Doctors Cost
Price list Doctors clinic
Dysbacteriosis is not an independent disease, but a consequence of certain factors. It is characterized by an imbalance of microorganisms in the intestines.
Beneficial bacteria are found throughout the human body, and there are especially many of them in the intestines. Their ratio can be individual for each specific person. The optimal set of bacteria is called eubiosis, or intestinal biocenosis. Dysbacteriosis can be characterized by a violation of the composition, a decrease in the number of beneficial bacteria, or a change in their properties.
A decrease in the number of beneficial microorganisms is caused by a whole range of reasons. Treatment of dysbiosis should include an analysis of factors that could lead to disruption of the natural balance.
What kind of remedy is Bifidumbacterin?
The drug is a microbial substance that contains colonies of living bifidocultures that populate the intestinal lumen. For better action, the medicine contains lactose - the “food” of bacteria, thanks to which they quickly multiply in the body. The medicine is intended to eliminate digestive pathologies and eliminate intoxications.
The tool has several forms:
- dry preparation in powder: white, packaged in portioned sachets;
- capsules;
- vaginal suppositories;
- liquid concentrate in ampoules or vials;
- Bifidumbacterin 1000: in tablet form.
The drug package contains from 1 to 5 doses.
Symptoms and signs of dysbiosis in children
It is usually quite simple to recognize that a child has problems with the digestive system; they are visible even if the baby does not speak yet.
- Irregular bowel movements, diarrhea, or, conversely, constipation.
- Bloating, gas.
- The child complains of abdominal pain, long-lasting, viscous.
- Often, dysbiosis can manifest itself in the form of rashes and itching.
If you suspect dysbiosis, do not self-medicate; it is best to get tested. Doctors will be able to determine which bacteria are missing and prescribe the necessary medications, usually of a probiotic nature.
When is Bifidumbacterin used?
It is recommended to use the drug:
- with dysbacteriosis;
- acute intestinal infections;
- malabsorption of nutrients;
- inflammatory processes in the intestines;
- dysfunctions due to taking antibiotics;
- for the prevention of dysbiosis in infants when changing the type of diet;
- for the prevention of mastitis in women.
In complex therapy, the medicine is prescribed for sepsis, pneumonia, and gynecological inflammation.
How to use Bifidumbacterin powder
The dry preparation should be taken orally. Adults, depending on the condition, require from 1 to 5 doses of the drug per dose up to three times a day.
- The contents of the package must first be diluted with several tablespoons of warm water: about 5 ml per dose.
- Stir for 2-3 minutes and drink.
- To improve the effect, it is recommended to increase the proportion of dairy products and vegetables in the diet.
The prepared solution cannot be stored; it must be used immediately. Course of continuous treatment: from 2 to 12 weeks.
INTESTINAL DYSBACTERIOSIS
What is meant by dysbiosis? What diagnostic methods are modern and reliable? What medications are used for dysbiosis?
The human intestine contains over 500 different types of microbes, the total number of which reaches 1014, which is an order of magnitude higher than the total number of cellular composition of the human body. The number of microorganisms increases in the distal direction, and in the colon 1 g of feces contains 1011 bacteria, which constitutes 30% of the dry residue of the intestinal contents.
Normal intestinal microbial flora
In the jejunum of healthy people there are up to 105 bacteria per 1 ml of intestinal contents. The bulk of these bacteria are streptococci, staphylococci, lactic acid bacilli, other gram-positive aerobic bacteria and fungi. In the distal ileum, the number of microbes increases to 107–108, primarily due to enterococci, Escherichia coli, bacteroides and anaerobic bacteria. We recently found that the concentration of the parietal microflora of the jejunum is 6 orders of magnitude higher than in its cavity, and amounts to 1011 cells/ml. About 50% of the biomass of the parietal microflora are actinomycetes, approximately 25% are aerobic cocci (staphylococci, streptococci, enterococci and coryneform bacteria), from 20 to 30% are bifidobacteria and lactobacilli.
The number of anaerobes (peptostreptococci, bacteroides, clostridia, propionobacteria) is about 10% in the small intestine and up to 20% in the large intestine. Enterobacteriaceae account for 1% of the total microflora of the mucous membrane.
Up to 90-95% of microbes in the large intestine are anaerobes (bifidobacteria and bacteroides), and only 5-10% of all bacteria are strictly aerobic and facultative flora (lactic acid and E. coli, enterococci, staphylococci, fungi, proteus).
Escherichia coli, enterococci, bifidobacteria and acidophilus bacilli have pronounced antagonistic properties. Under conditions of a normally functioning intestine, they are able to suppress the growth of microorganisms unusual for normal microflora.
The internal surface area of the intestine is about 200 m2. It is reliably protected from the penetration of food antigens, microbes and viruses. The body's immune system plays an important role in organizing this defense. About 85% of human lymphatic tissue is concentrated in the intestinal wall, where secretory IgA is produced. Intestinal microflora stimulates immune defense. Intestinal antigens and toxins from intestinal microbes significantly increase the secretion of IgA into the intestinal lumen.
The breakdown of undigested nutrients in the colon is carried out by bacterial enzymes, resulting in the formation of various amines, phenols, organic acids and other compounds. Toxic products of microbial metabolism (cadaverine, histamine and other amines) are excreted in the urine and normally have no effect on the body. When microbes utilize indigestible carbohydrates (fiber), short-chain fatty acids are formed. They provide intestinal cells with energy carriers and, therefore, improve the trophism of the mucous membrane. Fiber deficiency may impair the permeability of the intestinal barrier due to a deficiency of short-chain fatty acids. As a result, intestinal microbes can enter the bloodstream.
Under the influence of microbial enzymes in the distal ileum, bile acids are deconjugated and primary bile acids are converted into secondary ones. Under physiological conditions, 80 to 95% of bile acids are reabsorbed, the rest are excreted in feces in the form of bacterial metabolites. The latter contribute to the normal formation of feces: they inhibit the absorption of water and thereby prevent excessive dehydration of feces.
Dysbacteriosis
The concept of intestinal dysbiosis includes excessive microbial contamination of the small intestine and changes in the microbial composition of the large intestine. Disruption of microbiocenosis occurs to one degree or another in most patients with pathologies of the intestines and other digestive organs. Therefore, dysbiosis is a bacteriological concept. It can be considered as one of the manifestations or complication of the disease, but not an independent nosological form.
The extreme degree of intestinal dysbiosis is the appearance of gastrointestinal bacteria in the blood (bacteremia) or even the development of sepsis.
The composition of the intestinal microflora is disrupted by diseases of the intestines and other digestive organs, treatment with antibiotics and immunosuppressants, and exposure to harmful environmental factors.
Clinical manifestations of dysbiosis depend on the localization of dysbiotic changes.
Dysbacteriosis of the small intestine
With dysbiosis of the small intestine, the number of some microbes in the mucous membrane of the small intestine is increased, while others are decreased. There is an increase in Eubacterium (30 times), α-streptococci (25 times), enterococci (10 times), Candida (15 times), the appearance of bacteria of the genus Acinetobacter and herpes viruses. The number of most anaerobes, actinomycetes, Klebsiella and other microorganisms that are natural inhabitants of the intestines decreases from 2 to 30 times.
The cause of dysbacteriosis can be: a) excessive entry of microorganisms into the small intestine during achylia and dysfunction of the ileocecal valve; b) favorable conditions for the development of pathological microorganisms in cases of impaired intestinal digestion and absorption, development of immunodeficiency and intestinal obstruction.
Increased proliferation of microbes in the small intestine leads to premature deconjugation of bile acids and their loss in feces. An excess of bile acids increases colon motility and causes diarrhea and steatorrhea, and a deficiency of bile acids leads to impaired absorption of fat-soluble vitamins and the development of cholelithiasis.
Bacterial toxins and metabolites, such as phenols and biogenic amines, can bind vitamin B12.
Some microorganisms have a cytotoxic effect and damage the epithelium of the small intestine. This leads to a decrease in the height of the villi and deepening of the crypts. Electron microscopy reveals degeneration of microvilli, mitochondria and endoplasmic reticulum.
Colon dysbiosis
The composition of the microflora of the colon can change under the influence of various factors and adverse effects that weaken the body’s defense mechanisms (extreme climatic and geographical conditions, pollution of the biosphere with industrial waste and various chemicals, infectious diseases, diseases of the digestive system, malnutrition, ionizing radiation).
Iatrogenic factors play an important role in the development of colon dysbiosis: the use of antibiotics and sulfonamides, immunosuppressants, steroid hormones, radiotherapy, and surgical interventions. Antibacterial drugs significantly suppress not only pathogenic microbial flora, but also the growth of normal microflora in the colon. As a result, microbes that come from outside or endogenous species that are resistant to drugs (staphylococci, Proteus, yeast, enterococci, Pseudomonas aeruginosa) multiply.
Clinical features of dysbiosis
Clinical manifestations of excessive growth of microorganisms in the small intestine may be completely absent, act as one of the pathogenetic factors of chronic recurrent diarrhea, and in some diseases, for example, diverticulosis of the small intestine, partial intestinal obstruction or after surgical operations on the stomach and intestines, lead to severe diarrhea , steatorrhea and B12-deficiency anemia.
The features of the clinical course of the disease in patients with various variants of colon dysbiosis, according to bacteriological analyzes of stool, in most cases cannot be established. It can be noted that patients with chronic intestinal diseases are more often infected with acute intestinal infections compared to healthy people. This is probably due to a decrease in the antagonistic properties of normal intestinal microflora and, above all, the frequent absence of bifidobacteria.
Particularly dangerous is pseudomembranous colitis, which develops in some patients who have been treated with broad-spectrum antibiotics for a long time. This severe variant of dysbiosis is caused by toxins secreted by Pseudomonas aeruginosa Clostridium difficile, which multiplies in the intestines when the normal microbial flora is suppressed.
The main symptom of pseudomembranous colitis is profuse, watery diarrhea, the onset of which was preceded by the prescription of antibiotics. Then cramping pain in the abdomen appears, body temperature rises, and leukocytosis increases in the blood. The endoscopic picture of pseudomembranous colitis is characterized by the presence of plaque-like, ribbon-like and solid “membranes”, soft but tightly fused to the mucous membrane. The changes are most pronounced in the distal parts of the colon and rectum. The mucous membrane is edematous, but not ulcerated. Histological examination reveals subepithelial edema with round cell infiltration of the lamina propria, capillary stasis with the release of red blood cells outside the vessels. At the stage of formation of pseudomembranes under the surface epithelium of the mucous membrane, exudative infiltrates appear. The epithelial layer is raised and absent in places; bare areas of the mucous membrane are covered only by desquamated epithelium. In later stages of the disease, these areas may occupy large segments of the intestine.
Very rarely, a fulminant course of pseudomembranous colitis, reminiscent of cholera, is observed. Dehydration develops within a few hours and ends in death.
Thus, assessment of the clinical significance of dysbiotic changes should be based primarily on clinical manifestations, and not only on the results of a study of fecal microflora.
Diagnostic methods
Diagnosis of dysbiosis is a complex and time-consuming task. To diagnose small intestinal dysbiosis, culture of small intestinal juice obtained using a sterile probe is used. Dysbacteriosis of the colon is detected using bacteriological studies of stool.
Microbial flora produces a large amount of gases, including hydrogen. This phenomenon is used to diagnose dysbiosis. The concentration of hydrogen in exhaled air on an empty stomach is directly dependent on the severity of bacterial contamination of the small intestine. In patients with intestinal diseases occurring with chronic recurrent diarrhea and bacterial contamination of the small intestine, the concentration of hydrogen in exhaled air significantly exceeds 15 ppm.
To diagnose dysbiosis, a lactulose load is also used. Normally, lactulose is not broken down in the small intestine and is metabolized by the microbial flora of the colon. As a result, the amount of hydrogen in the exhaled air increases (Fig. 1).
| Figure 1. Hydrogen concentration in exhaled air |
The most common bacteriological signs of colon dysbiosis are the absence of the main bacterial symbionts - bifidobacteria and a decrease in the number of lactic acid bacilli. The number of E. coli, enterococci, clostridia, staphylococci, yeast-like fungi and Proteus increases. Some bacterial symbionts develop pathological forms. These include hemolyzing flora, E. coli with weakly expressed enzymatic properties, enteropathogenic E. coli, etc.
An in-depth study of microbiocenosis has shown that traditional methods do not provide true information about the state of the intestinal microflora. Of the 500 known species of microbes, only 10-20 microorganisms are usually studied for diagnostic purposes. It is important in which part - in the jejunum, ileum or colon - the microbial composition is studied. Therefore, the prospects for developing clinical problems of dysbiosis are currently associated with the use of chemical methods for differentiating microorganisms, which make it possible to obtain universal information about the state of microbiocenosis. The most widely used for these purposes are gas chromatography (GC) and gas chromatography coupled with mass spectrometry (GC-MS). This method allows one to obtain unique information about the composition of the monomeric chemical components of the microbial cell and metabolites. Markers of this kind can be determined and used to detect microorganisms. The main advantage and fundamental difference of this method from bacteriological ones is the possibility of quantitative determination of more than 170 taxa of clinically significant microorganisms in various environments of the body. In this case, the results of the study can be obtained within a few hours.
Our studies of microbiocenosis in the blood and biopsy samples of the mucous membrane of the small and large intestines in patients with irritable bowel syndrome allowed us to detect deviations from the norm up to a 30-fold increase or decrease in many components.
It is possible to assess changes in intestinal microflora based on blood analysis data using GC-MS microbial markers. Treatment regimen for intestinal dysbiosis
Treatment
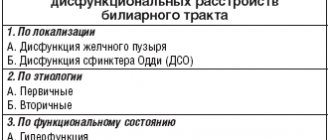
Treatment of dysbacteriosis should be comprehensive (scheme) and include the following measures:
- elimination of excessive bacterial contamination of the small intestine;
- restoration of normal microbial flora of the colon;
- improvement of intestinal digestion and absorption;
- restoration of impaired intestinal motility;
- stimulating the body's reactivity.
Antibacterial drugs
Antibacterial drugs are necessary primarily to suppress the excessive growth of microbial flora in the small intestine. The most widely used antibiotics are from the group of tetracyclines, penicillins, cephalosporins, quinolones (tarivid, nitroxoline) and metronidazole.
However, broad-spectrum antibiotics significantly disrupt eubiosis in the colon. Therefore, they should be used only for diseases accompanied by disorders of absorption and intestinal motility, in which, as a rule, there is a pronounced growth of microbial flora in the lumen of the small intestine.
Antibiotics are prescribed orally in normal doses for 7–10 days.
For diseases accompanied by colon dysbiosis, treatment is best carried out with drugs that have a minimal effect on the symbiont microbial flora and suppress the growth of Proteus, staphylococci, yeast fungi and other aggressive strains of microbes. These include antiseptics: intetrix, ersefuril, nitroxoline, furazolidone, etc.
For severe forms of staphylococcal dysbiosis, antibiotics are used: tarivid, palin, metronidazole (Trichopol), as well as biseptol-480, nevigramon.
Antibacterial drugs are prescribed for 10–14 days. If fungi appear in the stool or intestinal juice, the use of nystatin or levorin is indicated.
In all patients with diarrhea associated with antibiotics, occurring with intoxication and leukocytosis, the occurrence of acute diarrhea should be associated with Cl. difficile.
In this case, an urgent stool culture is done for Cl. difficile and prescribe vancomycin 125 mg orally 4 times a day; if necessary, the dose can be increased to 500 mg 4 times a day. Treatment is continued for 7-10 days. Metronidazole at a dose of 500 mg orally 2 times a day, bacitracin 25,000 IU orally 4 times a day are also effective. Bacitracin is almost not absorbed, and therefore a higher concentration of the drug can be created in the colon. In case of dehydration, adequate infusion therapy is used to correct the water and electrolyte balance. To bind the toxin Cl. difficile use cholestyramine (Questran).
Bacterial preparations
Live cultures of normal microbial flora survive in the human intestine from 1 to 10% of the total dose and are capable, to some extent, of performing the physiological function of normal microbial flora. Bacterial drugs can be prescribed without prior antibacterial therapy or after it. Bifidumbacterin, bificol, lactobacterin, bactisubtil, linex, enterol, etc. are used. The course of treatment lasts 1-2 months.
Another possible way to eliminate dysbiosis is to influence the pathogenic microbial flora with metabolic products of normal microorganisms. Such drugs include Hilak Forte. It was created 50 years ago and is still used to treat patients with intestinal pathologies. Hilak forte is a sterile concentrate of metabolic products of normal intestinal microflora: lactic acid, lactose, amino acids and fatty acids. These substances help restore the biological environment in the intestines necessary for the existence of normal microflora and suppress the growth of pathogenic bacteria. Perhaps metabolic products improve the trophism and function of epithelial cells and colonocytes. 1 ml of the drug corresponds to the biosynthetic active substances of 100 billion normal microorganisms. Hilak forte is prescribed 40–60 drops 3 times a day for up to 4 weeks in combination with antibacterial drugs or after their use.
More recently, there have been reports of the possibility of treating acute diarrhea associated with antibiotic therapy and Cl. difficile, large doses of pre- and probiotics.
Regulators of digestion and intestinal motility
In patients with impaired cavity digestion, Creon, pancitrate and other pancreatic enzymes are used. In order to improve the absorption function, Essentiale, Legalon or Karsil are prescribed, since they stabilize the membranes of the intestinal epithelium. Propulsive bowel function is improved by imodium (loperamide) and trimebutine (debridate).
Stimulants of body reactivity
To increase the reactivity of the body in weakened patients, it is advisable to use taktivin, thymalin, thymogen, immunal, immunofan and other immunostimulating agents. The course of treatment should average 4 weeks. Vitamins are prescribed at the same time.
Prevention of dysbacteriosis
Primary prevention of dysbiosis is a very difficult task. Its solution is associated with general preventive problems: improving the environment, rational nutrition, improving well-being and other numerous factors of the external and internal environment.
Secondary prevention involves the rational use of antibiotics and other medications that disrupt eubiosis, timely and optimal treatment of diseases of the digestive system, accompanied by a violation of microbiocenosis.