Co-author, editor and medical expert - Klimovich Elina Valerievna.
Number of views: 34 677
Last updated date: 12/20/2021
Average reading time: 3 minutes
Pain in the upper abdomen is perhaps one of the most common complaints with which patients consult a gastroenterologist. This is a rather complex symptom that can be triggered by a number of factors. It can be temporary or permanent and indicate the occurrence of a particular digestive tract problem that needs to be addressed.
Causes of pain in the upper abdomen after eating
Poor nutrition
Very often, the cause of abdominal pain after eating is nutritional errors. Failure to adhere to the daily routine, overeating, late dinner, dry food, rapid absorption of food, and low fluid intake during the day can lead to painful sensations. Also, fatty meat, dairy products, rough plant foods, brown bread, canned food, vegetable marinades, fructose, sorbitol, lutein and alcoholic beverages can trigger pain in the upper abdomen.
Food allergies
One type of food intolerance, leading to nausea, vomiting, pain in the stomach and upper abdomen, and various skin manifestations, is an allergy. The most powerful allergens include cow's milk, fish proteins, eggs, and seafood. Some vegetables, fruits and cereals (wheat and rye) can also provoke the development of an allergic reaction.
Digestive system diseases
Sometimes pain in the abdomen or directly in the stomach is one of the symptoms of diseases of the digestive organs. Regular or acute pain, accompanied by indigestion and increased body temperature, is a reason for mandatory consultation with a doctor.
to come back to the beginning
Hunger pains, what to do?
The first thing that needs to be done is to analyze the pain, make an appointment with a gastroenterologist, undergo diagnostics, and possibly even a second one. After which the doctor will make a decision - hospitalization.
You can analyze pain sensations as follows: with a stomach ulcer, pain appears approximately half an hour after eating; for duodenal ulcer - after a few hours. These symptoms may appear at night.
If you are experiencing hunger pangs, you must control your diet. Eliminate spicy, fatty and fried foods from your daily diet. Replace a sandwich snack with hot food: soups, cereals. Fish and meat are boiled or steamed. If you have hunger pains, you should give up all kinds of weight loss diets.
The nature of pain in the upper abdomen after eating
Acute intense pain
This feeling in the upper abdomen can be caused by food poisoning, overeating, constipation, indigestion, physical fatigue, muscle tension, injury, viral or bacterial infection, various psychogenic factors and many other reasons, sometimes not amenable to diagnosis.
Burning pain
Burning pain in the upper abdomen is often a consequence of eating hot, salty, sour or spicy foods, which irritate the gastric mucosa and lead to increased secretion of gastric juice.
Constant nagging pain
Most often it occurs due to overeating, eating dry food or due to quickly eating food on the go without first thoroughly chewing. Sometimes such a condition can develop as a reaction to certain foods.
to come back to the beginning
Hunger pains - treatment
Treatment of hunger pain is based on preventing the development of the above pathologies. Therefore, treatment is based on the following:
- normalization of motility of the entire gastrointestinal tract, for this purpose Metoclopramide or Cerucal is prescribed;
- prescription of painkillers, analogues of Analgin;
- in order to reduce the secretion of hydrochloric acid, gastrologists prescribe antisecretory drugs, for example, Lansoprazole, Pantoprazole, Omeprazole and other proton pump blockers;
- prescribing antispasmodics that eliminate local muscle spasms.
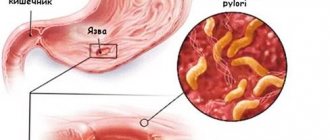
In addition to the above urgent complex treatment, it is necessary to carry out basic pathogenetic treatment. It involves taking antibacterial drugs. Helicobacter, which plays the role of a microbial agent in the development of peptic ulcers, is sensitive to these drugs.
img3_0.png
Often, rare and short-lived pain in the upper abdomen is the result of a violation of the diet and errors in diet. To eliminate this unpleasant symptom, it is recommended to regulate the frequency and timing of meals, observing the appropriate rules of eating behavior. Fractional meals in small portions, 4–6 times a day, have worked well. Dinner should take place at least 3 hours before bedtime. You should also limit your intake of foods that are difficult to digest and maintain fluid balance (drink water on an empty stomach and between meals).
Treatment of stomach pain
To treat stomach pain, in most cases, taking medications is sufficient. Regardless of the diagnosis, the patient will have to follow a gentle diet. Eating is recommended every few hours in small portions. It is necessary to exclude all foods that can irritate the mucous membrane of the organ: fatty and sweet foods, alcohol and carbonated drinks, baked goods and sweets, sauces and spices.
Drug treatment may include several stages:
- antispasmodics and painkillers;
- sorbents;
- drugs to correct the acidity of gastric juice;
- antibiotics and others.
Surgical intervention is indicated for benign neoplasms that do not grow deep into the wall of the organ. Surgery may also be prescribed for gastric ulcers with the risk of perforation of its walls. Some structural anomalies of the organ also require surgical treatment if they interfere with the normal functioning of the digestive tract.
The Clinical Brain Institute specializes in the diagnosis and treatment of stomach pain. The clinic has the opportunity to undergo a full examination, consult with specialists of a wide and narrow profile, and receive an appointment for treatment. Therapy is carried out under the supervision of doctors until complete recovery.
Abdominal discomfort during pregnancy
Heaviness in the lower abdomen in women is a common symptom during pregnancy.
But it is important to distinguish the discomfort that arises due to the development of pathologies from the severity familiar to almost all pregnant girls. Before treatment, it is necessary to understand how heaviness appears in the stomach after eating and the reasons. Such sensations arise due to the fact that the child constantly puts a lot of stress on the stomach. This also happens due to toxicosis, intra-abdominal pressure in the later stages, which also provoke heaviness. Pregnant women are characterized by excessive gas formation, which also causes unpleasant bloating and heaviness in the stomach. Increased gas is a typical problem for expectant mothers; it is affected by excessive amounts of progesterone. Hormones slightly inhibit the peristalsis of the intestines and stomach, which retains food in these sections, so gases are formed more actively. Causes of heaviness in the abdomen:
- eating food quickly;
- inappropriate chewing;
- stressful conditions and severe fatigue;
- eating without feeling hungry;
- overeating before bed.
Certain foods can also cause similar symptoms. For example, some people develop lactose intolerance.
Heaviness in the stomach in children
After eating, heaviness occurs not only in adults, but also in children. The main reasons for this are quite simple:
- the child consumed a large amount of food at one time;
- the food contained unusual and unusual products;
- poor quality of food or incorrect cooking method.
But in some cases, the factors causing such symptoms can be much more serious. For example, the development of appendicitis or infection with parasites. Preschool children often experience allergies to unfamiliar compounds, but in older adults, the cause of pain and heaviness in the stomach can be stress, fatigue and excessive exercise.
All this causes the development of a large number of diseases of the abdominal organs. But other signs can also occur in the opposite case, that is, as secondary manifestations of other diseases (infectious processes in the kidneys, gastritis, gallbladder pathologies).
Sometimes heaviness and bloating appear in the abdomen, the reasons for this are individual lactose intolerance, which can occur in children. In this case, it is necessary to consult a specialist and exclude the consumption of dairy products in order to make an accurate diagnosis.
Diagnostics
A gastroenterologist is involved in finding out the causes of heaviness in the abdomen. At the appointment, the patient is asked how long ago the symptoms began, what, in the patient’s opinion, they are associated with, and whether treatment was carried out at home. The specialist obtains valuable information by palpating the anterior abdominal wall and checking for pathognomonic symptoms. The diagnostic search requires the results of instrumental and laboratory studies. Commonly used:
- Ultrasound of the abdominal cavity.
Ultrasound diagnostics is a painless screening method that shows the location of abdominal organs and allows one to identify space-occupying formations and inflammatory processes. Duplex scanning is used to examine the vessels of the abdominal cavity. - X-ray examination
. A survey x-ray visualizes contrasting gallstones, signs of inflammation or tumor, overdistension or changes in the position of intestinal loops. To clarify the diagnosis, radiography with oral contrast is necessary, the large intestine is examined by irrigoscopy. - Endoscopy
. Diagnosis of atrophic gastritis, ulcers, and stomach tumors is impossible without performing endoscopy with biopsy samples taken for histological analysis. To identify pathological processes in the colon, sigmoidoscopy and colonoscopy are performed. A modern and patient-friendly imaging method is video capsule endoscopy. - Stool tests
. The standard coprogram displays the amount of undigested nutrients, the presence of leukocytes and red blood cells, which is required to verify intestinal diseases. The stool is analyzed for dysbacteriosis, for helminth eggs, and if an infectious pathology is suspected, a bacterial culture of the stool is performed.
To confirm vascular pathologies, MSCT of the abdominal aorta and angiography are prescribed. To identify early functional disorders that provoke heaviness in the abdomen, scintigraphy is performed. Auxiliary information for diagnosis is provided by the results of clinical and biochemical blood tests, coagulogram data and studies of acute phase parameters.
Capsule endoscopy
How to prevent the development of heaviness in the stomach?
Heaviness after eating brings a lot of discomfort in life, especially when this feeling comes very often. It is much better to take the necessary measures in advance to avoid encountering a problem than to eliminate the consequences.
Since most often patients experience pain and a feeling of a full stomach, the causes of which lie in an unhealthy diet, they need to start with normalizing their diet. If there are signs of heaviness in the stomach after eating, what to do is the main question for patients. The answer is simple: eat more often, but less, avoid overeating and breakdowns, chew food diligently, and take your time. It is important to take care of creating a healthy and balanced diet, in which nutrient-rich, but not very heavy food will prevail. If there is heaviness after eating or belching, you need to give up heavy smoking, drinking alcohol, and reduce the consumption of fatty, spicy foods. It is necessary to stop eating without feeling hungry or fasting for a long time, and you should also avoid stress in the process of eating food, because this also affects absorption and the development of unpleasant sensations.
In addition, it is recommended to build your nutrition schedule in such a way that once a week you can reduce the absorption of particularly carbohydrate foods and increase the amount, for example, of fiber and useful minerals. Adhering to these rules is recommended not only for patients who have experienced heaviness in the stomach and nausea after eating, but also for those who want to normalize the functioning of the body as a whole and the abdominal organs.
In order to avoid the unpleasant consequences of heaviness in the stomach and nausea, you need to pay attention to your diet and lifestyle:
- reducing portion sizes and eating more frequently;
- choosing a lighter and healthier diet, since the most common situation is heaviness after fatty foods;
- following a regimen: have breakfast, lunch and dinner at the same time to allow the stomach to develop an activity mode;
- do not overeat before bed: experts advise not to eat 2 hours before bedtime;
- reducing stressful situations in life;
- high-quality chewing of food and no snacking on the go;
- eating fresh foods that are not too hot or too cold;
- getting rid of bad habits;
- reducing the volume of consumed semi-finished products, concentrates, etc.;
- increased physical activity;
- frequent walks in the fresh air.
In the event that there is heaviness in the stomach, the causes of which are related specifically to the culture of nutrition, following all these rules will help get rid of the symptoms, as well as eliminate problems with the gastrointestinal tract. It happens that the causes of discomfort lie in other serious pathologies. Such a regimen will have a beneficial effect on the condition of the body, will help to quickly cure diseases, nausea and heaviness after eating, especially when combined with drug therapy.
Right upper quadrant
Organs in this quarter: liver, gallbladder, duodenum, head of the pancreas (the part of the pancreas firmly attached to the duodenum), part of the colon.
Pain in the right upper quadrant can be caused by hepatitis (inflammation of the liver), cholecystitis (inflammation of the gallbladder), inflammation of the bile ducts (cholangitis), inflammation of the pancreas (pancreatitis), or peptic ulcers of the stomach and duodenum.
Regardless of the cause of the disease, liver inflammation is called hepatitis. Many cases of hepatitis are viral, but the disease can also be caused by alcohol, drugs and other toxic substances.
Liver inflammation can be acute or chronic. With chronic hepatitis, a person usually does not experience any symptoms. During acute hepatitis, abdominal pain, nausea, jaundice (yellowing of the skin, mucous membranes, eyes) may occur, and in more severe cases, liver problems may occur.
The most common types of hepatitis are:
- The hepatitis A virus causes acute inflammation of the liver, which in many cases resolves spontaneously without residual effects. The infection is transmitted through the feces of an infected person (due to poor hygiene conditions and habits), contaminated food and water that has not been properly cooked. Sun-dried tomatoes, fish, shellfish, and frozen berries are the most common sources of infection.
- Hepatitis B is the most common chronic asymptomatic form of abdominal pain. Hepatitis B is transmitted through blood or other body fluids. The hepatitis B virus damages the liver, causing chronic inflammation that can progress to cirrhosis and primary liver cancer. In acute hepatitis B, the course is usually violent - abdominal pain, yellowing of the skin, liver problems. Requires hospital treatment.
- Hepatitis C is also the most common chronic asymptomatic form. Transmitted through blood (highest risk for people before 1990 who donated blood or had a blood transfusion and had any surgery or dental procedures).
Types of hepatitis
Kidney stone disease
This is a disease in which stones (calculi) form in the ducts and glands of the kidneys. This is a fairly common disease. Kidney stones usually do not cause symptoms until they begin to “move” and interfere with the flow of urine.
Kidney stone disease
If small stones get into the peritoneal fluid, the pain is especially severe (colic), the person sweats, gets cold, and a high temperature may rise. In such cases, the patient is hospitalized, given painkillers and antispasmodics, and given intravenous fluid infusions. If signs of infection appear, antibiotics are prescribed. If stones cannot be removed with medications, surgery is performed.
What did I eat and drink before bed or what did I have for breakfast?
Digestive disorders depend not only on what you eat, but also when, how much and how you eat. The process of digesting food is difficult if you:
- Eat late at night, especially large meals, which triggers the production of additional acid even while you sleep
- Eating fatty or spicy foods for breakfast or drinking carbonated or caffeinated drinks
- Smoke in the morning
- Eat on the run, hurrying to leave the house as quickly as possible
If any of the above are common for you, then breaking these habits may help you stop experiencing digestive symptoms. We also advise you to set aside enough time for eating in the morning, do not eat in a hurry. A calm breakfast promotes proper digestion of food. Stomach acid remains in the stomach when you stand, maintaining a stationary position. In the same way, the sitting position when eating allows the digestion process to be almost completely completed by the time you leave the house.
University
→ Home → University → University in the media → Chronic abdominal pain
Chronic abdominal pain is a complex diagnostic and treatment problem in pediatrics and, at the same time, one of the main complaints of children and their parents, a common reason for visiting a doctor. Chronic is defined as abdominal pain that lasts more than 3 months. In children, recurrent is more common, which is said to occur in cases where it is repeated at least 3 times within 3 months. and affects the child’s normal activity.
The nature of chronic abdominal pain can be organic and functional.
Organic diseases. Identification of the cause of chronic abdominal pain in children due to organic diseases is based on: 1) anamnesis; 2) physical examination; 3) laboratory research; 4) radiation and endoscopic research methods; 5) assessing the effectiveness of empirical treatment.
Determining the localization of abdominal pain in childhood has its own peculiarities. Thus, up to 3 years of age, children almost always detect pain in the navel area.
Older children localize pain more accurately. Of particular interest is the observation of J. Apley: “The further the pain is located from the navel, the greater the likelihood of an organic disease.”
Help in identifying the cause of chronic abdominal pain can be provided by parents keeping a diary, which records the type of food eaten and the symptoms observed after it for 2 weeks. In this case, it is possible to detect potential causes of some symptoms, for example, lactose intolerance, etc. It is also necessary to record the use of medications and all therapeutic measures. Family history may indicate a predisposition to gastric and duodenal ulcers, pancreatitis, inflammatory diseases of the biliary system, intestines and a number of other diseases.
During the study, fever, complaints of painful sensations in the joints, the presence of a rash, etc. are recorded. The presence of one or more of the listed symptoms suggests the inflammatory or infectious nature of the pain syndrome.
Since there is a connection between abdominal pain, nutrition and the physical development of the child, data on the patient’s height and body weight is required.
A full clinical examination is carried out, followed by focusing on the abdomen. Pain during examination of the abdomen will be indicated by a grimace on the child’s face or a remark. Important findings are enlargement of the liver, spleen, the presence of space-occupying formations, as well as localization of pain. Further diagnostic search is carried out taking into account the obtained data.
If topical diagnosis is not possible at the outpatient stage, the examination is continued in a hospital or in a diagnostic center. Here they carry out endoscopic examination (fibrogastroduodenoscopy, colonoscopy), biopsy (according to indications), sonography, radiography (cholecystography, irrigography), CT, MRI, scintigraphy, acidometry; determination of the enzymatic function of the digestive tract, electrophysiological study, stress tests, study of biochemical parameters of blood and urine, intestinal microbiocenosis, genetic examination, etc.+
Other methods of laboratory examination are used in connection with the characteristics of the data obtained. These include liver enzymes and amylase, serologic testing for H. pylori and amoebiasis, and stool culture and parasite testing. A study for lactose intolerance is carried out if the evaluation of the empirical diet does not produce results. Analyzing the child's body's response to treatment is part of the diagnostic process. For example, taking antibiotics can predispose to the development of intestinal dysbiosis, medications for the treatment of acne can predispose to esophagitis, and tricyclic antidepressants can predispose to constipation.
Main causes of abdominal pain
The most common causes of chronic abdominal pain are: chronic gastritis, duodenitis and gastroduodenitis. There are chronic gastritis type A (autoimmune), gastritis type B (associated with H. pylori) and gastritis type C (chemical or reflux gastritis). Type B gastritis is more common and is accompanied by severe pain that occurs on an empty stomach or 1-2 hours after eating. There is pain and sometimes tension in the abdominal wall in the epigastrium and pyloroduodenal area. Endoscopically, structural and inflammatory changes in the antrum of the stomach are revealed.
Duodenitis and gastroduodenitis are also characterized by pain associated with food intake or its nature (fried, spicy), as well as with long breaks in food. Dyspeptic syndrome is manifested by nausea, vomiting, which brings relief, belching, and heartburn. Symptoms of chronic intoxication and vegetative-vascular dystonia are often observed. Pain in the epigastric region is detected.
Peptic ulcer of the stomach and duodenum in children, unlike adults, often does not have clear clinical symptoms, since it is often characterized by the presence of superficial ulcers. The leading symptom is pain in the epigastrium or pyloroduodenal region, occurring on an empty stomach or 1-3 hours after eating, often at night and more severe than with gastroduodenitis. Eating temporarily relieves the condition. Hidden bleeding is possible. Endoscopic examination is decisive in diagnosis.
Chronic abdominal pain may be associated with esophagitis, which develops due to gastroesophageal reflux. This is characterized by pain behind the sternum during meals, in the epigastric region, a sensation of passing a food bolus, and dysphagia. Belching with a sour smell and heartburn are observed. Relatively rarely, the cause of chronic pain in the upper abdomen can be gastroptosis and hiatal hernia. In this case, pain occurs 2–3 hours after eating, especially in a horizontal position of the child, when bending forward and physical activity. This pathology can be assumed in the absence of effect from therapy for esophagitis and gastroduodenitis.
The cause of chronic abdominal pain can be chronic enteritis, colitis, enterocolitis. In this case, the pain is localized in the navel, hypogastric region on the left and right. It often occurs in the afternoon, sometimes 1.5–2 hours after eating. Its appearance is provoked by the consumption of large quantities of fresh vegetables, fruits, and milk. The pain is accompanied by bloating, rumbling, and intensifies with physical activity. If it is localized on the right, it is necessary to exclude acute appendicitis. Chronic intestinal damage is characterized by stool disorder - alternating diarrhea (with enteritis) and constipation (with colitis).
Nonspecific ulcerative colitis and Crohn's disease are characterized by recurrent abdominal pain, paroxysmal or constant. They are localized throughout the abdomen, to the left, to the right of the navel, but more often in the lower abdomen, intensifying after eating or physical activity. The stool is unstable, diarrhea gives way to constipation, mucopurulent or bloody stools, and the presence of tenesmus are noted.
Diagnosis is relatively simple if there are bloody stools, forced bowel movements at night, the presence of a perianal inflammatory process or a mass formation in the right iliac region (inflammatory bowel changes). Delayed sexual development, anemia, aphthous ulcers in the mouth, chronic hepatitis, synovitis or arthritis of large joints may occur. The diagnosis is established on the basis of irrigography and colonoscopy with biopsy.
When analyzing complaints from a child and his parents, you should pay attention to:
• duration of pain. Short-term is more often associated with motor disorders, long-term (more than 3 hours) - with inflammatory causes;
• connection of pain with the intake and nature of food;
• with defecation;
• presence of symptoms of “upper dyspepsia” - belching, heartburn, nausea, vomiting;
• bowel dysfunction.
A significant group of children with chronic abdominal pain consists of patients with cholepathy. These include diseases of the gallbladder and biliary tract - developmental anomalies, inflammatory, parasitic, tumor diseases, cholelithiasis. The pain is provoked by the nature of the food (spicy, fatty, fried). Characterized by nausea, vomiting that does not bring relief, belching, bitterness in the mouth, changes in stool (constipation, diarrhea), and sometimes uneven coloring of individual stool fragments. With the inflammatory nature of cholepathy, prolonged low-grade fever or febrile body temperature during an attack is possible. There is pallor of the child's skin, sometimes telangiectasia, and subicteric sclera. There is pain in the right hypochondrium. With severe cholestasis, liver enlargement is possible, which disappears after choleretic therapy.
Other forms of damage to the biliary tract (cholelithiasis, developmental abnormalities, tumors, parasitic diseases) do not have specific symptoms and are detected mainly during a paraclinical examination of the child.
Chronic abdominal pain may be associated with pancreatic pathology. Acute pancreatitis, in particular the edematous form, is both an independent disease and a reactive condition against the background of other pathologies of the digestive organs. Destructive forms of pancreatitis in children are rare. Chronic pancreatitis occurs with paroxysmal abdominal pain. Their localization depends on the area of damage to the pancreas. Its total defeat is characterized by intense girdling pain, which is accompanied by severe anxiety of the child, vomiting, which does not bring relief, sometimes indomitable. There is a disorder of the stool - constipation, more often diarrhea. Symptoms of intoxication are expressed.
The cause of chronic abdominal pain in children can be helminthiasis. In this case, the pain does not have any specificity and is accompanied by chronic intoxication, loss of appetite, drooling, and bruxism.
The second group that causes the presence of chronic abdominal pain is diseases of the urinary system: pyelonephritis, nephroptosis, vesicoureteral reflux, cystitis, urolithiasis, dysmetabolic nephropathy and more rare kidney pathology. These diseases are characterized by pain, often not associated with eating. In case of urolithiasis, nephroptosis, attacks can be provoked by hypothermia and physical activity. The pain is localized near the navel, lower abdomen, and lower back.
With vesicoureteral reflux, it is felt along the ureter. In this case, right-sided reflux can simulate acute appendicitis. When the kidneys are fused (horseshoe-shaped, biscuit-shaped, S- and L-shaped), the pain is localized in the epigastric region and is accompanied by dyspeptic disorders. Cystic formations of the kidneys lead to pain in the epigastrium, sometimes to renal colic. Colic is also characteristic of urolithiasis, dysmetabolic nephropathy, nephroptosis, hydronephrosis. With hydronephrosis, a nagging, dull pain in the abdomen is possible, accompanied by flatulence and dyspeptic disorders. With pyelonephritis, prolonged low-grade fever or “unmotivated” rises in temperature are noted. In general, the pathology of the urinary system is characterized by dysuric symptoms.
The group designated as “other diseases”, which may cause chronic abdominal pain in children, is represented by a variety of pathologies, including rare ones. However, gynecological pathology is more often observed in girls - salpingitis, adnexitis, ovarian cysts. The pain is often localized in the lower abdomen, in the mesogastric region, and can be acute, paroxysmal and nagging, aching, constant, radiating to the lower back. In menstruating girls, it is possible in the lower abdomen during the ovulation cycle. Functional diseases. The greatest difficulty is in the interpretation of chronic abdominal pain caused by functional disorders of the digestive system, when examination of the child does not reveal the morphological cause causing the pain. In accordance with the Rome criteria (Rome, 2006), several common signs are identified for functional disorders, regardless of the type of lesion:
• duration of main symptoms is at least 3 months. over the past year;
• absence of organic pathology;
• multiple nature of complaints (not only disorders of the digestive system) with the general good condition of the patient and a favorable course of the disease without noticeable progression;
• the importance of psychosocial factors and neurohumoral regulation disorders in the formation of the main symptoms.
The diagnosis of any functional disorder is a diagnosis of exclusion. It can be diagnosed only after a thorough examination of the patient and exclusion of organic causes that cause pain and other symptoms of the disease. Children should have no “alarm symptoms” - weight loss, loss of appetite, fever, changes in peripheral blood tests, blood in the stool, etc.
Psychosocial factors and social maladaptation are important in the pathogenesis of functional disorders and chronic abdominal pain. It is believed that they may be primary in the development of functional disorders and, in combination with genetic predisposition, determine the formation of the type of motor disorders and visceral hyperalgesia. The interdependence of the central nervous system and all peripheral influences leads not only to direct dysfunction of the gastrointestinal tract, but also to neuropsychological abnormalities. As a result, functional disorders are based on motor dysfunction caused by the failure of regulatory relationships on the brain-gastrointestinal axis.
Intestinal motility disorders in functional disorders can occur as hypotension, atony, or have a mixed nature. In functional disorders accompanied by chronic abdominal pain, in addition to motor disorders, sensory deviations characterized by visceral hypersensitivity (hyperalgesia) are typical. There is a change in the sensitivity of the receptor apparatus to irritants and a decrease in the pain threshold.
Chronic recurrent abdominal pain in children has a variety of causes. To make a correct diagnosis, it is necessary to take into account “symptoms of anxiety” and use targeted diagnostic methods depending on the clinical course and location of the pain syndrome.
Patients describe abdominal pain in functional disorders in different ways - from unpleasant sensations to unbearable, cramping pain without clear localization, occurring for no apparent reason or associated with eating, stress, physical activity, or defecation. In this case, the peculiarity of the pain syndrome is that it occurs in the morning or daytime, when patients are active, and subsides during sleep.
In children in the first months of life, chronic recurrent abdominal pain manifests itself in the form of intestinal colic, which manifests itself as restlessness and crying. To diagnose intestinal colic, the so-called “rule of three” is used - crying for 3 or more hours a day, at least 3 days a week for 3 weeks in a row. Colic appears in a child at the age of 6 weeks and can be observed until 3-4 months. Intestinal colic is caused by the tension of the digestive processes in conditions of physiological immaturity of the infant's gastrointestinal tract and the load on the intestines, which is associated with a large volume of nutrition. At the same time, children gain weight well, maintain a positive emotional mood, appetite, and normal bowel movements.
With functional stomach disorders, pain occurs regardless of food intake - short-term, of varying intensity, localized in the epigastric region. Sometimes pain appears after mental stress and is more often observed in emotionally labile children. The attacks are accompanied by symptoms of autonomic instability. The examination reveals moderate pain in the epigastrium and right hypochondrium. Endoscopic examination is decisive in diagnosis. In this case, the absence of morphological changes and impaired motor function of the upper gastrointestinal tract in the form of spasm or hypotension of the sphincters, impaired peristalsis are revealed.
Pain based on functional disorders is characterized by:
• absence of disease progression;
• the changing nature of complaints;
• the patient's assessment of pain as very severe;
• the presence of numerous complaints concerning other organs and systems;
• short medical history;
• parents’ excessive demands on the child, problems at school;
• emotional stress in the family;
• absence of objective changes during examination.
Pain based on functional disorders is not characterized by:
• local stereotypic pain;
• awakening from pain during sleep;
• special behavior during attacks;
• anorexia;
• vomit;
• persistent constipation or diarrhea;
• presence of chronic gastrointestinal diseases in family members;
• retardation in physical development or loss of body weight;
• fever;
• joint pain;
• blood in the stool.
Biliary dysfunctions . Biliary dyskinesias play a significant role among the causes of chronic abdominal pain. The hypertensive form is characterized by paroxysmal, short-term pain localized in the right hypochondrium, sometimes radiating to the right shoulder and scapula. Vegetative dystonia is pronounced. There is pain in the right hypochondrium. This form of dyskinesia is based on spasm of the sphincter apparatus of the biliary system.
With the hypotonic form of dyskinesia, the pain is often moderate, but longer lasting. The pain is provoked by physical activity, eating fatty foods, and overeating. There is moderate pain in the right hypochondrium, an enlarged but soft liver. This dyskinesia is based on stagnation of bile in the biliary system and a decrease in the motor-evacuation function of the gallbladder.+
Functional disorders of the gallbladder are manifested by impaired contractile function, slower evacuation of bile and stretching of the bladder, which causes pain. Dysfunction of the sphincter of Oddi may be associated with functional, motor, usually spastic disorders of the sphincter of the common bile duct, sphincter of the pancreatic duct or common ampullary duct. Depending on this, symptoms of damage to the biliary tract, pancreas, or joint changes predominate.
Irritable bowel syndrome . The most common and best studied among functional disorders of the digestive canal. The disease is manifested by abdominal pain, impaired bowel movements, and flatulence. Due to the lack of a clear conceptual apparatus in young children, it is difficult to clarify subjective sensations that are pathognomonic for establishing this diagnosis in strict accordance with the Rome criteria. Symptoms that can be used to diagnose irritable bowel syndrome are:
• stool frequency less than 3 times a week;
• stool frequency more than 3 times a day;
• hard or bean-shaped stool;
• thin or watery stool;
• straining during defecation;
• imperative urge to defecate (impossibility of delaying defecation);
• feeling of incomplete bowel movement;
• secretion of mucus during bowel movements;
• feeling of fullness, bloating or transfusion in the abdomen.
A significant role in the pathogenesis of irritable bowel syndrome belongs to the psycho-emotional status of the patient, as well as the presence of autonomic dysfunction. Psychopathological disorders in such children are characterized by a shallow level of damage (neuroses, neurotic reactions). The close connection between depression and chronic abdominal pain is explained by general biochemical processes, and primarily by the insufficiency of monoaminergic (serotonergic) mechanisms. This is supported by the effectiveness of antidepressants, especially serotonin reuptake inhibitors, in the treatment of abdominal pain.
There are two main forms of irritable bowel syndrome—hypertensive and hypotonic.
The hypertensive form is characterized by periodic cramping pain of uncertain localization or in the left iliac region. In this case, the abdomen is swollen, spastic contraction and soreness of the descending and sigmoid colon are determined by palpation. Constipation is common. After defecation, the pain decreases.
The hypotonic form is characterized by a feeling of discomfort, distension, bloating with moderate and intermittent pain. After defecation, the pain usually disappears.
The diagnosis of irritable bowel syndrome is a diagnosis of exclusion, requiring a thorough analysis of complaints, anamnesis, clinical laboratory and biochemical blood tests, instrumental studies to exclude organic intestinal pathology (ultrasound, colonoscopy, irrigography, parasitological studies, etc.). An etiological treatment for this syndrome has not yet been developed. Currently used therapy is aimed at individual known links in pathogenesis. One of them is the normalization of the microbial composition of the intestine. Correction of dysbiotic disorders, as well as prevention of their development, can be achieved with the help of functional nutrition. The use of myotropic antispasmodics is recommended. Since one of the leading mechanisms of the pathogenesis of irritable bowel syndrome is autonomic dysfunction and neuropsychiatric disorders, therapy includes drugs that correct these disorders.
Functional abdominal pain syndrome . Abdominal pain without intestinal dysfunction is classified as a separate category. This syndrome is defined as constant, almost constant or often recurrent abdominal pain, which is characterized by the following features:
• last for at least 6 months;
• are not associated with specific physiological factors (food intake, defecation, menstrual cycle, etc.);
• accompanied by a decrease in physical activity;
• characterized by a non-progressive course;
• do not have signs that would allow these pains to be attributed to other functional disorders of the gastrointestinal tract.
Functional abdominal pain syndrome is observed in prepubertal age with two frequency peaks. The first corresponds to the age of 5–7 years, is observed in 5–8% of children and often coincides with their sending to school. The second peak occurs in almost 25% of children and is observed at the age of 10–12 years with the highest frequency in girls. This syndrome is considered as a biopsychosocial disease. In this case, pain is caused by amplification (strengthening) of the perception of pain in the cerebral cortex due to excessive afferent impulses (to a lesser extent) and its insufficient descending suppression (to a greater extent). The process of amplification of pain is facilitated by mental stress - the death of parents, previous operations, the anniversary of a tragic event, etc.
Much attention in the development of functional abdominal pain syndrome is paid to episodes of physical or sexual coercion of children. Anamnesis-wise, they are detected in adolescence in 64% of patients with this syndrome (2.8 times more often than in children with organic diseases). The presence of such episodes causes patients to desire diagnostic tests, prompts them to frequently consult a doctor, and causes resistance to prescribed treatment. It is characteristic that patients, as a rule, do not tell the doctor about such episodes, and identifying them requires delicate formulation of questions.
In functional abdominal pain syndrome, the latter is not associated with physical activity and in most cases is accompanied by vegetative signs (pallor, nausea, dizziness, malaise, etc.). There is often a family history of a predisposition to functional bowel diseases.
When questioning patients, it is possible to identify a number of features of the pain syndrome: pain exists for a long time (months, years) and is localized in various parts of the abdomen; often diffuse, emotionally described as very intense, constant, having no connection with food intake and the act of defecation. Patients often say that “if it weren’t for pain, life would be wonderful.” They insist on various diagnostic studies and surgical interventions.
An objective examination of some patients reveals postoperative scars on the anterior abdominal wall, indicating operations, sometimes performed without objective indications. It is possible to identify a “closed eyes symptom” - when palpating the abdomen, the patient closes his eyes, while a patient with acute abdominal pain due to organic causes watches the doctor with open eyes, fearing increased pain. The “phonendoscope symptom” is known - pressing with a phonendoscope on the anterior abdominal wall during functional abdominal pain syndrome does not cause increased pain, whereas in pain associated with an acute surgical disease, this manipulation turns out to be very painful.
The diagnosis of functional abdominal pain syndrome should be a diagnosis of exclusion. It is legitimate to place it only after a thorough examination, including not only laboratory testing of blood, urine, feces, but also echography of the abdominal organs, endoscopic (FGDS, colonoscopy) and, if necessary, radiation research methods (x-ray, CT, MRI, scintigraphy, etc. .). In cases where the diagnosis still remains unclear, the issue of performing laparoscopy is discussed.
Chronic abdominal pain may be due to cyclic vomiting syndrome (abdominal migraine), described by J. Gee in 1882 under the name “periodic syndrome.” The disease is characterized by episodic attacks of nausea, abdominal pain, vomiting, usually starting at night or in the morning and lasting from 6 to 48 hours with subsequent intervals of well-being (weeks, months). Most children experience autonomic disorders (pallor, diarrhea, weakness, tachycardia, etc.). Treatment consists of prescribing antiemetics or migraine medications. Yuri ABAEV , Professor of the Department of Pediatric Surgery of BSMU, Doctor of Medicine. Sciences Medical Bulletin, August 7, 2008
Share
Treatment is necessary. When to see a doctor
Many different health problems can cause morning stomach pain. While some conditions may resolve on their own, others will require immediate treatment. When considering medical care, the following factors should be considered:
Severity: If the pain is so severe that the person cannot stand, seek medical attention immediately. Early symptoms of appendicitis may include abdominal pain.
Duration: The longer a person experiences abdominal pain in the morning, the sooner they need to seek medical help.
Age: Severe abdominal pain in young people may indicate appendicitis. In older people, this may indicate gallbladder problems. Both conditions require immediate medical treatment.
Speed of onset: Sudden abdominal pain is a potential symptom of appendicitis, especially if the pain gets worse.
Other symptoms: People with appendicitis may develop a fever along with abdominal pain. Abdominal pain along with nausea may indicate a blockage or other serious condition. Bleeding from the rectum is a possible sign of a condition that requires immediate medical treatment.
How to diagnose heaviness in the stomach?
Since it is usually quite simple to recognize heaviness in the abdomen and bloating, the main emphasis in diagnosing the pathology is on understanding the root cause of the symptoms and forming a further treatment plan. The gastroenterologist is responsible for determining therapy, but if the symptoms are not serious, a therapist can also help.
When faced with heaviness in the stomach, what should you do? Specialists independently determine examination methods:
- biochemical or general AA;
- Ultrasound;
- MRI;
- FGDS;
- X-ray;
- endoscopy of organs.
Any examination should begin with a consultation with a specialist; his task at this stage is to collect a detailed anamnesis, that is, to record a description of the complaints, their properties, and also to conduct an examination of the patient.
Heaviness in the lower abdomen, which does not develop due to gastrointestinal pathologies, appears as a result of an unhealthy eating schedule and poor foods. The patient may eat too much food, and if he eats this way regularly, the feeling of discomfort will not leave the patient. This is a big burden, because the body has to work harder to eliminate the consequences of overeating and other phenomena. Energy consumption increases, the quality of organ functioning decreases, and therefore the likelihood of developing serious diseases increases.