two to three times a day).
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Advantages and disadvantages
| pros | Minuses |
|
|
Reviews and results
According to reviews, adherence to therapeutic nutrition gives good results. First of all, the wound surface is not irritated by hot spices and dishes; the introduction of boiled beets, bran and prunes into the diet promotes easy bowel movements.
Drinking plenty of fluids also contributes to this. This therapeutic diet is easy to implement and effective, so people with diseases of the rectum (hemorrhoids, anal fissure) should constantly adhere to it to prevent complications in the form of paraproctitis.
- “... I suffer from constipation, and this caused a crack. The pain was not very severe, and I did not pay attention to it. When the temperature rose, the pain intensified, and it became impossible to sit, then I turned to a proctologist. He ordered hospitalization and a day later they opened it up. After that, I began to really watch my diet. First of all, you need to avoid constipation, and secondly, spicy, fried, smoked, garlic, and pickled vegetables should be avoided, as these all irritate the wound. It was difficult for me to drink a lot of water and eat beets several times a day (I don't like them). But I had to do all this. Prunes, baked apples and pumpkin helped well - this was instead of dessert. So in two months everything healed completely, my stool returned to normal. Now I eat like this all the time, because I’m afraid that the crack will appear again.”
- “... We performed an autopsy six months ago. I stuck to a diet: nothing spicy or fried. She ate porridge and boiled meat, beets, prunes, and drank a lot of water. Everything has healed and I feel fine. But how much suffering during this time - baths, ointment bandages, constant suppositories. I realized that I need to monitor my diet all the time to avoid constipation. I noticed that bread, pasta and all flour products, potatoes and meat are fortified in large quantities. Therefore, I forever gave up pasta, dumplings, pancakes, bread, and pastries. I eat meat only at lunch and a small piece, beets every day. I lost a lot of weight on this diet.”
- “... My fistula was complex and plastic surgery was performed during the operation. I had to go through a lot, I mean dressings, wound care and nutrition to make the stool soft. I tinkered with all this for six months. Now I only left sea buckthorn suppositories and Bezornil ointment. I started watching my diet. I eat 3 tablespoons of flax seed during the day - I grind it, infuse it with hot water and eat this “slimy porridge”. Be sure to drink a lot of water, otherwise you will be constipated. At night I drink kefir with steamed prunes, and during the day I drink beet salad with seaweed. Of course, all this is boring, especially beets, but there is no other way out.”
Diagnosis of paraproctitis
Treatment begins with a consultation with a proctologist. The doctor examines the patient, conducts diagnostics, and prescribes tests necessary to clarify the nature and complexity of the disease. These include:
- Anoscopy is a procedure used to visually evaluate the anal canal.
- Sigmoidoscopy, which allows you to diagnose the condition of the mucous membrane.
- Colonoscopy showing the condition of both the rectum and colon.
In addition, sometimes the patient needs to undergo laboratory diagnostics - blood tests, stool tests, etc.
Upon completion of a comprehensive examination, the day of surgery is scheduled.