Why does pain occur?
Discomfort in the epigastric region during breastfeeding can occur for a number of reasons:
- stressful state. The experiences of a nursing mother can provoke excessive production of gastric juice, which includes hydrochloric acid. It is this acid that has an irritating effect on the condition of the mucous membrane, which is fraught with the development of an inflammatory reaction and the appearance of pain;
- prolapse of the stomach. During pregnancy, due to the growing uterus, the organs are slightly displaced, and after childbirth the condition may worsen further. This change causes pain;
- exacerbation of chronic diseases of the digestive system: gastritis, gastroduodenitis, cholecystitis, pancreatitis;
- muscle pain. Difficult labor can cause muscle pain, which can easily be confused with stomach pain;
- convulsions. They are also called postpartum contractions, which occur due to decreased blood flow to the uterus;
- eating disorder. Limiting certain foods and increasing others can lead to digestive problems.
In some cases, discomfort in the stomach area is associated with disorders of other organs and systems: inflammation of the kidneys and adrenal glands, pleurisy, intervertebral hernia, metritis, inflammation of the small intestine.
Stomach pain in a nursing mother may be the result of overeating
Breastfeeding is very important!
Breast milk has been and remains the best nutrition for a newborn. No milk formula, even the highest quality, can fully replace it. Because it is with breast milk that your baby receives the full amount of nutrients, microelements and vitamins necessary for the full growth and development of this particular child. Moreover, in the form and proportions determined by Mother Nature herself. However, in some cases and depending on a number of circumstances, the quality indicators of human milk may change, and not for the better. This, of course, can cause harm to the baby, who will simply be “malnourished,” that is, not receive enough components that are extremely necessary for his growing body.
Symptoms
First, let's highlight the symptoms that require emergency medical attention:
- redness around the suture after cesarean section;
- nausea;
- fever;
- intense pain;
- bleeding.
The following symptoms indicate disorders of the digestive tract: discomfort, heaviness, vomiting, heartburn, belching, constipation or diarrhea, weakness, malaise, change in appetite. The specialist evaluates all these symptoms, as well as the nature of the pain.
Contact a specialist
If you feel unwell, the first thing you should do is assess your condition.
If your health has really deteriorated, be sure to consult a doctor. Not all diseases can go away on their own, without medical help.
When consulting with your doctor, tell him or her that you are breastfeeding. Unfortunately, many medications (except most homeopathic ones) are incompatible with feeding. Even proven and well-known medicines for colds or headaches during breastfeeding may be prohibited. In this case, you will have to switch to artificial feeding for the duration of treatment. In this case, you should definitely check with a specialist how long after stopping the medication you can return to breastfeeding.
Diseases that cause stomach pain in a nursing mother
Why does my stomach hurt when breastfeeding? The doctor will be able to answer this question after the examination. Let's talk about the most common diseases that provoke discomfort.
Gastroptosis
Stomach prolapse causes aching or dull pain in the epigastrium. Typically, discomfort occurs after eating and goes away while lying down. Sometimes pain occurs in the lumbar region. Eating food provokes bloating and heaviness in the stomach, nausea and belching.
Appetite also decreases, weakness, increased fatigue and irritability appear. Gastroptosis causes headaches and dizziness.
Physical therapy strengthens the ligamentous apparatus, which is responsible for holding the stomach in place. A woman is recommended to do gymnastics or swimming. A special role in the treatment of prolapse is played by breathing exercises, which should be carried out under the supervision of a specialist. Folk methods are also used as auxiliary therapy, for example, infusion of yarrow and wormwood.
Cholecystitis
Inflammation of the gallbladder causes a dull pain on the right side, which radiates to the shoulder blade and arm. Women complain of belching with a bitter taste, nausea and vomiting, general malaise, fatigue, drowsiness, and fever.
With cholecystitis, it is extremely important for a woman to follow a strict diet. In difficult cases, a two-day fast is prescribed. In the future, it is important to eat smaller meals. Food is best cooked steamed or stewed and baked. Food should be taken warm; cold foods will only increase discomfort. Compliance with the drinking regime plays an important role.
Abdominal pain during breastfeeding may occur due to inflammation of the gallbladder
Gastritis
Gastric pain has a pulling, cramping character. Women are also concerned about nausea, vomiting, belching, heartburn, and upset bowel movements. In some cases, the doctor may recommend interrupting feeding. If the pain is moderate and does not affect the general condition of the woman, then in this case the problem can be eliminated without interrupting feeding.
With gastritis, a woman is recommended to eat food that envelops the gastric mucosa and does not irritate the organ. During the inflammatory process, you should eat oatmeal with water, buckwheat porridge, jelly, vegetable stew, etc. Mineral waters can normalize the acidity of the stomach. For high acidity, it is recommended to take Borjomi; for low acidity, Essentuki.
Pancreatitis
Pain in the upper abdomen due to inflammation of the pancreas is burning and bursting in nature, which is simply unbearable to endure. Vomiting does not bring relief. Remnants of undigested food appear in diarrhea. The general condition of the woman is disturbed, the body temperature rises.
On the first day, a woman should fast. To relieve pain, cold is applied to the upper abdomen. Antispasmodics are prescribed to relieve pain.
What determines the quality of breast milk?
There are many stereotypes and even superstitions about this. Often, nursing mothers hear from more “experienced” relatives and friends that in order to increase the fat content of milk, you need to eat more, consume more dairy products with a high percentage of fat, and lean on sweets and nuts. It is believed that consuming large quantities of a wide variety of high-calorie foods (fatty meat or sausages) can give lactation an additional “impulse” of quality. In everyday life you can often hear the expression “poor milk” , which characterizes milk that supposedly has low fat content and for this reason cannot be a complete nutrition for the baby (sometimes they say “blue milk”, in fact it is “forem” milk, which contains more water and immune factors, in contrast to the “back” - more fatty and high-calorie). There are also warnings: do not eat garlic and onions, which will supposedly give the milk a bitter taste and the child will refuse it. Breastfeeding mothers are also strongly advised to refrain from smoking, drinking alcohol, taking uncontrolled medications and... not getting carried away with coffee, since caffeine easily penetrates into milk.
Of the above tips and prohibitions, perhaps the most indisputable are the last ones - about the dangers of cigarettes, alcohol, coffee and medications . All other recommendations - in relation to the same sausages that are supposedly “nutritious” - are far-fetched. One comedian, by the way, noted that “not a single animal was harmed during the production of sausages.” Of course, he exaggerated, but there is a lot of truth in these words. It is well known that various ingredients are added to sausages that have nothing to do with real meat. In particular, preservatives and dyes, flavor enhancers and thickeners, etc., etc. Now imagine that this explosive mixture first enters the woman’s body, and then, having penetrated into the milk, into the child’s body. So is it worth consuming such products to improve lactation rates? The answer, I think, is obvious...
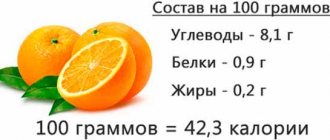
In fact, completely different factors influence the quality of breast milk . They have nothing to do with food (more precisely, they do, but indirectly - read about this below), and even more so to the amount of food eaten by the mother. Lactation occurs regardless of the quantity and quality of food a woman eats. Even if, hypothetically, she stops eating altogether, the process of producing breast milk will not stop. If the mother’s nutrition affects anything, it is, first of all, her own health. What stimulates breast milk production? It turns out that they are hormones, the production of which is especially activated when the baby suckles, stimulating the nipples. The nutritional value of milk - that is, its quality indicators - completely depends on the state of the woman’s body, her health, and hormonal levels. Culinary preferences have absolutely nothing to do with it.
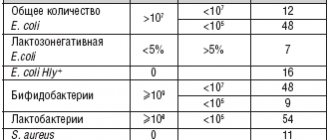
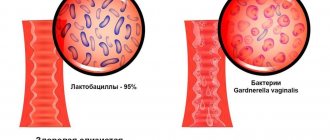
The quality and quantity of breast milk is influenced, among other things, by the timing of lactation (it is known that in the first two to three days after birth, highly nutritious colostrum is produced, then transitional milk, and only then mature milk), as well as the state of the microflora and the functions of food digestion in the body nursing mother. We will talk about the last factor in more detail today.
Lower abdomen hurts
The postpartum period is different for every woman. Sometimes pain appears in the lower abdomen, which can greatly frighten a woman. Brief and mild discomfort is considered normal. If the pain does not go away for a long time and brings unbearable discomfort, this cannot be tolerated.
Let's highlight the most common causes of pain in the lower abdomen:
- active production of oxytocin can cause cramping, nagging pain. The hormone stimulates the contractile function of the uterus so that the organ returns to its previous shape;
- Nipple irritation during lactation further stimulates the production of oxytocin. Active contraction of the uterus causes a new wave of pain;
- Remnants of the placenta in the uterus can provoke pain that does not subside within a month after birth. Adhering particles provoke the formation of blood clots and rotting. The problem can be solved with the help of surgery, along with which antibacterial therapy is prescribed;
- endometritis. Most often occurs after cesarean section. Surgery can cause infection to enter the uterus. In addition to pain, bloody discharge mixed with pus appears, and the temperature also rises. Comprehensive treatment will help cope with the inflammatory process, including the following drugs: antibacterial, desensitizing, detoxifying, restorative;
- salpingo-oophoritis. Inflammation of the appendages provokes nagging pain in the lower abdomen;
- peritonitis. Inflammation of the abdominal cavity causes unbearable pain and high fever;
- vertebral displacement. In this case, the pain radiates to the spine. Unpleasant sensations can bother a woman for a long period of time and intensify with physical activity.
Pain in the lower abdomen can be caused by inflammation of the appendages
Decreased wall immunity. How to fight?
Why is it that dysbiosis disrupts or significantly decreases the absorption of beneficial substances, while potentially dangerous substances, on the contrary, increase? The reason is a decrease or complete absence of parietal immunity in the intestine. To restore it to its previous level, a nursing mother needs to completely reconsider her diet, consuming more healthy foods: protein and lactic acid products, fruits, vegetables, etc. However, in a number of advanced cases this is clearly not enough and experts prescribe special preparations - probiotics containing live cultures of bifidobacteria and lactobacilli. They are produced by manufacturers in dry (lyophilized) and liquid form. Normoflorins are the most famous in our country and neighboring countries . Why, you ask? The fact is that during the production of liquid probiotics there is no loss and weakening of the active properties of beneficial microorganisms, while during drying these processes take place. For this reason, the effect of using dry probiotics does not appear immediately. Plus, it is less pronounced and short-lasting. , experts recommend liquid forms of probiotics for women suffering from dysbiosis during lactation Thanks to their rapid action, the balance of intestinal microflora and, accordingly, all digestive functions are just as quickly restored, including one of the most important - the absorption of all useful components of food.
Back to list Previous article Next article
Any doubts?
If you have the slightest doubt about whether you can take this or that medicine, consult a professional. Don't risk your child's health! Remember that you are not alone with the problem. You can get advice not only from your friends, but also from professionals - lactation consultants.
A mammologist at a clinic or a doctor at a antenatal clinic can give you contact information for such a consultant. Perhaps you were given the contact details of a breastfeeding consultant when you were in the maternity hospital.
You can ask for help at e-lactancia.org. This is the online directory of the Marina Alta Hospital "Compatibility of Breastfeeding with Pharmaceutical Drugs and other Products". APILAM (Association for the Promotion and Cultural and Scientific Research of Breastfeeding) is responsible for the information posted there. However, to use this resource it is advisable to know English.
In Russia there is an organization with similar goals - the Association of Consultants on Natural Feeding (AKEV). She has been working for about 10 years. Their website is located at: https://akev.info. Here you can also find the coordinates of specialists in your region.
A healthy pregnancy and the birth of a healthy baby is a reason for a woman to be proud of herself and her health. An important topic that concerns many women after childbirth is menstruation: when to expect it, why the cycle is irregular, is it possible to get pregnant while breastfeeding, and much more. Let's look at the main issues in our article.
Postpartum discharge
Postpartum heavy discharge in a woman has nothing to do with menstruation - it is lochia, which turns from bloody to bloody and then transparent, completely disappearing. After about two months, the uterus and ovaries return to their physiological state and size, which means that the onset of menstrual cycles with the maturation of eggs and menstruation is quite possible. Thus, a woman can expect her first period from the 2-3rd month after birth.
When should your period start after childbirth?
This period depends on the type of feeding the child: natural or artificial. Breast milk production occurs under the influence of the pituitary hormone prolactin. The level of estrogen does not increase, therefore, when breastfeeding, menstruation begins, on average, 2 months after birth, more often when feeding “by the hour.” But there are cases when some breastfeeding women do not get their periods for a year, and for some they can recover within a month and a half after giving birth. On average, the onset of menstruation during breastfeeding varies from 3 months to six months.
How long do periods last in the postpartum period?
Often the first menstruation is quite heavy. There may be heavy discharge, periods with blood clots. If you have to change the pad every hour, you should seek help from a doctor: this may be a symptom of bleeding. Subsequent periods usually become normal. In other cases, women experience irregular spotting in the first months. This is typical for breastfeeding, when prolactin synthesis gradually decreases.
Reasons for slow recovery of a regular cycle
Each woman has her own individual period for the restoration of the menstrual cycle. This is determined by the activity of the production of hormones by the sex glands, pituitary gland, and the state of the immune and reproductive systems as a whole. There are a number of reasons for this that affect the body in the postpartum period:
- features of individual hormonal levels;
- hereditary factors;
- the nature of the birth process;
- features of uterine restoration.
What to do if your menstrual cycle becomes irregular:
- In the first months of the postpartum recovery period, there is no need to panic. In most cases, this is the norm. For each woman, normalization of the cycle occurs individually, usually during the first months of the resumption of menstrual bleeding. Irregularity occurs more often in nursing mothers.
- It takes about 2 months to restore the normal function of all organs and systems. Balance in the endocrine system occurs later, especially if breastfeeding is used. Therefore, a woman can feel quite healthy, but she will not have menstruation.
- You should pay attention to an irregular cycle only after 3 cycles. This may be due to an inflammatory process, endometriosis or a tumor of the genital organs. A delay in your second period is not dangerous unless it is associated with another pregnancy.
Menstruation after cesarean section
Menstruation after a cesarean section is restored in the same way as after a normal birth. During lactation, periods do not come for six months. Against the background of artificial feeding from the maternity hospital, due to the lack of stimulation of the nipples (which activates the synthesis of oxytocin, which contracts the uterus), recovery may be somewhat slower, plus there is still a scar on the uterus. Therefore, restoration of menstrual function may occur a little later, by several weeks.
Cycle after pathological pregnancy or childbirth
After termination of a frozen pregnancy or abortion, the first menstruation occurs within 45 days. If this does not happen, the woman should seek help from a gynecologist. To exclude causes of amenorrhea, such as the remaining part of the fertilized egg in the uterus or inflammation, an ultrasound scan must be performed 10 days after the termination of a frozen or normal pregnancy.
Pathologies of menstruation, what to pay attention to and immediately contact a specialist:
- A sudden cessation of postpartum discharge is a sign of a bent uterus or endometritis, an accumulation of lochia in the uterine cavity - lochiometra.
- Scanty periods for 3 cycles or more. Perhaps they are a symptom of hormonal disorders, Sheehan syndrome or endometritis.
- Irregularity of menstruation six months after its restoration, a break between bleeding for more than 3 months. Most often accompanied by ovarian pathology.
- Excessive bleeding for 2 or more cycles, especially after surgical delivery or termination of pregnancy. They are often caused by the tissues of the membranes remaining on the walls of the uterus.
- The duration of menstruation is more than a week, which is accompanied by weakness and dizziness.
- The appearance of abdominal pain, fever, unpleasant odor, change in color of vaginal discharge is a sign of a tumor or infection.
- Spotting before and after menstruation is a likely symptom of endometriosis or an inflammatory disease.
- Itching in the vagina, an admixture of cheesy discharge is a sign of thrush.
- Bleeding twice a month for more than 3 cycles.
Is it possible to get pregnant?
The most common myth is that a woman cannot get pregnant if she is breastfeeding her baby. The fact is that the process of ovulation - the first after childbirth, is formed before the onset of the first spotting, and it is this process that, during unprotected intercourse, can lead to an unplanned pregnancy, and the woman will give birth the same age. If a woman does not breastfeed, you need to think about protection after childbirth right away, from the very first sexual intercourse, since the dynamics of restoration of reproductive functions are different for everyone; after 6-8 weeks from the moment of birth, the first ovulation is possible.
Remember that a long delay in menstruation after childbirth or a cycle failure are not always symptoms of dangerous disorders, but in any case it is not advisable to self-medicate. For any questions or problems arising with the reproductive system, please contact our specialists for advice.
read carefully
Use common sense when taking any medications. Carefully read the instructions for the drug, especially the “contraindications” section. It will definitely indicate whether the medicine can be taken while breastfeeding. If a specialist has prescribed the drug to you, and the instructions state that feeding is a contraindication, you should trust the instructions more, since doctors do not always remember by heart the subtleties of prescribing a particular drug and all the medications allowed for breastfeeding.