“People simply cannot afford to continue to be deprived of microbial diversity, which is already rapidly declining, in part due to antibiotic overuse.”
M. Blazer “When there are not enough microbes”
According to scientists, more than 100 trillion microorganisms, represented by bacteria, fungi, viruses and protozoa, live inside and outside the human body. They form colonies in areas such as the skin, respiratory system, eyes, oral cavity, urogenital and gastrointestinal tract. In each of these areas, microorganisms are organized into communities called the microbiota* or microflora of that area. The composition of the microbiota is individual, almost like fingerprints. It is determined by genetic predisposition and microorganisms received in childhood from the mother and from the environment and can change throughout life under the influence of external and internal factors.
*Microbiota is a community of microorganisms united by a certain area of habitat in the human body, with an established composition and ways of interacting with each other and with the host organism.
For a long time, humanity treated bacteria only as causative agents of dangerous diseases, but over time it came to the understanding that bacteria that permanently reside in the human body not only do not cause harm, but can also be useful to humans. The study of microflora and its connections with various diseases is still ongoing and is one of the most popular topics of scientific research at present.
What is dysbiosis
A child is born sterile; there are normally no bacteria in his body. The intestines and skin are colonized gradually, starting from the first attachment of the baby to the breast. The older the child gets and the more varied his food, the more different bacteria enter the intestines and form its microflora. In adults, the composition of microorganisms stabilizes, but becomes diverse. It can be compared to a fingerprint; despite the similarities, it is not repeated in any person.
Among intestinal bacteria, there are hundreds of types of good microorganisms, but normally there are also bad ones, the growth of which the body can restrain. There are three types of microbes:
- dominant - present in all healthy people, these include eubacteria, bacteroides, bifidobacteria, lactobacilli;
- non-permanent species - not found in everyone or under certain conditions, these are streptococci, Escherichia coli, Proteus, Cytobacter;
- transient species - sometimes enter the intestines, but do not stay there for a long time; these are types such as yeast fungi, clostridia, and Pseudomonas aeruginosa.
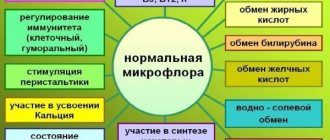
Good microorganisms are the dominant bacteria, they should be the majority. Thanks to the presence of normal microflora, food is digested. Bacteria help ferment some indigestible foods and participate in the absorption of vitamins, amino acids, and sugars. They themselves also synthesize vitamins B, K, and fatty acids. Therefore, with dysbacteriosis, signs of hypovitaminosis appear.
Good bacteria act as human shields. They form a protective layer on the intestinal wall, which does not allow pathogenic microorganisms to attach and limits their supply of nutrients. The immune function is to train immune cells and regulate its response to the penetration of foreign microorganisms or proteins.
But with a change in the ratio of bacteria, an increase in the number of transient species, and the appearance of yeast fungi, dysbacteriosis develops. It cannot be called a disease, but a person’s well-being is impaired. With dysbacteriosis, there are no pathogenic microorganisms in the intestines (Salmonella, Vibrio cholerae, Yersinia, pathogenic Escherichia, as well as viruses). Changes in composition occur due to an imbalance of normal flora and an increase in the concentration of opportunistic bacteria and the appearance of fungi.
How does the disease manifest in children?
Dysbacteriosis in children occurs in the same way as in adults. First of all, diarrhea or constipation occurs (sometimes alternating between them). The intestines experience colic and bloating, belching and bad breath. After eating, there is a feeling of fullness in the stomach. Often the syndrome occurs in the form of thrush in the mouth and skin lesions. A lack of vitamins and nutrients in the body contributes to the formation of congestion in the corners of the mouth. Due to decreased immunity, furunculosis, acne, and hair loss may occur.
Causes
The intestinal microflora in adults is in a state of dynamic equilibrium. It contains certain bacteria, which make up the majority, and about 3% of microorganisms that change their composition. Normally, fluctuations occur under the influence of food and eating habits. The microflora is affected by the predominance of sweets and fatty foods in the diet or predominantly plant foods.
Research shows that fatty foods inhibit bifidobacteria and enterococci, but under these conditions bacteroides multiply. A predominantly carbohydrate diet stimulates the proliferation of bifidobacteria and the total number of microorganisms. But these changes are temporary and do not lead to the appearance of symptoms of dysbiosis. They disappear on their own after a change in diet.
Intestinal dysbiosis in adults appears as a result of other diseases. The main causes of microflora disturbance are:
- long-term treatment with antibiotics;
- pathologies of the overlying parts of the digestive tract;
- long-term mono-diets and constant poor nutrition;
- intestinal infections.
Broad-spectrum antibiotics act nonselectively. They inhibit the growth or cause the death of all microorganisms. The longer the course of treatment, the higher the likelihood that dysbiosis will develop after it. Tetracycline antibiotics are especially dangerous. They significantly inhibit the proliferation of intestinal microflora, which leads to hypovitaminosis B, K, and an increased risk of bleeding.
Gastritis, cholecystitis, pancreatitis, hepatitis or biliary dyskinesia can lead to the development of dysbiosis. Cirrhosis of the liver, tumor processes in the stomach or ulcers are dangerous. These pathologies are accompanied by impaired digestion of food and enzyme production. Therefore, food enters the intestines insufficiently processed and cannot serve as a breeding ground for bacteria. Some of them die, and a seemingly pathogenic flora takes their place.
A fasting day, when the diet is based on the consumption of one food product, does not harm the body. But a mono-diet that lasts several weeks or becomes a way of life can lead to dysbiosis. Constant consumption of food containing simple carbohydrates and animal fats is dangerous. These are sweet, flour, fast food dishes. Such a diet inhibits the reproduction of normal flora, fermentation processes are activated in the intestines, and a large number of yeast fungi appear.
Food infections cause double damage to the intestines. They damage the mucous membrane, and antibiotic treatment kills beneficial bacteria. Therefore, recovery from illness is especially difficult.
Smoking has a negative effect on the condition of the intestines. It creates conditions for the proliferation of yeast, so smokers often suffer from unpleasant symptoms.
Factors causing intestinal dysbiosis:
- stress, decreased immunity;
- unnecessary use of antibiotics;
- chronic diseases of the gastrointestinal tract;
- food poisoning;
- intestinal infections;
- alcohol abuse (alcohol metabolism products lead to the death of microorganisms);
- consumption of food containing preservatives, herbicides and other foreign substances;
- unhealthy diet (frequent use of diets should also be included in this category).
Symptoms of dysbiosis
There are no strict symptoms that most likely indicate dysbiosis. Manifestations of pathology often do not correspond to the severity of the disorders. The most common symptom is indigestion such as intestinal dyspepsia. It manifests itself with the following symptoms:
- rumbling in the stomach;
- flatulence, increased gas formation;
- bloating;
- stool disorders;
- the appearance of pathological impurities in the stool.
Increased gas formation at the initial stage occurs after a nutritional disorder. If on a certain day the diet included milk, legumes, a large amount of flour and sweets, the symptoms appear clearly.
Stool disorders are variable. Most often, dysbiosis manifests itself as diarrhea. It may be accompanied by cramps and abdominal pain. Sometimes unformed stool appears only once a day, so it does not meet the criterion of diarrhea.
Diarrhea may alternate with constipation. This process is observed in people who limit the amount of fiber and dietary fiber in their diet. This deprives the bacteria of essential nutrients and prevents them from retaining water in the intestinal lumen. Mucous pathological impurities in the stool and abdominal pain appear with advanced forms of dysbacteriosis.
Violation of the microflora composition leads to vitamin deficiency. If it is not compensated by nutrition or taking multivitamin preparations, symptoms of hypovitaminosis appear:
- the condition of hair and nails worsens;
- rashes appear on the skin;
- allergic reactions or food intolerance appear;
- fatigue increases, performance decreases;
- sleep is disturbed.
Intestinal microorganisms synthesize vitamin K, which is involved in blood clotting. With hypovitaminosis, the appearance of bruises and hematomas under the skin from slight mechanical impact becomes more frequent. With a stomach ulcer or minor injuries, the risk of prolonged bleeding increases.
In severe cases, dysbiosis, which is accompanied by diarrhea, leads to dehydration. Many patients experience weight loss.
What examination is needed
Symptoms of dysbacteriosis are nonspecific. The same symptoms may mask pathology of the digestive system or hypovitaminosis. Therefore, dysbiosis is considered a clinical and laboratory syndrome.
Diagnosis begins with a scatological examination, which allows you to assess digestive function, the state of enzyme systems, peristalsis and the speed of movement of the food bolus.
But a change in the composition of feces does not indicate dysbacteriosis. It is necessary to confirm changes in the composition of bacteria in the intestinal lumen. In Moscow, many clinics use gas-liquid and ion chromatography methods. They make it possible to determine the composition of the microflora based on the resulting metabolites.
Bacteriological testing is often used. To do this, swabs from the intestinal mucosa, feces or scrapings are sown on special nutrient media. This method allows you to obtain colonies of bacteria and determine their type with high accuracy. A special stool test for dysbacteriosis is also used. But a mandatory condition is that the biological material must reach the laboratory no later than an hour after it is received from the patient. Feces must be kept warm so as not to cause the death of bacteria. The method does not justify itself by providing an idea only of the state of the colon flora.
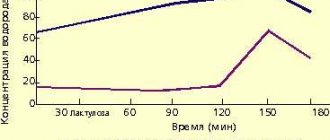
The gold standard for diagnosing dysbacteriosis is intestinoscopy. This is an endoscopic method during which a flexible probe with a video camera is inserted into the cavity of the small intestine through the mouth and stomach or rectum and colon. It is necessary to examine the intestinal mucosa and obtain an aspirate of its contents. The resulting liquid is also inoculated onto a nutrient medium. The disadvantage of this method is the need for general anesthesia, special bacteriological media and a long wait for the result. Sometimes a breath test with labeled H2 is used to diagnose dysbiosis.
Drugs and their action
The most effective way to restore microflora and get rid of dysbiosis is to use drugs from the group of probiotics. Manufacturers offer medicines in different forms:
- capsules;
- pills;
- powder;
- drops;
- solution.
The dosage form is selected by the doctor depending on the age of the patient. Children and elderly people who have difficulty swallowing tablets are prescribed a solution or powder for its preparation. At the age of 0-3 years, it is easier to give probiotic drops to a child. For everyone else, capsules or tablets are recommended.
Anti-dysbacteriosis medications are medications that can be purchased without a doctor's prescription. But self-medication is not recommended; only a specialist can tell you which type is best to take.
Probiotics usually contain 1-2 types of bacteria that restore mucous membranes well. Usually these are lacto- and bifidobacteria. They are normal inhabitants of the intestines that help improve microbial balance. The mechanism of action of this therapeutic group is associated with suppression of the growth of pathogenic flora. Lactic acid bacteria compete for receptors on the mucosal epithelium and nutrients. They secrete lactic acid and cytokines, which have an inhibitory effect on pathogens.
Preparations from the group of prebiotics help to effectively cure dysbiosis. These are medications that belong to the group of dietary fibers: inulin and lactulose, as well as drugs based on them.
They are not broken down by digestive enzymes and enter unchanged into the large intestine, where they become a nutrient substrate for lacto- and bifidobacteria. Therefore, microbes multiply well, increase the volume of bacterial mass, and restore the intestinal wall. To make the treatment as effective as possible, it is recommended to take prebiotics and probiotics at the same time.
Treatment of dysbiosis is not contraindicated in case of concomitant pathologies of the digestive tract. Probiotics are not harmful to patients with stomach ulcers, liver disease, or gallbladder disease. And in some cases they will speed up recovery.
In advanced cases of intestinal dysbiosis and when the symptoms of dyspepsia are too painful, medications from the group of enzymes can help. They should be selected by a doctor, depending on the type of digestive disorder. These medications must be taken daily before meals.
It’s hard to say how long it will take to treat dysbacteriosis. In some cases, this can last for several weeks, and in advanced cases – several months.
Treatment
At the initial stage of development of an imbalance of intestinal microflora, correcting the diet in favor of fresh vegetables and fruits, as well as fermented milk products, helps improve the general condition and stimulate the growth of beneficial bacteria. Complex treatment of dysbiosis includes the following points:
- Compliance with dietary recommendations (table number 4 according to Pevzner).
- Pathogenetic treatment, including the use of enzymatic drugs, laxatives and anti-inflammatory medications.
- Immunostimulating therapy.
- Taking enterosorbents to remove waste products of pathogenic microorganisms.
The drug Stimbifide Plus helps with intestinal dysbiosis, containing highly purified fructopolysaccharides necessary for the growth and reproduction of beneficial intestinal microflora. The drug also contains a vitamin complex that has anti-inflammatory and antioxidant effects.
Also, the drug activates intestinal immunity and has a detrimental effect on the bacterium Helicobacter pylori, which is the main cause of gastric ulcer development. At least 95% of those who completed the course of using the drug Stimbifid Plus noted an improvement in their general condition, complete disappearance of symptoms of microflora imbalance and normalization of digestion.