The gallbladder performs an important function in the body; disruption of its functioning can lead to very unpleasant consequences. Bile produced by the liver is stored in the gallbladder until the body needs it. This usually happens when food enters the stomach. Bile begins to flow into the duodenum, where, together with pancreatic juice, it helps digest food and facilitates bowel function. What are the symptoms of a kinked gallbladder?
What is inflection
What is a gallbladder bend? To understand what pathology is, you need to remember how the organ works.
Outwardly, it resembles a pear; the bubble consists of three parts:
- bottom;
- body;
- neck.
On one side, the gallbladder is connected to the liver, this happens through the cervix. As a result, a channel is formed through which bile flows. The process of bile circulation occurs continuously. If the organ functions normally, the liver, intestines, and stomach receive an amount of bile that is sufficient to digest food and other natural processes.
Deformation or curvature of an organ occurs for various reasons. Depending on which area has undergone undesirable changes, the type of disease is also distinguished. In some cases, a twisted gallbladder is a congenital pathology, but more often it has an acquired form.
Often congenital inflection is a pathology acquired during the first trimester. Among the causes are infectious diseases suffered by a woman after conception and bad habits.
Bend of the gallbladder neck treatment
There is no specific method or treatment for this disease. An operation can be prescribed only in case of serious complications; it is not performed unless absolutely necessary.
The patient must adhere to a strict diet with a healthy diet, where food should not be consumed in large portions. There should be an interval between meals, which should be at least four hours. And after eating you need to rest for about half an hour, but do not lie down.
A kink in the neck of the gallbladder can be treated with exercise. But any of them must be agreed upon with a specialist. As a rule, people with this disease are recommended to exercise to strengthen the diaphragm and anterior abdominal wall. With the help of breathing exercises, the patient can get rid of bile stagnation.
If you correctly observe and follow all the doctor’s prescriptions, then the bend does not pose any particular harm to health and is not a terrible diagnosis . But, if neglected and not given due attention, this will lead to adverse and serious consequences.
Kinds
There are several options for classifying pathology, depending on the type of development it is:
- temporary - functional;
- constant - persistent, fixed bends.
The permanent form of kinks of the gallbladder is more common. The main classification, which allows diagnosing pathology and selecting treatment, is associated with the location of the inflection. Pathology can affect:
- bending of the body;
- necks;
- bottom;
- duct between the bladder and the liver.
An inflection in the body and bottom of the gallbladder is less common; damage to the neck of the organ is more often diagnosed. At the same time, the size of the cervix changes, so the pathology is easy to diagnose by ultrasound. A gallbladder with a bend in the body quickly loses its functionality, the outflow of bile is disrupted, so this type of pathology is considered the most dangerous.
Depending on the shape of the bend of the gallbladder, the degree of development of the pathology is determined. The organ can be bent into the shape of an arc, an hourglass, or a hook. There is also an S-shaped or double bend, which results in double torsion of the organ. Usually one bend is diagnosed, less often two; more is extremely rare.
Fact. An S-shaped bend is often found among the congenital form of the pathology.
The bend does not need to be straightened or treated
This statement is a logical continuation of the first. In most cases, a standard bend does not affect the functionality of the gallbladder and does not provoke the development of other diseases. Gastroenterologist Sergei Vyalov urges once again “not to stuff yourself with medications” if your gall bladder does not hurt. It is much better not to overload it with excess fatty, fried, smoked and spicy foods.
— Gallstone problems are cured quite simply and quickly. You need to understand how it works, then things will go smoothly. And no cleaning will be needed. In general, cleanings do not give anything other than the usual reduction of the bladder. Therefore, they cannot cure anything. They only overload the gall duct, and if there is inflammation or stones in it, they cause an attack or jam stones into the duct,” explains the doctor.
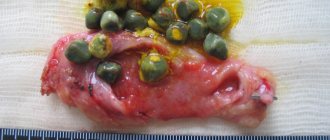
Photo
The photo below shows different types of pathology, in which the bladder is twisted in different places. And it is also shown, using the example of torsion in the cervical area, what a healthy and changed organ looks like.
Prevention
As is known, the prerequisites for the development of congenital pathologies are laid in the first weeks of intrauterine development of the fetus.
Therefore, the expectant mother needs to take care of her health even during pregnancy planning. And when pregnancy has occurred, it is necessary to visit a doctor in a timely manner and carefully follow all his recommendations.
Performing this gymnastics helps get rid of pathology
Symptoms of bending in adults
Symptoms of gallbladder deformation may not be obvious at first; sometimes a person finds out about the presence of pathology by chance, while doing a routine ultrasound of the internal organs. As the bend develops, some signs appear. Unfortunately, as pathology progresses in adults, its symptoms are often confused with other diseases and left unattended.
Gallbladder congestion
With the development of deformation of the gallbladder, the following often appear:
- pain in the abdominal area, which is aching in nature, can radiate to the area of the scapula and collarbone on the right side;
- nausea, frequent vomiting;
- constipation or diarrhea;
- bitter taste in the mouth due to impaired bile flow;
- belching, heartburn;
- staining of urine in very dark colors;
- stool discoloration;
- flatulence;
- loss of appetite, sudden weight loss.
Most of these symptoms are signs of diseases of the digestive system, such as gastritis and others. It is difficult to determine from them that changes have occurred in the gallbladder and it is bent. Therefore, doctors advise avoiding self-medication, especially without establishing an accurate diagnosis.
In rare cases, the pathology may disappear without therapeutic intervention, so that the person does not know about its existence.
Treatment methods
Therapy is expected to be comprehensive - diet and medication, and in difficult cases surgery is indicated.
Conservative therapy
Patients are prescribed table No. 5 according to Pevzner. Fried, fatty, alcohol, carbonated drinks and foods that cause gas formation are excluded from the diet. The main goal of this diet is to reduce the load on the biliary system and prevent a sharp outflow of bile. If there is no severe pain, you can eat as usual, but without harmful foods. Food should be varied and nutritious. You need to eat 4-6 times a day in small portions. The diet should be combined with taking B vitamins, as well as E, K, A, C.
- Choleretic drugs.
- Broad spectrum antibiotics.
- Antispasmodics.
- Quitting smoking and active lifestyle.
Surgery
The operation is carried out when there is some kind of obstruction that needs to be removed. It could be a cyst, tumor, scar. Different methods are used for different diseases:
- Praderi drainage - is carried out when forming an artificial connection between the small intestine and the bile duct so that there is no narrowing of the operated area. Also performed after removal of the gallbladder to maintain normal pressure in the common bile duct.
- Stenting - when the duct narrows, an expanding stent is installed into it - a thin tube made of metal or plastic. The stent restores patency.
- Endoscopic papillosphincterotomy is a gentle operation to remove stones from the ducts using a special probe.
Causes
Congenital kink develops in a baby in the womb and is usually diagnosed before the age of one year. Typically, the diagnosis of gallbladder deformity is not chronic. It doesn’t matter whether the bend is diagnosed in the body, cervix or bottom, as the child grows, the organ also stretches and changes. Often, by the age of 4–5 years, no trace remains of the congenital pathology.
Acquired bending of the gallbladder is more common; the main causes of the development of the disease are:
- cholecystitis and other diseases of the bladder associated with inflammation of its walls, the treatment of which was not started on time;
- bile stagnation;
- excessive physical activity, frequent heavy lifting;
- formation of adhesions on the gallbladder;
- diseases of the digestive system leading to an increase in organ size;
- fat deposits on the walls of the bladder.
Fat deposits often occur due to poor nutrition, excessive consumption of fatty and other unhealthy foods.
There are also predisposing factors that accelerate the development of pathology. These include:
- age-related changes - according to statistics, a bend in the gallbladder is more often diagnosed in people aged 55–60 years and older;
- sedentary work, especially if a person constantly sits in an incorrect position;
- obesity - extra pounds accumulated due to bad eating habits provoke excessive pressure on the gallbladder, which leads to its deformation.
Symptoms of the disease
Congenital gallbladder anomaly does not have any severe symptoms or consequences. However, when a baby is switched to regular food, specific symptoms appear: vomiting and lightening of the stool, and possible diarrhea. This is due to insufficient bile production.
At school age, the child develops painful attacks located under the ribs on the right. Sometimes morning sickness and bitterness, flatulence, heartburn and mild bloating appear. As a result of acquired bending of the neck or other part of the gallbladder, adults and schoolchildren report the same symptoms:
- severe nausea and vomiting;
- problems with stool, including frequent constipation, heaviness in the stomach;
- general weakness in the body;
- sharp painful sensations in the peritoneum;
- frequent bowel movements;
- facial skin becomes grayish-yellow;
- sometimes the temperature rises;
- a yellow coating appears on the tongue.
In adulthood, pain may appear in other areas if the neck, bottom or body of the bladder is affected. The pain can reach the collarbone, it radiates to the right shoulder blade and sternum.
Possible consequences
It is necessary to combat the pathology immediately after its discovery; if nothing is done, serious complications develop. With the healthy functioning of the gallbladder, bile emerges from it through the ducts, which has the property of breaking down fats. When an organ is deformed, it stagnates, which means that the level of fatty acids in the blood that have not been broken down increases greatly, and glucose oxidation also worsens.
Due to the cessation of fat breakdown and disturbances in glucose processing, there is a risk of developing diabetes mellitus.
As a result, the following changes occur in the human body:
- vision decreases;
- there is a sharp gain of extra pounds;
- the elasticity of blood vessels decreases - the risk of developing diseases of the cardiovascular system increases;
- the contractile functions of the muscles of the heart and other organs decrease.
One of the most difficult consequences of long-term deformation of the gallbladder is the risk of developing peritonitis. Cracks appear in the walls of the organ, through which bile flows out and spreads throughout the abdominal organs and beyond. As a result, inflammatory processes develop intensively, perhaps even over several days.
Peritonitis requires urgent surgical intervention, otherwise there is a risk of death.
Treatment options
The inflection of the bile duct does not go away asymptomatically
Treatment of defects formed in the structure of the bile reservoir is carried out mainly by conservative methods. The doctor must prescribe to the patient special medications that have a predominant choleretic effect in the body, as well as various types of antispasmodics that prevent excessive accumulation of bile in the body. Physiotherapeutic methods are also widely used. Special procedures prescribed by the attending physician are aimed at improving blood flow to the organ and restoring the activity of all existing muscles, as well as promoting their normal functioning.
In many cases, the child is prescribed to visit sanatoriums and resorts in order to increase the effectiveness of treatment.
The sick child is prescribed a special diet. Usually, high-fat, fried, and spicy foods are excluded from the daily menu. There is no need to pamper your child with an abundance of sweets and confectionery. Also, do not overuse flour products and various baked goods.
Diagnostics
Bend of the gallbladder is one of the forms of organ deformation. At the same time or separately, constriction, bending, twisting, and other modifications may appear. Therefore, the diagnosis usually sounds like gastric deformation. A detailed description can be provided by the doctor after diagnosis.
The main research method to establish an accurate diagnosis is ultrasound of the gallbladder. Its implementation requires certain preparation:
- you should not eat 10–12 hours before the procedure;
- dinner on the eve of the study should be light;
- if you cannot empty your bowels naturally, your doctor may prescribe an enema;
- Several hours before the ultrasound you should not drink anything, not even water.
- In addition to ultrasound, the doctor may prescribe:
- blood test (general and/or biochemistry);
- Ultrasound of other abdominal organs - to assess their condition, how much they have suffered due to the formation of a kink in the gallbladder;
- CT or MRI;
- X-ray with contrast injection.
If the patient consults a doctor in time, the symptoms indicate problems in the functioning of the gallbladder, and an ultrasound confirms its deformation, this is usually enough to make a diagnosis. If the doctor is not sure or the patient's condition is poor, additional diagnostics are required.
Inflection of the neck of the gallbladder diet
If the patient was nevertheless diagnosed with a bent gallbladder, then:
- You should definitely stop eating sweets.
- It is also strictly forbidden to eat sour, fried or spicy foods.
- You should not eat over-salted food.
- You should try not to eat things that are too cold.
- Products must be boiled or baked, but not raw.
When a bend in the neck of the gallbladder occurs, the diet should be followed as quickly as possible in order to cause minimal harm to the body.
But what is good to eat for such a disease?
1. Corn silk is a very useful product, as it has an excellent choleretic effect.
2. Corn oil is a great helper in easing the work of the gallbladder, so taking the oil should not be ignored.
3. Not least of all is pumpkin. You can use it in any form. You should eat within half a kilogram daily. Or you can drink one glass of juice.
4. Bee products can also have a therapeutic effect on this disease. In particular, this is pollen from flowers and beebread .
Reception should be carried out as follows:
- 1 teaspoon in the morning (on an empty stomach) - at least half an hour before breakfast.
And repeat the procedure 2-3 times a day, also before meals.
Strengthening the beneficial effects of pollen can be achieved by filling it with water (leaving for several hours) and taking small sips - portionwise, also before meals.
5. In addition, experts recommend using yellow gentian. An infusion is prepared from it :
- take gentian root (one tablespoon) and pour boiled, but not hot water (two glasses);
- leave to infuse for eight hours;
- then we filter the ready-made infusion and take 250 ml (¼ liter) morning and evening half an hour before meals;
Yellow gentian is an effective aid in the treatment of this disease.
6. It is also useful to use food additives from: beet, apple, pumpkin pectins. Since they improve peristalsis. Fruits and vegetables should only be consumed on an empty stomach or during the daytime.
7. You should not forget about the body’s water balance, so you need to increase the amount of clean, raw (preferably filtered) water you drink, which is necessary to avoid its deficiency, which will result in a rapid thickening of the bile formed.
Finally, it is recommended to thoroughly chew the food consumed , because the digestion process begins as a result of grinding and mixing food with saliva.
Treatment
The doctor decides how to treat the patient based on the diagnostic results. The basis of therapy is medications, the action of which is aimed at normalizing the outflow of bile and eliminating inflammatory processes. In addition to this, physiotherapy is prescribed. Compliance with diet and other recommendations of the attending physician plays an important role.
Traditional medicine for deformation of the gallbladder is powerless; they cannot in any way affect its position. They can only be used in addition to drug treatment as a general tonic.
Medication
Medications are selected based on the degree of development of the pathology, the general condition of the patient and the individual characteristics of his body. Among choleretic drugs, the following are often prescribed:
- Gepabene. Normalizes the flow of bile, has an antispasmodic effect, eliminating pain due to inflammation. And Gepabene also helps normalize liver function.
- Allohol. The advantages of the drug are its low cost. Allochol is often prescribed for diseases of the gallbladder. The composition of the drug is unique, which includes bile of horned animals, extracts of nettle and garlic.
- Flamin. It has a natural base and is effective due to the presence of flavonoids and glycosides. The drug normalizes bile synthesis and has antispasmodic and analgesic effects.
- Hofitol. A popular choleretic drug, which includes artichoke extract. It has a hepaprotective effect, eliminates discomfort and pain, reducing the inflammatory process.
Doctors often prescribe herbal remedies in addition to medications, which usually require long-term use.
And Odeston, Ursofalk, Tanacechol, Nicodin and other drugs belonging to the choleretic group can also be prescribed.
Dyskinesia (dysfunction) of the biliary tract
Treatment for gallbladder dysfunction includes:
- mode,
- diet therapy;
- drug therapy;
- physiotherapy;
- hydrotherapy;
- Spa treatment.
Treatment of patients with dysfunction of the gallbladder and sphincter of Oddi is often carried out on an outpatient basis.
Treatment of hypertensive type of gastric dyskinesia:
- With the hypertensive type of dyskinesia, a state of psycho-emotional comfort and peace is very important for patients. After the elimination of the pain syndrome and signs of exacerbation, the patient’s regimen expands.
- Diet therapy is essential. The general principles of the diet are a diet with frequent meals of small amounts of food (56 meals a day) with the last meal immediately before bed, which promotes regular emptying of the bile ducts and eliminates bile stagnation.
For the hypertensive type, it is recommended to limit foods that stimulate bladder contractions - animal fats, meat, fish, mushroom broths, eggs.
A good effect in this form of functional disorders is provided by drugs belonging to the group of cholespasmolytics.
The group of cholespasmolytics and anticholinergics includes the following drugs:
- Atropine sulfate, 0.1% solution is prescribed orally, 5-10 drops. appointment.
- Bellalgin (analgin 0.25 g; anesthesin 0.25 g; belladonna extract 0.015 g; sodium bicarbonate 0.1 g) take 0.51 tablets 2-3 times a day.
- Besalol (belladonna extract 0.01 g, phenyl salicylate 0.3 g) is prescribed 1 tablet. 2 times a day.
- Metacin is used 1 tablet. 2-3 times a day. For colic, the drug is injected subcutaneously or into the muscle, 1 ml of 0.1% solution.
- Platiphylline is prescribed 1 tablet. (0.005 g) 2-3 times a day before meals for 100 days. For colic, the drug is administered subcutaneously, 1 ml of a 2% solution 1-3 times a day.
- Euphylline (theophylline 80%; ethylenediamine 20%) 1 tablet. (0.15 g) 1 time per day.
- In case of hypertensive dysfunction of the gallbladder, cholespasmolytics of synthetic origin are more often used.
- Noshpa (drotaverine hydrochloride) is prescribed in tablets of 0.04 g 1-3 times a day for 14 days or more or in ampoules of 2 ml of a 2% solution intramuscularly or intravenously 1-2 times a day.
- Papaverine (papaverine hydrochloride) is prescribed orally in tablets of 0.04 or 0.01 g 3 times a day or intramuscularly (intravenously) 2 ml of a 2% solution.
Combined cholespasmolytics include nicoshpan (nicotinic acid 22%; drotaverine hydrochloride 78%) 20 mg 1-2 times a day and papazole (dibazol 0.03 g; papaverine hydrochloride 0.03 g) 1 tablet. 2-3 times a day The disadvantage of drugs in this group is their non-selectivity, i.e. they act on the entire smooth muscle latura, including the urinary tract and blood vessels, and there is also the possibility of developing hypomotor dyskinesia and hypotension of the sphincter apparatus of the gastrointestinal tract.
The modern drug duspatalin (mebeverine), belonging to the group of myotropic antispasmodics, has a direct blocking effect on the fast sodium channels of the myocyte cell membrane, which disrupts the influx of Na+ into the cell, slows down the depolarization processes and blocks the entry of Ca2+ into the cell through slow channels, preventing the development of muscle spasm and pain syndrome. Duspataline has no effect on muscarinic receptors, which means that there are no side effects such as dry mouth, blurred vision, tachycardia, urinary retention, constipation, and weakness. The drug has a prolonged action; it is prescribed no more than 2 times a day in the form of 200 mg capsules for 2-4 weeks. By increasing the flow of bile into the small intestine, myotropic antispasmodics help improve digestion processes and activate intestinal motility, which leads to normalization of stool. Myotropic antispasmodics include selective blockers of calcium channels of smooth muscles: minavirin bromide (dicetel), it is prescribed 50-100 mg 3 times a day; spasmolin (otilonium bromide).
Odeston (7-hydroxy-4-methylcoumarin) is a myotropic antispasmodic with a choleretic effect. The drug enhances the formation and separation of bile, has a selective antispasmodic effect on the sphincter of Oddi and the sphincter of the gallbladder, which promotes good outflow of bile from the liver and biliary tract. Odeston has an indirect choleretic effect by facilitating the passage of bile into the gastrointestinal tract, which enhances the recirculation of bile acids. The advantage of the drug is the absence of adverse effects on the smooth muscles of the vascular walls and intestinal muscles; it does not increase pressure in the bile ducts and also does not impair the secretory function of the digestive glands and the absorption of nutrients. Thus, odeston helps improve digestion and peristalsis, normalize stool, eliminate constipation, and has a positive effect in cases of sphincter of Oddi dysfunction, dyskinesia of the gastrointestinal tract, chronic cholecystitis (including uncomplicated calculous), as well as in cases of disruption of the digestive processes caused by a deficiency of bile in the intestine. The daily dose of odeston is 600 mg (1 tablet 3 times a day). The duration of treatment is individual (from 1 to 3 weeks).
For biliary dyskinesia, herbal remedies such as arnica (flowers, tincture), valerian (rhizomes with roots), elecampane (rhizomes with roots), St. John's wort (herb), lemon balm (herb), peppermint (leaves), calendula are used (flowers), marshweed (herb), sage (leaves), convaflavin, olimetin, holagol, calamus, immortelle budra, capitol, snake knotweed, gorse, oregano, St. John's wort, centaury strawberry, calendula, willowherb, horseweed, hoofed grass, nettle , oregano, corn silk, cinquefoil erecta, flax, juniper, mint, dandelion, shepherd's purse, plantain, tansy, wormwood, kidney tea, wheatgrass, strap, rose, chamomile, knotweed, thuja, dill, fennel, hops, chicory, thyme, blueberry, celandine, sage, rosehip
In case of bladder dysfunction caused by increased tone of the sphincters of the biliary system, the intake of medications that have a choleretic and hydrocholeretic effect (bile acids, enzyme preparations, infusions and decoctions of choleretic herbs, synthetic choleretic drugs, gastric juice, etc.) is limited.
In order to stimulate bile secretion, reduce the tone of the common bile duct, which increases the flow of bile into the duodenum, cholekinetics are used - drugs that cause the production of cholecytokinin, which controls the kinetics of the gallbladder and sphincter of Oddi. The effect is due to the irritating effect of drugs of this group on the receptor apparatus of the duodenal mucosa.
In order to stimulate the formation and outflow of bile, as well as an antispasmodic effect, tea is used, which includes the following plants: spinach leaves (Folia Spinaciae), thistle fruits (Fructus Cardui Mariae), cinquefoil herb (Herba Anserinae), celandine herb (Herba Cheh' dorm), yarrow herb (Herba Millefolii), licorice root (Radix Liqumtae), rhubarb rhizome (Rhizoma Rhei), dandelion root and herb (Radix Taraxaci p. Herba), turmeric rhizome, turmeric oil (Rhizoma Curcumae, Oleum Curcumae) , aloe extract (Extractum Aloes).
A number of medicinal plants have a cholekinetic effect: (berberine sulfate), extracts from medicinal plant materials (calamus, rhizomes), barberry (tincture of leaves), sandy immortelle (flowers), lingonberry (leaves, shoots), blue cornflower (flowers), watch trifoliate (leaves), knotweed (herb), oregano (herb), calendula (flowers), coriander (fruit), juniper (fruit), dandelion (roots), shepherd's purse (herb), rhubarb (root), chamomile (flowers ), common thyme (herb), caraway (fruit), yarrow (herb), rose hips (fruit, cholosas), fennel (fruit).
The approximate treatment regimen for hypermotor dyskinesia of the gallbladder is the use of antispasmodics for rapid relief of pain (phosphodiesterase inhibitors - noshpa, papaverine) or anticholinergics (atropine, platyphylline) in combination with hepabene to reduce the tone of the sphincter of Oddi.
Treatment of hypotonic type of gastric dyskinesia. In the treatment of gallbladder dysfunction of the hypotonic type, it is advisable to expand the motor regimen.
These individuals tolerate weak broths, fish soup, cream, and sour cream well. Food with sufficient vegetable fat content (up to 80 g/day) and eggs are used. For 2-3 weeks, vegetable oil is prescribed, 1 tsp. 2-3 times a day 30 minutes before meals. To prevent constipation, raw vegetables are recommended: carrots, pumpkin, zucchini, greens. Bran has a pronounced effect on the motility of the biliary tract (1 tablespoon is brewed with boiling water and added as a gruel to various side dishes).
Prokinetics indicated: cisapride 5-10 mg 3 times a day; domperidone 5-10 mg 3 times a day 30 minutes before meals; metoclopramide 5-10 mg per day.
Drugs from the choleretic group, as well as bile acid drugs, have a good effect.
Drugs containing bile acids include the following:
- Lyobil (lyophilized bovine bile), tablets 0.2 g, 1-2 tablets. 3 times a day after meals. Course 1-2 months.
- Decholin (sodium salt of dehydrocholic acid), ampoules of 5 ml of 5% and 20% solution, administered intravenously 5-10 ml once a day.
- Cholecin (a compound of a salt of deoxycholic acid and a sodium salt of higher fatty acids) is prescribed in 1-2 tablets. 3 times a day before meals.
- Hologon (dehydrocholic acid), tablets 0.2 g, 0.2-0.25 g once a day. The course of treatment is 2-3 weeks.
Preparations of plant origin and medicinal plants that have a choleretic effect have a good effect on the function of the gallbladder: aqueous extracts from medicinal plant raw materials calamus (rhizome), barberry (leaf, root), birch (buds, leaves), immortelle sandy (flowers), barberry multi-veined (herb), knotweed (herb), goldenweed (herb), coriander (fruit), corn (columns with stigmas), burdock (roots), tansy (flowers), wormwood (herb), rowan (fruit ), hops (cones), chicory (herb), choleretic herbs No. 1 and 2, combined herbal remedies (holagogum, cholagol, holaflux, hepatofalplanta, hepabene, kurepar, flamin, fumetere, etc.).
In the presence of hypomotor dysfunction of the gallbladder against the background of increased tone of the sphincters of the extrahepatic bile ducts, Odeston 200 mg 3-4 times a day is added to drugs that enhance the contractile function of the gallbladder.
Effective in the treatment of hypomotor dyskinesia of the gallbladder with normal motor function of the gastrointestinal tract is the combined use of prokinetic drugs (metoclopromide, or domperidone, or 5-10% solution of magnesium sulfate, 1 tablespoon 2-4 times a day for 10-15 minutes before meals) with choleretic drugs containing bile acids or herbal products (allochol, cholenzyme, hepabene). Long-lasting biliary sludge during or after this therapy is an indication for the use of UDCA drugs for up to 3-6 months.
To correct hypomotor dyskinesia of the gallbladder in case of its combination with gastrointestinal tract and/or duodenostasis, a 2-week (if indicated and longer) treatment regimen is used, including prokinetics; choleretic preparations of plant origin or containing bile acids; antibacterial drugs in the presence of symptoms of bacterial contamination of the small intestine.
In the case of hypomotor dyskinesia of the gallbladder and colon, 24-week therapy is recommended, which includes prokinetics and choleretic drugs containing bile acids.
When hypofunction of the gallbladder is combined with intestinal hypermotility and dysbiosis, treatment with hepabene in combination with hilacomfort is indicated. In addition to these medications, intestinal adsorbents such as smecta, phosphalugel, etc. can be prescribed.
It is very effective to use probeless tubes with a decoction of rosehip, corn silk, warm mineral water, 10-25% solution of magnesium sulfate (1-2 tablespoons 2 times a day) or 10% solution of sorbitol or xylitol (50 ml 2 times in a day).
Method of “blind” probing according to Demyanovich
“Blind” probing is prescribed 23 times a week for 1 month. Probing is carried out as follows:
- In the morning on an empty stomach, the patient is given to drink 15-20 ml of a 33% solution of magnesia sulfate, heated to 40-50 ° C (instead of magnesia sulfate, you can use 1-2 egg yolks, warm olive or corn oil; 10% solutions of sorbitol, xylitol; warm mineral water type Essentuki-17; a glass of beet juice).
- It is necessary to place the patient on the right side on a cushion with a heat pad or paraffin application on the right side.
- During the procedure, take deep breaths (to open the sphinter of Oddi) - 23 breaths every 5 minutes.
Patients with biliary tract dysfunction are advised to use acupuncture and rational psychotherapy, which improves the psycho-emotional state, reduces the intensity of autonomic reactions and pain. It is important for the doctor to contact the patient, explain the causes of the disease and possible ways to eliminate it. Trust in the doctor largely determines the success of treatment.
Pharmacological correction of psychoneurological disorders is carried out with antidepressants. For this purpose, tricyclic antidepressants are used: amitriptyline, drugs with a serotonin reuptake mechanism (fevarin, Framex, etc.).
For vegetative-vascular dystonia and neurotic-neurosis-like syndrome, “minor” tranquilizers (Elenium, Tazepam, etc.) and sedatives are recommended: tincture of valerian, motherwort, 40 drops. 3-4 times a day or an infusion of these plants (10 g per 200 ml) 1 tbsp. l. 4 times a day.
Physiotherapeutic procedures are used in the treatment of gallbladder dysfunction:
- To improve microcirculation and trophic processes in patients with hypertensive dyskinesia, inductothermy is indicated.
- For hypotension, diadynamic currents and faradization of the gallbladder are prescribed.
- UHF has anti-inflammatory and bactericidal effects.
- Microwave therapy improves blood flow, tissue trophism, enhances redox processes, has anti-inflammatory and analgesic effects, and relieves spasms of the biliary tract.
- Applications of paraffin and ozokerite improve blood flow and tissue trophism, have a resolving effect and the ability to cause an antispasmodic effect in hypertensive biliary dyskinesia.
- For hypertensive dyskinesias, electrophoresis of a 5% novocaine solution and a 10% magnesium sulfate solution is indicated.
- Baths (pine, pearl) are prescribed every other day, for a course of 10-12 baths.
- Showers (rain, fan, circular) are recommended for 35 minutes, 10-15 procedures per course.
- Massage of the cervical collar area No. 10. Galvanic collar on the collar area.
- Electrophoresis of calcium chloride, bromine solution on the collar area, for a course of 7-10 procedures. Electrophoresis of 5% novocaine solution, 0.1% papaverine solution, 5% magnesium sulfate on the area of the right hypochondrium, for a course of 7-10 procedures.
Forecast:
The prognosis for dyskinesia is favorable. Working capacity has been preserved.