Nonspecific ulcerative colitis is a disease that demonstrates large-scale development in modern living conditions. In addition, the disease began to be detected more and more often in children, that is, it became noticeably “younger.” At first, ulcerative colitis is localized in the rectum, and over time, if left untreated, it spreads to the entire large intestine. People aged 20 to 40 are at increased risk, as evidenced by official statistics. Among older people, this disease is detected very rarely.
What is ulcerative colitis?
Ulcerative colitis falls under the category of inflammatory bowel diseases (IBD). The disease is chronic and often affects teenagers and young adults. The main symptoms are the appearance of pain in the abdomen, the inability to hold feces, diarrhea, and the appearance of blood clots in the stool. The inflammatory process originates in the rectum and during development spreads to the entire colon. In treatment, special drugs are used that regulate this inflammatory process.
There is another disease that, due to the similarity of symptoms, is often confused with ulcerative colitis - Crohn's disease. The main difference between illnesses is that they affect different parts of the body. If colitis is localized only in the colon, then Crohn's disease is localized in any part of the digestive tract.
Page 4 of 12
Diet therapy for vitamin deficiency in patients with inflammatory bowel diseases
Vitamin deficiency is more often observed in Crohn's disease, since in this disease, as a rule, the small intestine is affected, where absorption of nutrients occurs. For example, vitamin B12 is absorbed in the final part of the small intestine (the ileum). When this part of the intestine becomes inflamed or when it is removed (resection), vitamin B12 deficiency occurs, which is manifested by anemia and neurological symptoms. In the case of ulcerative colitis, vitamin B12 deficiency occurs more often due to reduced consumption of foods rich in this vitamin. In the presence of an inflammatory process in the small intestine, the absorption of both water-soluble (group B and C) and fat-soluble vitamins (A, D, E, K), that is, multivitamin deficiency develops.
Table 4 shows products that are sources of various vitamins.
Table 4. Vitamin content in 100 g of the edible portion of products
| Vitamins | Amount of vitamin per 100 g of product | Food products |
| 1 | 2 | 3 |
| Vitamin C | Very large (100 mg or more) Large (40-99 mg) Moderate (15-39 mg) | Fresh rosehip, red sweet pepper, black currant, sea buckthorn, green sweet pepper, parsley, Brussels sprouts, dill, wild garlic. Cauliflower, white and red cabbage, oranges, garden strawberries, horseradish, spinach, garlic (feather), lemons, kiwi, grapefruit, spinach, white currants. Tangerines, liver, rutabaga, green onions, green peas, tomatoes, radishes, potatoes, leeks, green onions, lettuce, zucchini, melon, gooseberries, chokeberries, cloudberries, dogwoods, raspberries, quince, lingonberries, cherries, cherries, apples, cranberries, red currants, pineapple, sauerkraut |
| Vitamin B1 | Very large (1 mg or more) Large (0.4-0.9 mg) Moderate (0.15-0.39 mg) | Pork tenderloin, piglet meat. Split peas, bacon pork, yeast, cereals (oatmeal, buckwheat, millet), beans. By-products, wholemeal bread, pork sausages, boiled sausages, green peas, veal bread, barley, rabbit meat, catfish, pink salmon, chum salmon, grenadier, horse mackerel, tuna, caviar (sturgeon, stellate sturgeon, pollock), pasta, bread . |
| Vitamin B2 | Very large (more than 0.4 mg) Large (0.2-0.4 mg) Moderate (0.1-0.19 mg) | Liver, kidneys, heart, yeast, almonds, cheeses, eggs, mushrooms, granular beluga caviar. Tongue, fat cottage cheese, bread, beef, goose, turkey, soybeans, rose hips, green beans, mushrooms, buckwheat, halva, sheep's milk, spinach, chum salmon, fatty herring, mackerel, tuna, Cow's milk, goat's milk, cream, kefir, butter, sour cream, green peas, Brussels sprouts, cauliflower, green sweet pepper, parsley, celery, dill, green onion, granular caviar (sturgeon, stellate sturgeon, pollock), flounder, pink salmon, grenadier , perch, halibut, sardine, pike, cod, hake, pork, chicken, rabbit meat, boiled sausages, oatmeal. |
| Vitamin PP | Very large (3 mg or more) Big (1.5-2.9 mg) Moderate (1.0-1.4 mg) | Peanuts, yeast, offal (liver, kidneys, tongue, etc.), tuna, herring, mackerel, sardines, sunflower seeds, fresh mushrooms, poultry, beef, lamb, almonds, buckwheat, wholemeal bread. Legumes, pork, boiled sausages, cod, sea bass, halibut, chum salmon, peas, beans, green peas, pearl barley, barley, rice, wheat bread made from 2 grades of flour, hazelnuts. Horse mackerel, hake, pike perch, pike, wheat bread made from premium flour, rice, millet, oatmeal, corn, semolina, pasta, carrots, walnuts, potatoes, red sweet peppers, garlic. |
| Folic acid | Very big (30 mcg or more) Large (20-29 mcg) Moderate (10-19 mcg) | Yeast, beef and pork liver, soybeans, parsley, beans, spinach, lettuce, leeks, low-fat cottage cheese, porcini mushrooms, millet, horseradish, wild garlic, beans, hard cheeses, buckwheat and barley cereals, Brussels sprouts. Cottage cheese, many cheeses, cereals (oatmeal, semolina, pearl barley), bread, pasta, green peas, dill, cauliflower and early white cabbage Egg yolk, cereals (rice, corn), herring, horse mackerel, hake, pike perch, eggplant, zucchini, onions, peas, pumpkin, rhubarb, late white cabbage, beets, strawberries, figs. |
| Vitamin A | Very large (3 mg or more) Large (0.4-2.9 mg) Moderate (0.1-0.3 mg) | Chicken liver, beef liver, canned cod liver, pork liver. Granular beluga caviar, egg yolk, butter. Cheese, sour cream, 20% fat cream, full-fat cottage cheese, kidneys, halibut, sprats (canned), sturgeon caviar, stellate sturgeon. |
| β-carotene | Very big (2 mg or more) Large (1-1.8 mg) Moderate (0.2-0.9 mg) | Carrots, parsley, celery, spinach, wild garlic, rose hips, red bell pepper, leek, onion, garlic (feather). Lettuce, apricots, pumpkin, ground tomatoes, sea buckthorn, sweet green pepper, dill, chokeberry, beef liver. Green peas, Brussels sprouts, greenhouse tomatoes, green beans, melon, peaches, raspberries, gooseberries, red currants, butter, yellow carrots, cheeses (cheddar, camembert). |
If diet cannot correct vitamin deficiency, they must be administered in the form of multivitamin complexes or by injection (intravenously or intramuscularly).
- Back
- Forward
Causes of the disease
With nonspecific ulcerative colitis, it is impossible to accurately determine the causes of its development, since this disease is characterized by an unclear etiology. However, based on many years of experience, experts were able to compile a list of the main factors in the development of ulcerative colitis:
- unfavorable environmental conditions (working or living in difficult environmental conditions);
- unbalanced diet - lack of vitamins and beneficial microelements leads to a weakened immune system in general;
- presence of bad habits (for example, smoking, alcohol abuse);
- taking medications for a long period of time;
- constant psychological stress.
Additionally, the following factors can cause the development of ulcerative colitis:
- a history of dysbacteriosis;
- hereditary predisposition;
- the occurrence of a viral or bacterial infection in the body;
- development of autoimmune processes, etc.
Taken together, these factors increase the risk of ulcerative colitis. It is worth noting that colitis is often diagnosed against the background of Crohn's disease.
Description of the drug PREDNIZOLON-FEREYN
Use with caution in case of parasitic and infectious diseases of a viral, fungal or bacterial nature (currently or recently suffered, including recent contact with a patient) - herpes simplex, herpes zoster (viremic phase), chickenpox, measles, amoebiasis, strongyloidiasis (established or suspected), systemic mycosis; active and latent tuberculosis. Use for severe infectious diseases is permissible only against the background of specific therapy.
Use with caution within 8 weeks before and 2 weeks after vaccination, with lymphadenitis after BCG vaccination, with immunodeficiency conditions (including AIDS or HIV infection).
Use with caution for gastrointestinal diseases:
- peptic ulcer of the stomach and duodenum, esophagitis, gastritis, acute or latent peptic ulcer, recently created intestinal anastomosis, ulcerative colitis with the threat of perforation or abscess formation, diverticulitis.
Use with caution for diseases of the cardiovascular system, incl. after a recent myocardial infarction (in patients with acute and subacute myocardial infarction, the necrotic focus may spread, slowing down the formation of scar tissue and, as a result, rupture of the heart muscle), with decompensated chronic heart failure, arterial hypertension, hyperlipidemia), with endocrine diseases - diabetes mellitus ( including impaired tolerance to carbohydrates), thyrotoxicosis, hypothyroidism, Itsenko-Cushing's disease, with severe chronic renal and/or liver failure, nephrourolithiasis, with hypoalbuminemia and conditions predisposing to its occurrence, with systemic osteoporosis, myasthenia gravis, acute psychosis , obesity (III-IV degree), with poliomyelitis (with the exception of the form of bulbar encephalitis), open- and closed-angle glaucoma.
If intra-articular administration is necessary, use with caution in patients with a general severe condition, ineffectiveness (or short duration) of the action of 2 previous administrations (taking into account the individual properties of the corticosteroids used).
During treatment (especially long-term), it is necessary to observe an ophthalmologist, monitor blood pressure and water-electrolyte balance, as well as pictures of peripheral blood and blood glucose; In order to reduce side effects, you can prescribe anabolic steroids, antibiotics, and also increase the intake of potassium in the body (diet, potassium supplements). It is recommended to clarify the need for ACTH administration after a course of treatment with prednisone (after performing a skin test!).
In Addison's disease, concomitant use with barbiturates should be avoided.
After stopping treatment, withdrawal syndrome, adrenal insufficiency, and exacerbation of the disease for which prednisolone was prescribed may occur.
For intercurrent infections, septic conditions and tuberculosis, simultaneous antibiotic therapy is necessary.
In children during the growth period, GCS should be used only for absolute indications and under the close supervision of a physician.
It should not be used externally for more than 14 days. If used for acne vulgaris or rosacea, an exacerbation of the disease is possible.
Who is at risk?
According to statistics, approximately 0.6% of the total population of the Russian Federation is diagnosed with IBD. It is also known that these values are increasing, that is, every year an increasing number of diseases are recorded.
Main features of the development of ulcerative colitis:
- Both men and women are equally susceptible to the disease (the disease is not gender specific);
- Every year approximately 30 thousand cases of Crohn's disease and ulcerative colitis are recorded;
- men aged 50 to 60 years are more susceptible to the disease than women at this age;
- The average age of people who develop ulcerative colitis ranges from 15 to 25 years;
- According to statistics, Europeans are more likely to suffer from ulcerative colitis than representatives of other races;
- Most often people living in highly developed countries and large cities get sick.
Research shows that ulcerative colitis is a disease that can be inherited from relatives. The risks of developing the disease are quite high and amount to 5.2–22.5%. At the same time, many questions remain about the disease and the characteristics of its spread.
Classification and stages of development
The disease is characterized by certain symptoms that vary with different levels of inflammation and location in the colon. To act correctly, you must first determine the location of the lesion.
Ulcerative colitis can take the following forms:
- Ulcerative proctitis. The development of the disease begins directly in the rectum. The lesion most often affects no more than 15 cm of the organ, and for this reason this form of the disease is considered the most benign. Among the main symptoms, it is necessary to highlight the release of blood drops or clots from the rectum, pain in the rectal area, and the inability to hold feces.
- Left-sided colitis. The inflammation affects the rectum and moves to the splenic flexure, which is located in the upper abdomen. The inflammatory process continues for quite a long time. Among the main symptoms, it is necessary to highlight lack of appetite, bleeding from the anus, weight loss, pain in the left side of the abdomen, which manifests itself quite strongly.
- Pancolitis. With this form of total ulcerative colitis, the entire colon is affected. Among the main symptoms, it is necessary to highlight lack of appetite, diarrhea with severe bleeding, pain in the abdomen, which is quite severe, and weight loss.
Scheme of drug therapy for nonspecific ulcerative colitis in children
Nonspecific ulcerative colitis (UC) is a chronic inflammatory bowel disease, the etiology of which remains unknown to date. The frequency of nonspecific ulcerative colitis, according to foreign researchers, is 4–10 per 100 thousand children [1]. Difficulties in selecting therapy for UC are associated with a lack of knowledge about the etiology and some parts of the pathogenesis of the disease [2].
In choosing the most optimal treatment regimen for nonspecific ulcerative colitis, first of all, determining the degree of activity of the inflammatory process and its localization helps. According to the literature, with nonspecific ulcerative colitis, the inflammatory process in 54% of cases is localized in the rectum and sigmoid colon, in 28% of cases there is left-sided damage to the colon, and in 18% of patients pancolitis occurs. In young children (up to three years of age), the right-sided parts of the colon are predominantly affected [3].
The degree of activity of nonspecific ulcerative colitis is determined based on the severity of clinical and laboratory parameters. The most pronounced clinical indicators are: diarrhea, blood in the stool, intensity of abdominal pain, weight loss and fever. Laboratory indicators of nonspecific ulcerative colitis include changes in hemoglobin and albumin levels, and an increase in ESR. Currently, there are three degrees of activity of ulcerative colitis: mild, moderate and high (see Table 1) [4, 5].
Among the main directions in the treatment of nonspecific ulcerative colitis, nutrition correction and diet therapy should be mentioned. The principles of rational nutrition include avoiding fried, fatty, salty, spicy foods, milk and dairy products.
A sick child’s diet should also not include chocolate, legumes, mushrooms, fruits and vegetables that stimulate peristalsis (plums, kiwi, dried apricots, beets). During periods of exacerbation, the consumption of fiber, sweets, and juices is limited [6]. With long-term remission, the diet can be significantly expanded, but milk and dairy products are contraindicated for the patient throughout his life [7].
Drug therapy as the main method of treating ulcerative colitis involves the use of:
- preparations of 5-aminosalicylic acid (5-ASA);
- corticosteroids;
- immunosuppressants (cytostatics).
Symptomatic and antibacterial therapy is prescribed to restore the structure of the mucous membrane, normalize peristalsis, restore digestive processes and eubiosis of the colon, and increase the overall immunoreactivity of the body. If diet therapy and drug therapy are ineffective, surgical treatment is indicated.
5-ASA drugs are basic in the treatment of ulcerative colitis. In 1942, the drug sulfasalazine was first used in patients with combined damage to the intestines and large joints, which gave a pronounced positive effect: arthralgia and hemocolitis were relieved [8]. Sulfasalazine has been used in the treatment of ulcerative colitis to this day. However, its use is limited due to a large number of side effects, such as hemolytic anemia, neutropenia, drug-induced hepatitis, Steven-Johnson syndrome, pericarditis, interstitial nephritis, pancreatitis. The frequency of side effects, according to different authors, ranges from 5 to 55% [9]. Sulfasalazine contains mesalazine (5-aminosalicylic acid), which has an anti-inflammatory effect, and sulfapyridine, which ensures the delivery of mesalazine to the colon,
to the site of localization of the main inflammatory process in nonspecific ulcerative colitis. Sulfapyridine contributes to the development of a large number of side effects [10]. Numerous studies conducted to develop drugs containing mesalazine made it possible in the late 70s and early 80s. create drugs that did not contain sulfapyridine. This has led to a significant reduction in side effects, which in turn has made it possible to use higher doses of mesalazine and, in some cases, eliminate the use of corticosteroids. Mesalazine is active upon local contact with the intestinal mucosa, and its therapeutic efficacy is correlated with the concentration in the intestinal lumen. These features of mesalazine made it possible to develop drugs based on it and successfully use them both in the acute period and for the purpose of local maintenance therapy, such as suppositories and microenemas [11].
Table 2 presents some of the 5-ASA drugs [12], which can be divided into three groups. The first group includes sulfasalazine and olsalazine, which are released under the influence of intestinal flora and act in the colon. The second group includes mesacol, salofalk, rovaza. The release of these drugs depends on the pH of the environment, and their action is localized in the terminal ileum and colon. The third group includes the drug Pentasa, which is released slowly and acts throughout the intestine.
The mechanism of action of 5-ASA is based on an anti-inflammatory effect, which is realized through inhibition of prostaglandin formation, reduction in the synthesis of cytokines IL-1, IL-2, IL-6, tumor necrosis factor, inhibition of the lipoxygenase pathway of arachidonic acid metabolism, and reduction in the production of free radicals [13, 14, 15].
Indications for the use of 5-ASA drugs.
- Primary therapy for mild UC activity.
- Primary therapy in combination with steroids for moderate to highly active UC.
- Maintenance therapy for UC.
In our country, the most commonly used 5-ASA drugs are sulfasalazine, salofalk and pentasa. As noted earlier, sulfasalazine has been used in the treatment of ulcerative colitis for 60 years. The breakdown of sulfasalazine into mesalazine and sulfapyridine depends on the composition of the intestinal flora and occurs only in the colon [16]. When inflammation is localized in the cecum and ascending colon (in young children), the effectiveness of sulfasalazine is significantly reduced.
Salofalk - the active ingredient in this drug is mesalazine. The drug is a tablet coated that is resistant to gastric juice. Its feature is the absence of a sulfonic component, which reduces the number of side effects. Activation of salofalk occurs when the acidity of the environment changes (over 6). The site of action of salofalk is predominantly the terminal ileum and colon [17].
The drug Pentasa appeared on the Russian market relatively recently. The active ingredient is also mesalazine, enclosed in microgranules that are resistant to the acidic environment of the stomach. Pentasa is released slowly, gradually, along the intestine, starting from the duodenum. At the same time, changes in the level of intraluminal pH and acceleration of transit during diarrhea do not affect the rate of drug release. Thanks to these features, Pentasa provides high therapeutic concentrations throughout the small and large intestines [18, 19].
When treating nonspecific ulcerative colitis, doses of 5-ASA drugs are selected individually. Typically, the dose of sulfasalazine is 50–60 mg/kg/day; the maximum daily dose at which no side effects are observed is up to 6 g/day [20]. The dosage of mesalazine ranges from 20 to 50 mg/kg/day, the maximum daily dose is 4 g/day. At these dosages, the drug can be used from one to three months [21]. Salofalk and Pentasa are used for local therapy in suppositories and microenemas: suppositories - 250-500 mg once or twice a day, microenemas - 2-4 mg once a day. Local therapy is carried out for 14–28 days; if necessary, repeated courses of local therapy can be prescribed. Maintenance doses of 5-ASA for nonspecific ulcerative colitis are half the therapeutic dose: sulfasalazine - 20 mg/kg/day, mesalazine - 10 mg/kg/day. Maintenance therapy is prescribed for a long time, from six months to two years, in the absence of an active inflammatory process [22].
Side effects when using mesalazine are quite rare (1–3%) [23]. In this case, abdominal pain, diarrhea, flatulence, nausea, vomiting, and pancreatitis are noted. Allergic reactions occur in the form of skin itching and allergic rash. Bronchospasm, pericarditis, myocarditis, and interstitial nephritis are extremely rare; their frequency, according to the literature, is 0.1-0.5% [24]. To prevent side effects, it is not recommended to exceed the maximum permissible therapeutic doses of drugs; the condition of peripheral blood should be monitored (complete blood count once every two weeks). Repeated biochemical blood tests are also necessary, including determination of the level of total protein, protein fractions, urea, creatinine, transaminases, alkaline phosphatase, electrolytes, and serum iron.
In addition to 5-ASA drugs, corticosteroids are used in the treatment of ulcerative colitis. The most commonly used are prednisolone, methylprednisolone, and hydrocortisone. The mechanism of action of corticosteroids is based on the anti-inflammatory effect, reducing the formation of prostaglandins, inhibiting the formation and action of cytokines IL-1, IL-2, IL-3, tumor necrosis factor and stabilization of lysosomal membranes [25]. Indications for the use of corticosteroids in nonspecific ulcerative colitis are the lack of effect of mesalazine therapy for mild UC activity (in combination with mesalazine), primary therapy for moderate and high UC activity. Corticosteroid treatment is often complicated by multiple side effects, the most common of which are hypothalamic-pituitary axis suppression, Cushing's syndrome, hypertension, osteoporosis, peptic ulcers, electrolyte disturbances, and steroid-induced diabetes [26]. Side effects are dose-dependent and increase with increasing duration of hormonal therapy. To prevent them, it is necessary to monitor the state of peripheral blood, biochemical parameters, and electrolyte state of the blood.
Doses of glucocorticoids in the treatment of nonspecific ulcerative colitis for oral and/or parenteral administration are: when prescribing prednisolone - 1-2 mg/kg/day, methylprednisolone - 25-30 mg/day. For local therapy, it is possible to use prednisolone in suppositories 20-40 mg 1 time per day and/or in microenemas 20 mg per 60-100 ml of liquid 1 time per day. Hydrocortisone is usually used only for local therapy in microenemas 100 mg per 60–100 ml of water once a day. The duration of therapy for oral administration is 2-3 weeks, then it is necessary to gradually reduce the dosage of the drugs by 10 mg per week to a level of 0.75 mg/kg/day. Further reduction is carried out by 5 mg per week until the drug is completely discontinued. In this case, the dose of 5-ASA should not be lower than 1/2 of the therapeutic dose [27].
Hormonal therapy can lead to the development of hormonal dependence, in which the positive effect is either absent or replaced by reactivation of the inflammatory process due to dose reduction or withdrawal of corticosteroid therapy [28]. There are two forms of hormonal dependence of ulcerative colitis (in relation to steroids): a hormone-resistant form, which is primary, and a hormone-dependent form, which is often secondary. In this case, sensitivity to 5-ASA drugs may remain or be absent [29]. To overcome hormonal dependence, increased doses of glucocorticoids and pulse therapy are used; if these measures are ineffective, immunosuppressive therapy is indicated [19].
Immunosuppressants used in the treatment of ulcerative colitis include azathioprine, 6-mercaptopurine, methotrexate, and cyclosporine. The mechanism of action of these drugs is different. Azathioprine and 6-mercaptopurine affect natural killer cells [30], methotrexate disrupts the synthesis of RNA and DNA of cells [31], cyclosporine inhibits the production of cytotoxic lymphocytes and inhibits interleukins IL-2, as well as their receptors [32].
Indications for the use of immunosuppressants for nonspecific ulcerative colitis are hormone-resistant and hormone-dependent forms.
Doses of immunosuppressants in the treatment of ulcerative colitis, according to different authors, vary greatly. Typically, azathioprine is prescribed at a dose of 1-2 mg/kg/day, 6-mercaptopurine at a dose of 1.5 mg/kg/day. The dosage regimen is set individually. The effect of therapy with these drugs is observed after 3 months. Methotrexate is used at a dose of 2.5 mg/day; the therapeutic effect of methotrexate occurs much earlier than that of azathioprine: after 3-4 weeks. Cyclosporine is usually used in a short course to interrupt the activity of the process, followed by a transition to long-acting immunosuppressants [33].
The toxic effects that occur with the use of antidepressants are very diverse. These include anorexia, nausea, vomiting, suppression of hematopoiesis, skin rash, arthralgia, myalgia, pancreatitis, toxic hepatitis, cholestasis syndrome, opportunistic infections, lymphadenopathy, arterial hypertension, toxic kidney damage, parasthesia, tremor. The severity of side effects of immunosuppressants limits their use in the treatment of ulcerative colitis [34]. To prevent side effects, it is necessary to monitor the functions of hematopoiesis, liver, and kidneys. General blood test, general urine test, biochemical blood test, including determination of the level of total protein, protein fractions, liver enzymes, alkaline phosphatase, urea, creatinine, glucose, acute phase proteins - all these studies must be carried out once a week.
Symptomatic therapy for nonspecific ulcerative colitis is indicated for any degree of activity of the inflammatory process. In each special case it is selected individually. Enzyme preparations (Creon, Mezim-Forte) are often prescribed in the presence of malabsorption syndrome and to relieve the load on the pancreas. Choleretic drugs and hepatoprotectors are used if the patient has cholestasis syndrome and toxic hepatitis. To correct vitamin and metabolite deficiency and iron deficiency anemia, multivitamins, iron preparations (for parenteral administration), and a metabolite complex are used. It is advisable to include herbal medicine (galangal, chamomile, burnet, licorice) in the complex of therapeutic effects. Antibacterial therapy is prescribed in the presence of secondary infections, septic complications, and perianal inflammation. Antibiotics, nitrofuran drugs, metronidazole (Trichopol) are used [27].
The treatment regimen for nonspecific ulcerative colitis, developed by the European Association of Pediatric Gastroenterologists, Hepatologists and Nutritionologists (ESPGHAN) and used in the Department of Gastroenterology and Hepatology of the Scientific Center for Disease Control and Prevention of the Russian Academy of Medical Sciences, is based on various degrees of activity and localization of the inflammatory process. For isolated proctitis, the main treatment method is local therapy in the form of suppositories and/or microenemas. With a mild degree of activity, you can limit yourself to using only mesalazine drugs (salofalk, pentasy). Changes in intestinal flora make treatment with sulfasalazine suppositories ineffective. The treatment regimen for nonspecific ulcerative colitis with proctitis is presented in Table 3.
For proctosigmoiditis of moderate and high activity, in addition to local therapy, oral administration of mesalazine or prednisolone in age-specific dosages is indicated. The treatment regimen for proctosigmoiditis is given in Table. 4.
Pancolitis, or total intestinal damage, usually has a moderate or high degree of activity. In the treatment of pancolitis, mesalazine or sulfasalazine orally and prednisolone in large doses orally or parenterally are used; in the presence of rectal damage, local therapy is indicated (see tables 3 and 4). The treatment regimen for pancolitis in nonspecific ulcerative colitis is presented in Table 5. Doses of 5-ASA drugs are given for children over 12 years of age. For children under 12 years of age, the dosage of drugs is calculated based on body weight: sulfasalazine - 60 mg/kg/day, mesalazine - 30-40 mg/kg/day.
The tactics for monitoring children with nonspecific ulcerative colitis in the active stage include conducting control blood tests to determine the level of hemoglobin, ESR, leukocytes, total protein and protein fractions once a week during the active stage and once a month during remission. Colonoscopy and morphological examination are carried out 3 months after the appointment of therapy during exacerbation of the disease, once every 2-3 years - during remission, once a year - when the disease history is more than 8-10 years. Children with inflammatory bowel diseases require long-term medical supervision. In the presence of remission in spring and autumn, preventive courses of 5-ASA drugs in maintenance doses for 3 months are indicated [7].
Thus, treatment of nonspecific ulcerative colitis is based on determining the localization of the inflammatory process and the degree of its activity. With a mild degree of activity, the prescription of mesalazine is indicated; moderate and high degrees of activity require the appointment of corticosteroid therapy. If there is no effect from therapy with 5-ASA drugs and steroids and the development of hormonal dependence, immunosuppressive therapy is used. If drug therapy is ineffective, surgical treatment is indicated.
Literature
- Diseases of the digestive system in children (small and large intestines) / Ed. A. A. Baranova, E. V. Klimanskaya. M., 1999. pp. 240-250.
- Shcherbakov P. L. Inflammatory bowel diseases in children: Crohn's disease and ulcerative colitis / Children's doctor. 2000. No. 4. P. 22-26.
- Beattie RM and others, Endoscopic assessment of colonic response to corticosteroids in children with ulcerative colitis/ /J Pediatr Gastroenterol Nutr. 1996. No. 22. P. 373-379.
- Truelove SC, Witts LJ Cortisone in ulcerative colitis: final report on therapeutic trial//Br Med J. 1987. No. 295. P. 517-519.
- Griffiths AM, Buller HB Inflammatopy Bowel Disease. 613-653
- Surikova O. A. Nonspecific ulcerative colitis in children // Children's doctor. 2000. No. 1. P. 45-49.
- Kanshina O. A. Experience in the treatment of nonspecific ulcerative colitis in children and adolescents // Pediatrics. 1992 No. 1. P. 78-82.
- Barden M.E., Lipson A., Pert P., Walker-Smith JA Mesalasin in childhood inflammatopy bowel disease//Aliment Pharmacol Ther. 1989. No. 3. P. 597-603.
- Tolia V., Massoud N., Klotz U. Oral 5-aminosalycilic acid in children with colonic chromic inflammatopy bowel disease: clinical and pharmacokinetic experience//Aliment Pharmacol Ther. No. 6. P. 1012-1014.
- Khalif I. L. The use of salicylates in the treatment of nonspecific ulcerative colitis / Attending Physician. 2000. No. 5-6. P. 52.
- Loginov A. S., Parfenov A. I. Intestinal diseases. M., 2000. P. 32.
- Paykov V. L. Pharmacotherapy in pediatric gastroenterology. St. Petersburg, 1998. pp. 188-189.
- Laursen Ls and others: Disposition of 5-aminosalicylic acid by olsalasin and three mesalasin preparation in patients with ulcerative colitis//Gut, 1990. No. 31. P. 1271-1276.
- Rijk MCM and others: Disposition of 5-aminosalicylic acid delivering drugs during accelerated untestinal transit in healthy volunteers // Scand J Gastroenterol, 1989. No. 24. P. 1179-1185.
- Colllins JR Adverse reaction to salicylasosulfapyridine in the treatment of ulcerative colitis//South Med J. 1968. No. 61. P. 354-358.
- Loginov A. S., Parfenov A. I., Ruchkina I. N., Krums L. M. The use of salosinal in the treatment of inflammatory diseases of the colon.
- Courtney MG and others Randomized comparison of olsalazin in prevention of relapses in ulcerative colitis//Lancet. 1992. No. 339. P. 1079-1281.
- Hardy JG, Harvey WJ, Sparrow RA et al. Localization of drug release sites from an oral sustained formulation of 5-ASA (Pentasa(r)) in the gastrointestinal tract using gamma scintigraphy//J Clin Pharmacol. 1993. No. 3. P. 712-718.
- Stein RB, Hanauer SB Medical therapy for inflammatopy bowel disease//Gastroenterol Clin North Am. 1999. No. 28. P. 297-321.
- Azad Khan AK and others. Optimun dose of sulphasalasine for maintenance treatment in ulcerative colitis//Gut. 1980. No. 21. P. 232-240.
- Baron JH, Connell AM, Lennard-Jones JE Sulphasalasine and salicylasosulfapyridine in ulcerative colitis/ Lancet. 1962. P. 1094-1096.
- Hanacur SB Inflammatopy bowel disease // N Engl J Med. 1996. No. 334. P. 841-848.
- Sutherland LR, May GR, Shaffer EA Sulphasalasine revisited: a meta-analysis of 5-aminosalicylic acid in the treatment of ulcerative colitis//Ann Inten Ned. 1993. No. 118. P. 540-549.
- Zlatkina A. R. Treatment of chronic diseases of the digestive system. M., 1994. pp. 163-217.
- Belaiehe J., Louis E. Corticosteroids treatment in active Crohn's disease//Asta Gastroenteerol Belg. 1998. No. 61(2). P. 153-157.
- Kusunoki M. and others. Steroid complications in patients with ulcerative colitis//Dis Colon Rectum. 1992. No. 35. P. 1003-1009.
- Alieva E. I., Khalif I. L., Mazankova L. N. Conservative treatment of nonspecific ulcerative colitis in children // Children's doctor. 2001. No. 2. P. 36-42.
- Kopeikin V.N. Mechanisms of formation and optimization system for the treatment of nonspecific ulcerative colitis in children: Abstract of thesis. dis. ... doc. honey. Sciences, M., 1996.
- Compston JE Corticosteroids and growth//J Pediatr. 1998. No. 113. P. 249-254.
- Verhave M., Winter HS, Grand RJ Azathioprine in treatment of inflammatopy bowel disease//J Pediatr. 1998. No. 117. pp. 809-814.
- Egan LJ, Sandorn WJ Metotrexate for inflammatopy bowel disease//Mayo Clin Proc. 1996. No. 71. P. 69-80.
- Treem WR and others. Cyclosporine for the treatment of fulminant ulcerative colitis in children//Dis Colon Rectum. 1995. No. 38. P. 474-479.
- Aranda R., Horgan K. Immunosuppressive drugs in the treatment of inflammatopy bowel disease//Semin Gastrointest Dis. 1998. No. 9. P. 29.
E. G. Tsimbalova, Candidate of Medical Sciences A. S. Potapov P. L. Shcherbakov, Doctor of Medical Sciences SCCD RAMS, Moscow
Can ulcerative colitis be cured?
It is immediately worth noting that ulcerative colitis is a chronic disease and it is incurable. Each case of the disease is individual, and it is impossible to 100% accurately predict its further behavior. For some patients, the disease is asymptomatic for several years, for others it is characterized by frequent exacerbations and outbreaks of development.
According to statistics, the disease does not affect human life expectancy. In addition, with ulcerative colitis you can achieve long-term remission and live a full, happy life.
Causes of development of nonspecific ulcerative colitis
Many factors play a role in the development of ulcerative colitis, but the exact causes of the disease have not yet been established. Taken together, genetic, infectious, environmental, and immunological factors cause intestinal malfunction and the development of autoimmune inflammation in the mucosal and submucosal layer of the intestinal wall. If the disease is not treated, it gradually progresses with the formation of inflammatory ulcers in the direction from the rectum to the overlying sections.
At the appointment, the gastroenterologist at our hospital finds out in detail from the patient the peculiarities of life and work, the nature and duration of the development of the disease. This is necessary to clarify the initiating factors that provoke the disease and its exacerbation and the possibility of eliminating them.
Etiology and pathogenesis
The development of the disease can begin under the complex influence of several factors (for example, genetic predisposition, intestinal microflora, immune disorders, negative environmental influences, etc.). It is worth noting that approximately hundreds of single nucleotide polymorphisms are associated with ulcerative colitis. Accordingly, this phenomenon increases the risks of the innate immune response, as well as the processes of recognition of microorganisms, functions of the epithelial barrier, etc.
Impaired recognition of bacterial molecular markers by dendritic cells is the main pathology of the immune system, which more often provides hyperactivation of pro-inflammatory signaling pathways. If a person with such a history additionally eats poorly, abuses alcohol and smokes, then he significantly increases the risk of developing ulcerative colitis.
Symptoms of Ulcerative Colitis
When the mucous membrane of the rectum becomes covered with an increasing number of inflammations and ulcers, it ceases to function normally - in particular, it loses the ability to efficiently absorb fluid from waste products. As a result, the stool becomes liquid, which contributes to the formation of diarrhea. Also, mucus may appear in the stool - a sure sign that the rectal mucosa is not working well. When stool passes through the rectum, it affects the ulcers, and blood is released from them. This causes bleeding, which makes the stool bloody. This negatively affects a person’s condition, as blood loss occurs, which can result in anemia, which has negative consequences for the body.
Patients with ulcerative colitis often complain of pain in the left side of the abdomen, but it can spread throughout the entire abdominal cavity. Due to severe pain, a person loses appetite, which leads to weight loss. In combination with anemia, increased fatigue develops. The patient constantly experiences weakness and fatigue, and is in a sleepy state. If such phenomena occur in children, then the process of growth and development may additionally be disrupted.
Symptoms outside the bowel include the following:
- the appearance of pain, itching in the eyes, their redness;
- inflammatory processes in the oral cavity;
- formation of swelling and pain in the joints;
- development of osteoporosis;
- the appearance of soft bumps, inflammation, ulcers and rashes on the skin;
- development of hepatitis, cirrhosis;
- the appearance of kidney stones, etc.
It is noteworthy that many symptoms outside the gut can appear in people long before they appear in the gut itself.
Approximately 50% of patients diagnosed with ulcerative colitis have mild symptoms. But strong manifestations of the disease, which are most often short-lived and unstable, are not excluded.
Prednisolone
Since complications of therapy with Prednisolone depend on the dose and duration of treatment, in each specific case, based on an analysis of the risk/benefit ratio, a decision is made on the need for such treatment, and the duration of treatment and frequency of administration are determined.
The lowest dose of Prednisolone that provides a sufficient therapeutic effect should be used; if necessary, the dose should be reduced gradually.
Due to the risk of developing arrhythmia, the use of Prednisolone in high doses should be carried out in a hospital environment equipped with the necessary equipment (electrocardiograph, defibrillator).
If prolonged spontaneous remission occurs, treatment should be discontinued.
During long-term treatment, the patient should undergo regular examination (chest x-ray, plasma glucose concentration 2 hours after meals, urinalysis, blood pressure, body weight control, preferably an x-ray or endoscopic examination if there is a history of gastrointestinal ulcers). intestinal tract).
The growth and development of children on long-term therapy with Prednisolone should be carefully monitored. Growth retardation may occur in children receiving long-term, daily, multi-dose therapy. Daily use of prednisolone for a long time in children is possible only for absolute indications. Taking the drug every other day may reduce the risk of developing this side effect or avoid it altogether.
Children receiving long-term therapy with Prednisolone are at increased risk of developing intracranial hypertension.
Patients receiving drugs that suppress the immune system are more susceptible to infections. For example, chickenpox, genus, and measles can be more severe and even fatal in unimmunized children or in adults receiving Prednisolone.
Prednisolone should also be prescribed with great caution to patients with confirmed or suspected parasitic infections, such as strongyloidiasis. Prednisolone-induced immunosuppression in such patients leads to strongyloid hyperinfection and dissemination of the process with widespread migration of larvae, often with the development of severe forms of enterocolitis and gram-negative septicemia with possible death.
During prednisolone therapy, susceptibility to infections may increase, some infections may occur in an erased form, and new infections may develop. In addition, the body’s ability to localize the infectious process is reduced. The development of infections caused by various pathogenic organisms, such as viruses, bacteria, fungi, protozoa or helminths, which are localized in various systems of the human body, may be associated with the use of the drug Prednisolone, both as monotherapy and in combination with other immunosuppressants that affect on cellular immunity, humoral immunity or neutrophil function. These infections may not be severe, but in some cases they can be severe and even fatal. Moreover, the higher doses of the drug are used, the higher the likelihood of developing infectious complications.
In patients receiving treatment with Prednisolone in doses that have an immunosuppressive effect, the administration of live or live attenuated vaccines is contraindicated, but killed or inactivated vaccines can be administered, however, the response to the administration of such vaccines may be reduced or even absent. Patients receiving treatment with Prednisolone in doses that do not have an immunosuppressive effect may be immunized according to appropriate indications.
The use of Prednisolone in active tuberculosis should be limited to cases of fulminant and disseminated tuberculosis, when Prednisolone is used to treat the disease in combination with appropriate anti-tuberculosis chemotherapy. If the drug Prednisolone is prescribed to patients with latent tuberculosis or with positive tuberculin tests, then treatment should be carried out under strict medical supervision, since reactivation of the disease is possible. During long-term drug therapy, such patients should receive appropriate preventive treatment.
There have been cases of the development of Kaposi's sarcoma in patients receiving GCS therapy. When the drug is discontinued, clinical remission may occur.
When using the drug Prednisolone in therapeutic doses for a long period, suppression of the hypothalamic-pituitary-adrenal system (secondary adrenal insufficiency) may develop. The degree and duration of adrenal insufficiency is individual for each patient and depends on the dose, frequency of use, time of administration and duration of therapy.
The severity of this effect can be reduced by using the drug every other day or by gradually reducing the dose. This type of relative adrenal insufficiency can continue for several months after the end of treatment, so in case of any stressful situations during this period, Prednisolone should be re-prescribed. If the drug is abruptly discontinued, acute adrenal insufficiency may develop, leading to death.
GCS withdrawal syndrome (not related to adrenal insufficiency) can also occur due to abrupt drug withdrawal. This syndrome includes symptoms such as anorexia, nausea, vomiting, lethargy, headache, fever, joint pain, skin peeling, myalgia, weight loss and low blood pressure. It is assumed that these effects occur due to sharp fluctuations in the concentration of prednisolone in the blood plasma, and not due to its decrease.
Patients with hypothyroidism or cirrhosis have a more pronounced effect of prednisolone.
Since the secretion of mineralocorticosteroids may be impaired, concomitant administration of electrolytes or mineralocorticosteroids is necessary.
Moderate to large doses of hydrocortisone or cortisone may cause increased blood pressure, sodium and water retention, and increased potassium excretion. These effects are less likely with the use of synthetic corticosteroids (including prednisolone), except when they are used in high doses. It is necessary to limit the consumption of table salt with food and prescribe potassium supplements. All corticosteroids increase calcium excretion.
The use of Prednisolone may lead to an increase in the concentration of glucose in the blood plasma and a worsening of existing diabetes mellitus. Patients receiving long-term therapy with Prednisolone may be predisposed to developing diabetes mellitus.
For patients who may be exposed to stress during treatment with Prednisolone, an increase in the dose of the drug is indicated before, during and after a stressful situation.
During therapy with Prednisolone, the development of various mental disorders is possible: from euphoria, insomnia, mood swings and depression to acute mental manifestations. In addition, existing emotional instability or psychotic tendencies may be exacerbated.
Potentially severe mental disorders may occur when using Prednisolone. Symptoms usually appear within a few days to weeks after starting therapy. Most reactions disappear either after reducing the dose or after discontinuation of the drug. Despite this, specific treatment may be required. Patients and/or their relatives should be warned that if changes occur in the patient's psychological status (especially with the development of depression and suicidal attempts), they should seek medical help. Patients or their relatives should also be warned about the possibility of developing mental disorders during or immediately after reducing the dose of the drug or completely stopping it.
There are reports of the development of epidural lipomatosis in patients receiving GCS. Usually with long-term therapy at high doses.
Long-term use of the drug Prednisolone can lead to the occurrence of posterior subcapsular cataracts, exophthalmos or glaucoma with possible damage to the optic nerve and provoke the addition of a secondary ocular fungal or viral infection.
Due to the existing risk of corneal perforation, GCS should be prescribed with caution when treating eye infections caused by the herpes simplex virus (ophthalmoherpes).
Prednisolone therapy can lead to the development of central serous chorioretinopathy, which in turn can lead to retinal detachment.
Therapy with Prednisolone may mask the symptoms of a peptic ulcer, in which case perforation or bleeding may develop without significant pain.
Prednisolone should be used with caution in patients with risk factors for cardiovascular diseases, including hyperlipidemia and patients predisposed to high blood pressure, since taking Prednisolone may provoke new reactions when using high doses of the drug and long-term treatment. Regular monitoring of heart function is necessary. Using low doses of Prednisolone every other day may reduce the severity of these reactions.
Careful monitoring of patients receiving systemic corticosteroids and those who have recently suffered a myocardial infarction is necessary.
Patients taking Prednisolone should be prescribed acetylsalicylic acid-based analgesics and non-steroidal anti-inflammatory drugs with caution.
Allergic reactions are possible. Due to the fact that phenomena such as skin irritation and anaphylactic or pseudoanaphylactic reactions have rarely been observed in patients receiving GCS, the necessary measures should be taken before prescribing GCS, especially if the patient has a history of allergic reactions to drugs.
High doses of corticosteroids can cause acute pancreatitis.
Therapy with high doses of GCS can cause acute myopathy; In this case, the disease is most susceptible to patients with disorders of neuromuscular transmission (for example, myasthenia gravis), as well as patients receiving concomitant therapy with quinolytics, for example, blockers of neuromuscular transmission. This kind of myopathy is generalized; it can affect the muscles of the eyes or respiratory system and even lead to paralysis of all limbs. In addition, creatine kinase levels may increase. In such cases, clinical recovery may take weeks or even years.
Osteoporosis is a common (but rarely detected) complication of long-term therapy with high doses of corticosteroids.
GCS are prescribed with caution for long-term therapy in elderly patients due to the increased risk of osteoporosis and fluid retention in the body, which potentially causes an increase in blood pressure.
Concomitant treatment with methylprednisolone and fgorquinolones increases the risk of tendon rupture, especially in elderly patients.
Since prednisolone can enhance the clinical manifestations of Itsenko-Cushing syndrome. Prednisolone should be avoided in patients with this disease. Careful monitoring of patients with a history or current history of thrombosis or thromboembolic complications is necessary.
Diagnostics
It is impossible to name an exact list of diagnostic procedures that must be performed for ulcerative colitis as a standard. This is explained by the fact that the disease occurs individually in each case and it is quite difficult to predict its further development.
The doctor focuses on many factors when determining diagnostic methods: the results of a physical examination, anamnesis, clinical picture, complaints, etc.
Diagnostics can be represented by the following types of studies:
- serodiagnosis;
- stool analysis (general);
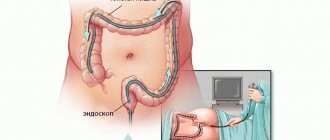
- colonoscopy – during the procedure, a specialist examines the intestinal mucosa and performs a biopsy;
- determination of the level of fecal calprotectin - necessary to determine the severity of inflammation;
- analysis of inflammatory factors;
- stool analysis for the presence of clostridia toxins A, B;
- blood test (general) - to determine the presence or absence of anemia;
- CT or MRI;
- X-ray with contrast – necessary for severe symptoms.
Additionally, an ultrasound examination of the abdominal organs may be required. As you can see, in order to diagnose and prescribe the most effective treatment, it is necessary to undergo a fairly large-scale study.
Diagnosis of nonspecific ulcerative colitis
Diagnosis begins with an examination of the patient, identification of complaints and medical history, a detailed interview with the patient, including, in particular, collection of information about trips to southern countries, intolerance to any foods, medications taken (in particular, antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs)), smoking and the presence of inflammatory and malignant bowel diseases in relatives. Laboratory diagnostic methods
- Complete blood count, hematocrit, erythrocyte sedimentation rate (ESR), C-reactive protein, hemocoagulogram, total protein, albumin, liver tests, electrolytes. In the acute course of UC (the first attack of the disease), it is necessary to perform a bacteriological and microscopic examination of stool to exclude acute intestinal infection. Both at the onset of the disease and during exacerbations, a study of C. difficile toxins A and B is recommended.
- Changes in laboratory parameters in UC are usually nonspecific. Anemia, leukocytosis, and electrolyte changes in the blood may occur.
Instrumental diagnostic methods
- Examination of the perianal area, digital examination of the rectum, sigmoidoscopy.
- Plain radiography of the abdominal cavity to exclude complications.
- Colonoscopy
with ileoscopy is a mandatory procedure to establish the diagnosis of UC, as well as to decide on colectomy. - A biopsy of the colon mucosa is also required during the study in most cases.
- Ultrasound examination of the abdominal organs, retroperitoneal space, pelvis.
- If it is impossible to conduct an endoscopic examination of the colon and ileum, it is possible to perform a computed tomography or magnetic resonance imaging with ascertainment of the intestine.
For additional indications the following is carried out:
- fibrogastroduodenoscopy;
- video capsule endoscopy;
- single or double balloon enteroscopy.
Treatment of nonspecific ulcerative colitis of the intestine
Treatment options for UC include medications, surgery, psychosocial support, and dietary advice.
Mild and local forms of the disease can be treated on an outpatient basis; moderate and severe forms of the disease require hospitalization:
- Diet and its regularity are important. In remission, the diet should contain a sufficient amount of plant fiber, fresh vegetables and fruits. Patients with UC do not need significant restrictions during the period of remission. During the period of exacerbation and diarrhea, it is possible to limit foods that stimulate motility (dairy, fermented milk, fresh vegetables and fruits).
- Depending on the form and severity of the disease, anti-inflammatory drugs, hormones, immunosuppressants, antibiotics, and biological therapy can be taken alone or in combination.
Some complications of the disease require surgical treatment. We are talking about the following conditions:
- perforation of the intestinal wall,
- toxic intestinal dilatation,
- intestinal stenosis,
- bleeding,
- malignant neoplasms.
Surgical treatment of ulcerative colitis can also be used in cases of severe disease and ineffective therapeutic treatment.
What questions should you ask your doctor?
To get the desired results from interacting with doctors, you need to find a common language with them. The patient’s interest in his own health is the best proof that he will follow all the specialist’s recommendations completely.
Ask your doctor the following questions:
- Could another disease in the body cause similar symptoms?
- What tests will be required to diagnose ulcerative colitis or another disease?
- What are the features of taking tests?
- What areas of the gastrointestinal mucosa are affected?
- Does current treatment need to change?
- What are the consequences if you stop taking the medication?
- What side effects may the prescribed medications have?
- How to behave if side effects occur while taking medications?
- What should be the behavior when symptoms of the disease appear?
- What symptoms should be considered extreme to promptly seek medical help?
- Do I need to change my usual diet? If so, what principles should be followed?
- Do I need to visit a doctor regularly to monitor the progress of the disease?
These and other questions with answers will help you adjust your behavior and lifestyle to make it more comfortable in combination with ulcerative colitis
Treatment methods
Treatment of ulcerative colitis includes the following measures:
- Following a special diet. By eating the right foods and avoiding junk food, there is a positive effect on the rectal mucosa. Inflammation is relieved, the processes of fermentation and putrefaction in the body are reduced, intestinal function is normalized, etc. It is necessary to introduce liquid, semi-liquid and pureed dishes, steamed or cooked in water, into the diet. It is strictly forbidden to eat food at too high or, conversely, too low a temperature.
- Drug therapy. It involves taking certain medications - corticosteroids, immunosuppressants, aminosalicylates. In addition, biological therapy is used.
- Anti-relapse treatment. To stop relapses, the doctor prescribes aminosalicylates for a course of 6 months. In the future, based on the behavior of the disease, the doctor regulates the use of this drug.
- Surgical methods of treatment. They are prescribed if conservative therapy does not produce any results, and the disease proceeds with complications. In this case, the colon is removed.
The treatment program for ulcerative colitis is drawn up based on the degree of development of the disease, as well as the location of the lesion. If this is a mild form of the disease, outpatient treatment is possible. If the disease is quite complicated, then the patient must be hospitalized and undergo inpatient treatment.
Treatment
Therapeutic tactics for ulcerative colitis are determined by the localization of the pathological process in the colon, its extent, the severity of the attack, and the presence of local and/or systemic complications. Conservative therapy is aimed at stopping the attack as quickly as possible, preventing relapse of the disease and progression of the process. Distal forms of ulcerative colitis—proctitis or proctosigmoiditis—are characterized by a milder course, so they are most often treated on an outpatient basis. Patients with left-sided and total lesions are usually treated in a hospital, since the course of the disease in them is characterized by greater severity of clinical symptoms and greater organic changes.
The food of patients should be high in calories and include foods rich in proteins, vitamins, limiting animal fats and excluding coarse plant fiber. We recommend low-fat fish, meat (beef, chicken, turkey, rabbit), boiled or steamed, pureed cereals, potatoes, eggs, dried bread, walnuts. Raw vegetables and fruits are excluded from the diet, as they contribute to the development of diarrhea. Patients often have lactase deficiency, so dairy products are added only if they are well tolerated. These recommendations correspond to diets 4, 4B, 4B of the Institute of Nutrition of the Russian Academy of Medical Sciences.
All medications used in treatment regimens for ulcerative colitis can be divided into two large groups. The first combines basic anti-inflammatory drugs and includes aminosalicylates, i.e. drugs containing 5-aminosalicylic acid (5-ASA, mesalazine), corticosteroids and immunosuppressants. All other drugs play either an auxiliary role in the treatment of ulcerative colitis or are at the stage of clinical study.
The first drug containing 5-ASA was sulfasalazine (salazosulfapyridine), which was introduced into clinical practice in 1942. Sulfasalazine consists of two components linked by a nitrogen bond - sulfapyridine sulfanilamide and 5-ASA. It has been proven that only 5-ASA has an anti-inflammatory effect. Sulfapyridine was forced to be included in the sulfasalazine molecule, since “pure” 5-ASA is well absorbed in the small intestine, and in the mucous membrane it turns into an inactive metabolite - N-acetyl-5-ASA. In sulfasalazine, sulfapyridine acts solely as a “carrier” that allows delivery of 5-ASA to the affected areas of the colon. Under the influence of colonic microflora, the nitrogen bond is destroyed. Sulfapyridine is absorbed in the colon, undergoes detoxification in the liver through acetylation and is excreted in the urine, and 5-ASA, in contact with the mucous membrane, has an anti-inflammatory effect.
The mechanisms by which 5-ASA exerts its anti-inflammatory effect are not fully understood. Nevertheless, numerous effects are known due to which mesalazine inhibits the development of inflammation. Thus, by inhibiting cyclooxygenase, mesalazine inhibits the formation of prostaglandins. The lipoxygenase pathway of arachidonic acid metabolism is also suppressed, and the release of leukotriene B4 and leukotriene sulfopeptide is inhibited.
At high concentrations, mesalazine can inhibit certain functions of neutrophil granulocytes in humans (eg, migration, degranulation, phagocytosis, and the formation of toxic oxygen free radicals). In addition, mesalazine inhibits the synthesis of platelet-activating factor. Due to its antioxidant properties, mesalazine is able to scavenge free oxygen radicals.
Mesalazine effectively inhibits the formation of cytokines - interleukin-1 and interleukin-6 (IL-1, IL-6) - in the intestinal mucosa, and also suppresses the formation of IL-2 receptors. Thus, mesalazine interferes directly with immune processes.
The "bullet" component sulfapyridine has been shown to be primarily responsible for the overall incidence of sulfasalazine side effects. Literature data on the frequency of side effects caused by sulfasalazine range from 5 to 55%, averaging 21%. In addition to nausea, headache, male infertility, anorexia, dyspeptic disorders, hematological reactions (leukopenia and hemolytic anemia) and hypersensitivity reactions with multiple organ lesions occur.
In order to maintain the anti-inflammatory activity inherent in sulfasalazine and avoid the side effects associated with the sulfapyridine component, preparations containing “pure” 5-ASA have been developed in recent years. An example of a new generation of aminosalicylates is the drug salofalk, developed by the German pharmaceutical company. The drug is available in three dosage forms: tablets, suppositories and microenemas. In tablets, mesalazine is protected from contact with gastric contents using a special acid-resistant polymer shell, which dissolves at pH levels above 6.5. These are the pH values that are usually recorded in the lumen of the ileum. After dissolution of the membrane, a high concentration of the active anti-inflammatory component (mesalazine) is created in the ileum. The choice of a specific dosage form of salofalk is determined by the extent of the zone of inflammation in the colon. For proctitis, it is advisable to use suppositories, for left-sided lesions - microenemas, and for total colitis - tablets.
Pentasa, which recently appeared in Russia, while being just as effective, has a number of features. It differs from other mesalazine preparations in its microgranular structure and the nature of its coating. Pentasa tablets consist of microgranules in an ethylcellulose coating, the dissolution of which does not depend on the pH level in the gastrointestinal tract. This ensures a slow, gradual and uniform release of 5-ASA throughout the intestinal tube, starting from the duodenum. The uniformity of release contributes to a constant concentration of the drug in different parts of the intestine, which does not depend not only on pH, but also on the transit rate, so Pentasa can be successfully used for inflammatory bowel diseases with diarrhea with virtually no losses. These features make it possible to use the drug not only for ulcerative colitis and Crohn's disease with damage to the colon and ileum, but also, most importantly, in patients with high-intestinal localization of Crohn's disease.
The daily dose of aminosalicylates is determined by the severity of the attack of ulcerative colitis and the nature of the clinical response to the drug. To stop an acute and moderate attack, 4-6 g of sulfasalazine or 3-3.5 g of mesalazine per day are prescribed, divided into 3-4 doses. In the absence of a good clinical response, the daily dose of mesalazine can be increased to 4.0-4.5 g, however, it is usually not possible to increase the daily dose of sulfasalazine due to the development of severe side effects.
Sulfasalazine blocks the conjugation of folic acid in the brush border of the jejunum, inhibits the transport of this vitamin, and inhibits the activity of the enzymatic systems associated with it in the liver. Therefore, the treatment complex for patients with ulcerative colitis receiving treatment with sulfasalazine must include folic acid in a dose of 0.002 g 3 times a day.
It usually takes 3 to 6 weeks to stop an attack of ulcerative colitis. After this, anti-relapse treatment is carried out with sulfasalazine (3 g/day) or mesalazine (2 g/day).
Of the modern drugs for the treatment of proctosigmoiditis and left-sided colitis, the suspension of salofalk is most often used. Disposable containers contain 4 g of mesalazine in 60 ml of suspension or 2 g of mesalazine in 30 ml of suspension. The drug is administered into the rectum 1-2 times a day. The daily dose is 2-4 g, depending on the severity of the process in the intestine. If the extent of the inflammatory process in the rectum is no more than 12 cm from the edge of the anus, it is advisable to use salofalk suppositories. The usual daily dose in these cases is 1.5-2 g.
When using aminosalicylates, it is possible to achieve remission in 75-80% of cases of ulcerative colitis.
The most effective anti-inflammatory drugs in the treatment of ulcerative colitis remain steroid hormones, which in severe forms of the disease are superior in activity to aminosalicylates. Corticosteroids accumulate in inflammatory tissue and block the release of arachidonic acid, preventing the formation of prostaglandins and leukotrienes, which cause the inflammatory process. By blocking chemotaxis, steroid hormones indirectly exhibit an immunomodulatory effect. The effect on tissue fibrinolysis leads to a decrease in bleeding.
- acute severe and moderate forms of the disease and the presence of extraintestinal complications;
— left-sided and total forms of ulcerative colitis with severe and moderate course in the presence of III degree of activity of inflammatory changes in the intestine (according to endoscopic examination);
- lack of effect from other treatment methods for chronic forms of ulcerative colitis.
In acute severe form of ulcerative colitis or severe attack of chronic forms of the disease, treatment should begin with intravenous administration of prednisolone at least 120 mg/day, evenly distributed over 4-6 injections with simultaneous correction of water and electrolyte disturbances, administration of blood and blood substitutes and (if possible) hemosorption in order to quickly eliminate endotoxemia. The hydrocortisone suspension should be administered intramuscularly, but the duration of such administration is limited to 5-7 days due to the likely development of abscesses at the injection sites and possible fluid retention. After 5-7 days, you should switch to oral prednisolone. During this time, gastroscopy is performed to exclude peptic ulcers of the stomach and duodenum. In case of a moderate form and the absence of clinical signs and anamnestic indications of gastroduodenal ulcers, treatment should immediately begin with oral prednisolone. Typically, prednisolone is prescribed at a dose of 1.5-2 mg/kg body weight per day. A dose of 100 mg should be considered the maximum.
If hormonal drugs are well tolerated, it is recommended to take the prescribed dose until a lasting positive result is obtained - within 10-14 days. After this, a reduction is carried out according to the so-called stepwise scheme - by 10 mg every 10 days. Starting from 30-40 mg, a single dose of prednisolone in the morning is recommended, which practically does not cause serious complications. At the same time, mesalazine or sulfasalazine is included in the treatment regimen, which should be taken until the hormones are completely withdrawn. Starting from 30 mg, prednisolone is withdrawn more slowly - 5 mg per week. Thus, the full course of hormonal therapy lasts from 8 to 12 weeks. depending on the form of ulcerative colitis.
In distal forms of the lesion and I-II degree of process activity according to sigmoidoscopy data, hydrocortisone should be prescribed rectally by drip or in microenemas. Moreover, if patients have difficulty maintaining large volumes, then the administration of hydrocortisone (65-125 mg) should be started in 50 ml of isotonic sodium chloride solution and, as the inflammation subsides and the frequency of false urges decreases, gradually increase the volume to 200-250 ml per therapeutic enema. The drug is usually administered after bowel movements in the morning or before bed.
For ulcerative proctitis and sphincteritis, suppositories with prednisolone (5 mg), administered 3-4 times a day, have a fairly good effect. In more severe distal forms, accompanied by increased body temperature, general weakness, anemia and III-IV degrees of activity according to rectoscopy, in cases of no effect from sulfasalazine or mesalazine, treatment with oral prednisolone at a dose of 30-50 mg/day is indicated.
In middle-aged and elderly patients, the dose of prednisolone should not exceed 60 mg, since they are characterized by the presence of concomitant diseases: atherosclerosis, hypertension, diabetes mellitus, etc. In cases where ulcerative colitis occurs against the background of atherosclerotic lesions of the mesenteric arteries, therapeutic the complex should be administered with vascular drugs: trental, prodectin, etc.
Hormone therapy is associated with the development of side effects: retention of fluid, chlorides and sodium in tissues (edema is possible), arterial hypertension, hypokalemia, calcium loss, osteoporosis, various autonomic disorders, carbohydrate metabolism disorders, adrenal insufficiency, stomach ulcers, gastrointestinal bleeding . In these cases, it is recommended to prescribe adequate symptomatic therapy: antihypertensive drugs, diuretics, calcium supplements, antacids. If carbohydrate metabolism is disturbed, a diet with limited carbohydrates is necessary; according to indications, fractional administration of insulin (according to glycemia) or oral antidiabetic drugs. To prevent the development of thrombosis in patients with severe forms of ulcerative colitis receiving hormonal treatment, constant monitoring of the blood coagulation system should be carried out and at the same time antiplatelet agents should be prescribed: chimes, prodectin, etc.
ACTH-zinc phosphate is effective only in the acute form of ulcerative colitis, since its effect is mediated by the preserved function of the own adrenal glands. The drug is administered intramuscularly at a dose of 20-40 mg, depending on the severity of the attack.
In recent years, in the treatment of inflammatory bowel diseases, especially Crohn's disease, drugs containing the glucocorticosteroid budesonide as an active component have been actively used. Unlike traditional glucocorticosteroids, budesonide has a very high degree of affinity for receptors and high (about 90%) first-pass metabolism in the liver. Due to this, it has a very powerful local anti-inflammatory effect with a minimum number of systemic side effects. As an alternative to prednisolone and hydrocortisone, the drug budenofalk can be recommended. When developing the structure of budenofalk, the physiological characteristics of the gastrointestinal tract were taken into account. Each capsule of budenofalk contains about 350 microspheres consisting of budesonide, coated with a polymer shell that is resistant to the action of gastric juice. Release of budesonide from microspheres occurs in the ileum and colon at pH values above 6.4. Budenofalk is used to treat mild and moderate exacerbations of ulcerative colitis. The recommended daily dose is 1 capsule of budenofalk containing 3 mg of budesonide, 4-6 times a day.
The most serious problem in the treatment of ulcerative colitis is hormonal dependence and resistance. This group of patients has the worst results of conservative therapy and the highest surgical activity. According to the State Scientific Center for Cancer Research, hormonal dependence develops in 20-35% of patients with severe ulcerative colitis. Often, signs of dependence and resistance are observed simultaneously, forcing one to resort to unsafe and aggressive methods of influence.
Hormonal dependence is a reaction to glucocorticoid therapy, in which the positive therapeutic effect is replaced by reactivation of the inflammatory process due to dose reduction or withdrawal of corticosteroids. This is a special variant of refractory colitis. We believe that there are at least 4 different etiopathogenetic variants of hormonal dependence: true hormonal dependence, combined with steroid resistance, false, caused by inadequate treatment, chronic adrenal insufficiency itself, and a mixed or combined form.
Currently, the causes and mechanisms of the formation of hormonal dependence are completely unknown. Nevertheless, we believe that among the etiological factors, defects in hormonal therapy itself, persistent inflammatory activity, and a transient or persistent decrease in the function of the pituitary-adrenal system will undoubtedly find their place. Probably, in some cases, hormonal dependence and resistance are hereditary, in others they represent an acquired defect in hormonal receptors and an imbalance between proliferation and cell death, i.e., deregulation of apoptosis. The hypothesis of a low density of hormonal receptors in patients with inflammatory diseases of the colon, especially with refractory disease, has recently received convincing confirmation.
It is immunosuppressants that play a responsible role in the treatment of patients with inflammatory diseases of the colon with hormonal dependence and resistance. However, this role for various drugs is assessed ambiguously. First-line and long-term drugs include 6-mercaptopurine and azathioprine. They are excellent sparring partners for glucocorticoids. Purine analogues can reduce and cancel hormones in 60-70% of patients with hormonal dependence, subject to certain rules, namely: they must be prescribed simultaneously with hormones so that their effect has time to manifest itself. The daily dose of azathioprine should be no more than 150 mg. The effect can be expected only by the end of the 3rd month of continuous use. Purine analogues produce relatively few side effects, and they should be used in patients with hormonal dependence for as long as possible - 2-3 years or more.
The 2nd line drug for long-term therapy is methotrexate, which is used in cases of intolerance to azathioprine or the need to accelerate the effect. It is administered orally or intramuscularly at a dose of 30 mg/week. The result can be obtained in 2-4 weeks. Side effects are few. Unfortunately, like azathioprine, it does not provide a lasting effect. Exacerbations occur upon withdrawal. Outbreaks that are milder than before sometimes occur during therapy after 6 months. from the start of the reception.
Cyclosporine can be used orally, intravenously at a dose of 4-6 mg/kg body weight with a good and rapid effect, occurring within 5-7 days. The action is short-lived. It is more often used to interrupt an attack with a subsequent transition to immunosuppressants suitable for prolonged use.
Violation of the barrier functions of the colon in ulcerative colitis may cause the development of toxemia syndrome. To correct it, it is necessary to prescribe an appropriate complex, restore eubiosis, antibacterial therapy, hemosorption, and ultraviolet irradiation of autologous blood.
Due to pronounced metabolic disorders and the catabolic effect of steroid hormones, parenteral administration of protein preparations is advisable: serum albumin, plasma protein, essential amino acids.
To improve the processes of microcirculation and transcapillary exchange, the administration of rheopolyglgine and hemodez (in normal dosages) is indicated.
In case of anemia (hemoglobin 90 g/l and below), which is a sign of a severe attack of ulcerative colitis, it is recommended to carry out blood transfusion of 250 ml of same-type blood with an interval of 3-4 days. When the level of iron in the blood serum decreases, it is necessary to include iron supplements in the treatment complex.
Taking into account the immunological disorders in ulcerative colitis, immunomodulators, levamisole, thymalin, etc. are used in the treatment of the disease. However, their role is not completely clear, the therapeutic effect of their use is short-term, so the activity of these drugs as basic agents is doubtful.
It is advisable to recommend the use of immunomodulators in combination with basic anti-inflammatory treatment.
Vitamins of groups B, C, A, D, K are prescribed, which also help restore eubiosis in the intestines.
The treatment complex includes psychotropic drugs in usual dosages, focusing on individual tolerance.
Exacerbation of ulcerative colitis in some cases is accompanied by irritable bowel syndrome, most often manifested by constipation. In this case, it is justified to prescribe wheat bran or proprietary preparations containing ballast substances (mucofalk, etc.), which help normalize stool and at the same time act as enterosorbents.
Inpatient treatment ends when clinical-endoscopic remission is achieved, after which the patient is subject to dispensary observation in a clinic with a general practitioner, gastroenterologist or proctologist.
- -Etiology
- -Nonspecific ulcerative colitis (UC)
- -Epidemiology
- -Pathological anatomy
- -Pathogenesis
- -Clinical classification of ulcerative colitis
- -Local and systemic complications in ulcerative colitis
- -Differential diagnosis
- -Surgery
- -Diagnostics
Emotions and stress
Since the human body is a single system, the disease of some organs inevitably leads to the defective functioning of others. Thus, stress and emotional stress often negatively affect human health. However, there is no clear evidence that stress is an irritating factor for the recurrence of the disease.
It is important for people with ulcerative colitis to receive support and understanding from friends, family and doctors.
The chronic course of the disease can lead a person to depression, so the doctor always pays attention to the patient’s emotional state and, if necessary, prescribes antidepressants.
Complications of ulcerative colitis
With proper and timely treatment, complications of the disease can be avoided. However, you need to know what exactly they can be:
- profuse intestinal bleeding - when blood clots pass simultaneously with stool;
- swelling or bloating
- toxic megacolon (occurs quite rarely).
It is recommended that you discuss the topic of complications with your doctor in order to understand the possible deterioration of your own health and know the reasons for this phenomenon.
Forecast. Prevention
If you ignore the symptoms of the disease for a long time, it will transform into a severe form with a number of complications. In this case, surgery will be required. However, if surgery is not followed in a timely manner, serious complications or death are possible (11-49% of cases). If surgery is performed in a timely manner, it will reduce the risks of complications and death by three times.
Accordingly, a timely visit to the doctor, in-depth diagnosis, determination of the correct treatment program for ulcerative colitis and strict adherence to it by the patient will ensure good results.
To make an appointment with a specialist at the Miracle Doctor clinic in Moscow for consultation and choice of treatment tactics, call the numbers listed on the website of our medical center or use the online application form. We work without breaks or weekends so that patients can see a doctor and get help immediately after the onset of symptoms of the disease.
Diagnosis and treatment of ulcerative colitis
Modern diagnostic equipment, which is available in our clinic, allows us to detect even minimal manifestations of the disease at its initial stages.
Diagnostics
Diagnosis of ulcerative colitis at the Yauza Clinical Hospital is carried out within one or several days and includes a series of examinations that are selected individually, depending on the symptoms, severity and duration of the disease process.
When the rectum and sigmoid colon are affected, visual examination of the walls of the lower intestines using sigmoidoscopy gives an accurate idea of the presence and severity of the disease. If the ulcerative process affects the overlying parts of the intestine, colonoscopy, intestinal X-ray with contrast, or MRI on a modern tomograph may be additionally prescribed.
Endoscopic examinations are performed at partner clinics and can be performed under anesthesia provided by an experienced anesthesiologist.
Conservative therapy
Depending on the results of the examination, the gastroenterologist prescribes a treatment program using immunosuppressants (azathioprine) and anti-inflammatory drugs (sulfasalazines), corticosteroids (prednisolone), antibacterial drugs, and sedatives.
A diet is prescribed to reduce the irritating effect of food on the intestinal wall (mechanical and thermal sparing, limiting the consumption of vegetables and fruits, using food with easily digestible and absorbable protein).
Surgery
In later stages, when complications develop, patients often require surgical treatment. At the Yauza Clinical Hospital, it is possible to perform a minimally invasive surgical laparoscopic operation to remove the affected area of the intestine without a wide incision. The operation is performed through small puncture incisions and ensures a faster recovery and the absence of an extensive postoperative scar.
Hemocorrection
The use of modern technologies in our hospital - extracorporeal hemocorrection - allows us to quickly cope with exacerbations and better control the course of the disease. This is explained by the removal from the blood of autoantibodies that support autoimmune inflammation in the intestinal wall. In addition, the use of blood cells as drug transporters makes it possible to reduce drug dosages without reducing their effectiveness. This significantly facilitates the tolerability of drug treatment and reduces the side effects of hormone therapy.
The doctors at our medical center do everything possible to make life easier for patients with nonspecific intestinal ulcers. Specialists work using a modern scheme for diagnosing and treating nonspecific ulcerative colitis, which ensures efficiency and speed in achieving a positive result.
Cost of services
You can see prices for services