- Why does pain occur with hemorrhoids?
- Treatment of hemorrhoids
Hemorrhoids are a fairly common disease throughout the world. Out of 100 people, every fourth person can encounter it, and after 50 years - already every second1. In recent years, the prevalence of this disease has been increasing. Its reasons could be 2:
- physical inactivity;
- long sedentary work, including at the computer;
- long periods of driving;
- long standing work without movement;
- constipation, including during pregnancy;
- childbirth.
What else do you need to know about hemorrhoids?
- Often this delicate problem may be accompanied by constipation3.
- Together, these problems can increase pain, worsen symptoms, and increase the likelihood of bleeding.
- But even if there is no constipation and the stool is hard, every trip to the toilet can cause discomfort. Therefore, the question “How to relieve pain from hemorrhoids?” may become more relevant than ever.
How to painlessly go to the toilet with hemorrhoids
It is impossible to imagine hemorrhoids without symptoms of severe discomfort, which significantly impair a person’s quality of life. These include itching, pain, pasty condition in the anal area, enlarged lymph nodes, secondary infection, thrombosis of the anal fissure and other complications. Pathological symptoms intensify, especially during defecation. Preventing inflammation of the lymph nodes by regulating your diet and monitoring regular bowel movements may help.
Defecation during hemorrhoids directly depends on the quality and composition of food consumed. The emphasis in the diet for persistent constipation should be on fresh fruits and vegetables, grain products and dairy products.
In combination with proper nutrition (40 ml per 1 kg of body weight), beets, apricots, plums, olives, plums, figs will help soften the stool and make defecation easier without effort and pain.
It will be important to exclude from the diet foods that irritate the mucous membrane of the gastrointestinal tract: spicy, salty, fatty foods, canned food, spices, cookies. A balanced diet is the key to painless trips to the toilet if you have hemorrhoids.
The toilet should be used while taking non-steroidal anti-inflammatory painkillers (Diclofenac) or antispasmodics (No-Spa). Moreover, prolonged constipation (more than a day) should be relieved by taking laxatives (Duphalac).
Folk remedies for pain
Proponents of traditional medicine can relieve the pain that occurs during bowel movements using methods based on the use of various oils.
- Sea buckthorn oil is an excellent remedy that helps expand the anal canal and stretch the vascular walls, which under its influence become more resistant to injury. For internal hemorrhoids, before going to the toilet, it is recommended to give an enema using 50 ml of this oil.
- Castor oil, which has the ability to liquefy hard feces and remove them without hindrance. Castor oil can be taken orally in liquid form at the rate of 1 g per 1 kg of body weight or in the form of capsules (20-30 pieces per night). You can also perform a cleansing enema with this substance, which requires just a few drops of oil mixed with warm water.
- Milk thistle oil, which is recommended for constipation and hemorrhoids in the form of enemas. For one procedure, 30 ml of the substance is enough.
- Flaxseed oil, commonly used to prevent constipation in the presence of hemorrhoids. Due to the content of omega-3 and omega-6 acids, the oil normalizes metabolic processes in the body, which in turn contributes to the formation of soft feces.
- Tea tree oil – suitable for baths used to relieve pain after bowel movements.
- Camphor oil, which should also be applied to the anorectal area after bowel movement, using a gauze pad. The product not only softens inflamed areas, but also has a healing, antiseptic and anti-inflammatory effect.
- Butter, which can be used mixed with honey or chamomile. Suppositories made from such a substance and placed before defecation will soften the rectal mucosa and have an additional calming effect on it, while reducing the risk of bleeding.
Thanks to the existence of various modern drugs that have a laxative effect, as well as traditional medicine recipes, coping with the pain of constipation and hemorrhoids is not difficult. However, it is important to remember that the main weapon in this fight is your own calmness, a positive psychological attitude and properly adjusted nutrition.
Rules for bowel movements for constipation and hemorrhoids
Hemorrhoids and constipation are two sides of the same coin. Inflammation of hemorrhoids is often caused by damage to the rectal mucosa from feces, and constipation is caused by hemorrhoids on a psychological level (fear of pain during bowel movements). One way or another, the situation of irregular bowel movements requires simple rules:
- Optimal ratio of ballast products (fiber) in the daily menu;
- Simultaneous bowel movements, sometimes with the help of laxatives (don't hold back when you want to bowel movement);
- balance in the drinking system.
It is important to determine the cause of the “problem” and eliminate it. Constipation may seem easy to treat with laxatives, but this is not true. A sense of proportionality is necessary. Taking too much laxative can cause uncontrollable diarrhea or force your bowels to work on their own. Proctologists recommend Posterizan as an adjuvant in the form of ointments and suppositories with anti-inflammatory and analgesic properties that can protect the anus and anal skin from injury and local forms of hemorrhoids.
In addition, patients with constipation and hemorrhoids are advised to exercise and walk wisely.
Causes of pain
There are several reasons that explain pain during bowel movements when hemorrhoids develop.
- The hard consistency of stool, its compactness, which entails injury to the walls of the rectum, as well as existing hemorrhoidal cones. These phenomena can lead to not only pain, but also bleeding.
- Strong and improper tension during the act of defecation, which leads to blood flow to the vessels of the rectum and the formation of stagnation in it.
- Staying on the toilet for a long time, as a result of which the blood circulation in the pelvis is disrupted, and the hemorrhoids increase even more and thereby block the flow of feces.
- Untimely visiting the toilet, causing stagnation in the intestines, which leads to the formation of gases, bloating, and painful spasms. This factor contributes to even greater consolidation of feces and makes it difficult to remove, especially in conditions of acute hemorrhoids.
Knowing these provoking factors will help you successfully avoid constipation and the discomfort that accompanies it during bowel movements.
How to improve bowel movements during pregnancy and after childbirth
When it comes to bowel movements for hemorrhoids during pregnancy, there are a few things to consider. As a rule, hemorrhoids begin to bother the expectant mother in the second trimester, when the uterus has grown sufficiently and its pressure on the pelvic organs has become significant. Stagnation in the pelvic organs causes inflammation of the hemorrhoids, their growth, discomfort and pain during bowel movements, and psychogenic constipation.
From this moment, problems with defecation begin, which must be solved in the most gentle way, because the main task of the expectant mother is to give birth to a healthy baby and give him to the world. There are several rules that will help ease the situation:
- During bowel movements, you should not apply pressure, as the uterus may become more tense;
- Balance your diet with foods with laxative properties: beets, plums, carrot puree;
- calculate the drinking dose (40 ml per 1 kg of weight);
- walk more;
- as a last resort, use natural laxatives: Lactulose, Duphalac, Normaza (they are not addictive and do not affect the fetus).
Another option is sea buckthorn suppositories, which are completely safe for the fetus and mother. Micro gags allowed. All medications should be selected only by a doctor.
The recovery process after childbirth is often complicated by hemorrhoids. This makes bowel movements painful. In addition, if there were wounds and stitches during childbirth, the woman has an additional fear of going to the toilet. The following tips may help alleviate the situation:
- Normal psycho-emotional mood;
- Drinking water and prune decoction regularly without restrictions;
- proper nutrition;
- lack of physical inactivity;
- Immediate bowel movement;
- Kegel exercises.
The lack of effects is a reason to use laxatives based on lactulose and macrogol that are not harmful to the baby (breastfed): Prelax, Forlax, Tranzipeg.
Useful tips
Modern Internet resources, as well as many medical books, are full of various information about the causes of hemorrhoids, its types, and treatment methods. In addition, in this large information flow you can find useful and important tips that will make the process of going to the toilet as easy as possible with this disease.
- Proper nutrition, which was discussed above.
- Drink a sufficient amount of liquid, with preference given to regular drinking water.
- Compliance with basic rules of personal hygiene when visiting the toilet: first of all, this is the use of soft, non-scented toilet paper that does not cause irritation. In addition, in a situation of aggravated hemorrhoids, washing is important, which it is advisable to do after each act of defecation. An excellent and very convenient alternative to cleaning procedures is the use of alcohol-free wet wipes.
- Using underwear made from natural materials, as well as changing it daily.
- Going to the toilet at the same time is something you need to accustom your body to. The development of this reflex will allow the intestines to empty every day at a set hour, with the most ideal time being the morning, immediately after sleep or breakfast.
- Adopting the correct posture during the act of defecation, which implies a stable position with support on the full surfaces of the feet. In no case should you empty your bowels while half-squatting, since improper muscle tension can aggravate developing hemorrhoids. Arming yourself with this knowledge and putting it into practice will greatly help when going to the toilet.
How to go to the toilet without pain after hemorrhoid surgery?
The recovery period after a classic hemorrhoidectomy is a real challenge. Postoperative soreness is accompanied by painful bowel movements. Systemic pain relievers (Nise), an ice pack on the wound area, plenty of fluids, and a balanced diet as directed by your doctor may help improve the situation.
Reasonable exercise will also help, and in a pinch a short course of laxatives will help. All types of drugs are suitable: secretory, osmotic, prebiotics, intestinal fillers. The doctor will develop a course of action.
Where does it come from?
For many years, there was an opinion that hemorrhoids are the same disease as varicose veins of the lower extremities. In fact, there is its own, separate “base”. The basis of hemorrhoids is arterial-venous junctions, which every person has and is not a pathological condition. There are anastomoses between the muscles and the mucous membrane of the anus - three large “pads” inside and outside. Together with the muscles of the anal canal, they hold the intestinal contents. When the process of defecation occurs, the anastomosis “hides” into the muscles, freeing the passage of feces. In addition, anastomoses are special “stations” at which arterial blood mixes with venous blood. Unfortunately, the possibilities of venous outflow are limited, therefore, if the flow of arterial blood increases, “overloads” begin within the “station” itself. Actually, this is hemorrhoids.
How to ease bowel movements with hemorrhoids?
The basic principles of easing bowel movements for hemorrhoids are a balanced diet, a reasonable exercise routine and a lack of stress. Laxatives are used as a supplement.
Laxatives
Laxatives are used only for pain of more moderate intensity. Their advantage over non-drug therapy is obvious: rapid action, long-term therapeutic effect, elimination of the main negative symptoms, prevention of the progression of pathology. Currently, the best results are achieved with lactulose-based products.
In addition to laxatives, the most effective suppositories and ointments can be used in complex therapy in direct contact with the lesion. The most popular of them are Relief suppositories and ointments, Anestezol suppositories, Procto-Glivenol, Ginkor Procto, Troxevasin, Fleming ointment and Bezornil. If there is no result or to prevent complications, phlebotonics can be administered orally: Detralex, Phlebodia, Venarus, Pilex. The analgesic effect is shown by: Nise, Ibuklin, Ibuprofen in tablets. Pain that cannot be cured with novocaine blockade.
Folk remedies
Among the most effective folk remedies:
- castor oil;
- pharmaceutical preparation for constipation based on yarrow and nettle;
- burdock seeds;
- beet enema;
- Cool shower after bowel movement;
- cool bath while sitting;
- cold water compress on the anal area;
- infusions of chamomile, calendula, plantain and echinacea;
- Applications for knots from centipede leaves or grated raw potatoes;
It is important to understand that painkillers for hemorrhoids are effective in the early stages of the disease. Severe pain is treated with special medications prescribed by the doctor.
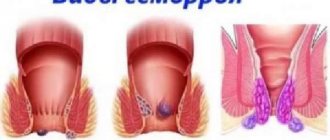
Causes and symptoms of the disease (briefly)
The exact cause of hemorrhoids is still not clear. Some factors increase pressure in the abdominal cavity and, therefore, provoke the disease. Pressure may cause bulging vessels, similar to veins, in the forehead or neck during exercise. The pressure expands the wall of the hemorrhoid. As a result, the vessels can lose elasticity and burst. During defecation, the feces compress the raised nodes. Sections of the vessels descend until they emerge from the anus.
Constipation, a low-fiber diet, and age contribute to the formation of hemorrhoids. On the other hand, the effect of pregnancy is considered uncertain. For other factors, only limited empirical evidence exists. However, risk factors that can be addressed have important health implications. In other words, a patient who prevents hemorrhoids also prevents the development of other common diseases.
The main risk factors for developing hemorrhoids:
- Unfavorable diet: a diet that lacks fiber contributes to hardening of the stool, causing acute or chronic constipation. All three conditions stress the vessels in the hemorrhoidal tissue,
- Dehydration: If the body does not have enough fluid, the stool becomes hard,
- Diarrhea, laxatives: prolonged diarrhea or taking laxatives provokes hemorrhoids,
- Hereditary factors: Scientists suggest that a hereditary predisposition to connective tissue weakness contributes to the development of the disease.
- Age: The disease is more common in older people, probably because the connective tissue loses its elasticity,
- Obesity: Patients with a high body mass index (BMI) have increased abdominal pressure, which increases the risk of hemorrhoids,
- Pregnancy and childbirth: in this case, expert opinions differ. Some scientists believe that both factors can cause and worsen hemorrhoidal disease. Others argue that this assumption is based on the fact that perianal venous thrombosis, which is common during childbirth and pregnancy, is often mistaken for true hemorrhoids.
- Certain diseases: diseases that increase the amount of blood in the abdomen (for example, heart failure, cirrhosis of the liver), increase pressure on the hemorrhoids,
- Sports: sports that increase pressure in the abdomen (weight lifting, abdominal exercises, etc.) contribute to the development of the disease,
- Poor anal hygiene: Feces can cause itching, inflammation and irritation of enlarged hemorrhoids.
Read also: Treatment of hemorrhoids with massage, main types of massage and manipulation techniques
Alcohol, spicy foods, chronic bronchitis, and sitting on cold ground have been found to influence the development of the disease in separate studies.
Alcohol is a factor contributing to the development of hemorrhoidal diseases
Slowly but surely he makes his way
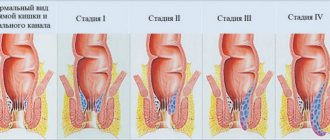
The first stage of hemorrhoids is an enlargement of the hemorrhoids, which is often accompanied by bleeding during bowel movements: prolonged overflow with blood causes stretching of the nodes and thinning of the walls, on which erosions and tears appear. The flowing blood is arterial and scarlet in color. There is also a bloodless option: itching, burning, sensation of a foreign body in the anus. These symptoms do not bother you constantly, but occasionally; Because of this, many patients believe that there is no problem. But chronic hemorrhoids tend to progress without serious treatment. From the beginning to the “advanced” stages it takes approximately 7-10 years. Hemorrhoids are attached to the rectum by muscle fibers. If the nodes “crawl” out, this is already the second stage. Not the worst, because the muscles are still quite functional and easily “pull” the knots inward. Sometimes you can see traces of blood on toilet paper. Here we should be wary, but if there is no pain (or it goes away quickly), our person “moves on with life,” that is, he approaches the third stage, when prolapsed nodes can be adjusted only with his hands. At this stage, nodes can “pop out” even from minimal physical exertion. Doctors believe that in the third stage you need to literally run to the clinic. But they usually run on the fourth, when the muscles finally lose their elasticity and the hemorrhoids can no longer be removed inside - they are on the outside in the form of an inflamed bunch of grapes. At the same time, terrible pain is felt, such that it is impossible to touch even toilet paper.
Give life without hemorrhoids!
Hemorrhoids have a direct bearing on quality of life. When the anus - in the figurative expression of surgeons - is “full of bad teeth,” such a life can hardly be called high-quality. With proper treatment, hemorrhoids disappear within a week. Don't be afraid to go to the doctor with severe pain. Firstly, during the examination you will definitely be given anesthesia. Secondly, the doctor will definitely tell you the appropriate painkiller - tablets, ointments or suppositories. Our Center has everything necessary for a comprehensive examination and treatment of many proctological diseases, including hemorrhoids. To treat this “insidious” disease, both surgical treatment methods followed by the patient’s hospital stay, and radical minimally invasive techniques are used. The latter are good because they are highly effective in the treatment of internal hemorrhoids, they rarely cause complications, are well tolerated by patients, and do not require general anesthesia or hospitalization. In principle, in most cases, they are an alternative to the surgical method.