- nutrition for various diseases
Peptic ulcer of the stomach and duodenum is a chronic relapsing disease that is characterized by the formation of ulceration - a defect in the mucous membrane - of the stomach or duodenum. It requires not only drug treatment, but also non-drug prevention and support. Nutritional therapy plays a key role in the treatment and prevention of this disease. It creates optimal conditions for the functioning of the gastrointestinal tract, reduces the likelihood of a negative reaction of the body to medications, provides a gentle mechanical effect on the gastrointestinal mucosa and promotes the proper formation of the food bolus and the absorption of nutrients.
General rules
Peptic ulcer disease is a chronic disease, the manifestation of which is a recurrent ulcer. Peptic ulcer of the stomach and duodenum occurs against the background of an imbalance between aggressive factors, which are Helicobacter pylori and the acid-peptic state, and protective factors - the mucus of the duodenum and stomach and the ability of the mucous membrane to repair. Today we will touch on duodenal ulcer and nutritional characteristics during different periods of the disease.
In the typical version, the ulcer is localized on the posterior or anterior wall of the duodenum and more often in the bulb (this is the part of the duodenum closest to the stomach). Functionally, this part is associated with the intake of acidic gastric contents, which here acquire an alkaline reaction. The duodenal glands produce an alkalizing secretion, and normally stomach acid is neutralized. The alkalization process is also affected by bile and pancreatic juice (the bile duct and pancreatic juice open into the bulb).
The causes of duodenal ulcer are:
- infectious pathogen Helicobacter pylori, which is detected in 70-80% of patients;
- eating disorders (consumption of fried and fatty foods, fast food, starvation diets, consumption of alcohol and excessively spicy foods);
- long-term stressful situations, which in the case of an ulcer of the bulb cause disruption of the nervous regulation of its function (the secretion of protective mucus is disrupted).
For these reasons, the secretory function of the duodenum is disrupted and its protective barrier is reduced, constant irritation of the mucous membrane is maintained, ultimately leading to an ulcerative defect.
The main complaint with this disease is pain. Its intensity depends on the state of the nervous system, age and individual sensitivity of the patient to pain. The pain takes on a nocturnal and “hungry” character and is significantly reduced when eating. A characteristic rhythm of pain is noted: hunger-pain-eating-pain-free interval-hunger-pain again.
Dyspeptic disorders are also typical - heartburn , vomiting, nausea and belching. As the duration of the disease increases, the number of these symptoms increases. Some patients may have a decreased appetite and often experience a tendency to constipation or diarrhea .
Treatment is aimed at eliminating aggression factors and includes:
- suppression of gastric secretion;
- anti-Helicobacter therapy;
- correction of the patient’s psychoneurological status;
- stimulation of reparative processes in the mucosa.
In order to suppress secretion, H2 blockers ( cimetidine , ranitidine , famotidine ), which have recently been used less and less because they do not completely block acid synthesis. They were replaced by proton pump blockers, which are 3-10 times H2 blockers The era of PPIs began with Omeprazole , later this group was replenished with Lanzoprazole , Pantoprazole , Pariet ( rabeprazole ) and Esomeprazole .
Effective regimens have been developed for anti-Helicobacter therapy - 3-component and 4-component, prescribed for 7 days. Due to the risk of developing dysbiotic changes in the intestines, probiotics ( Bifiform , Linex ) are included in parallel.
Normalization of autonomic tone is achieved by taking Atarax , Adaptol or Grandaxin . As a result, autonomic reactivity is restored, which ensures an adequate response of the body to external stimuli. Due to the restoration of psycho-vegetative balance, an acceleration of scarring of ulcers is noted.
Among the agents that enhance reparative processes, one can name Gastritol , which includes plant components that promote the rapid restoration of damage to the mucous membrane. Next, the issue of maintenance therapy is resolved. For multiple ulcers, continue taking De-nol and PPIs for up to three weeks. With concomitant gastroesophageal reflux disease, the duration of taking antisecretory drugs is increased to 6-8 weeks.
Violation of the diet and consumption of food that irritates the mucous membrane is one of the causes of peptic ulcer disease, therefore therapeutic nutrition is an important component of treatment. The diet for duodenal ulcers is aimed at eliminating pain and dyspeptic symptoms. Therapeutic nutrition for peptic ulcers should help reduce the acid factor, the activity of which is most often increased, and stimulate ulcer healing.
At any stage of the disease, secretion stimulants and mucosal irritants are excluded (to one degree or another). Eating small portions of food is gentle on the mucous membrane and reduces inflammation of the duodenum. Regular and small meals greatly facilitate the digestion and absorption of foods.
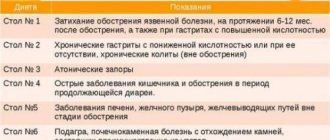
During different periods of the disease (exacerbation, unstable remission, stable remission), the diet is different and the following tables can be prescribed sequentially:
- No. 1A with maximum limitation of all types of effects on the mucous membrane;
- No. 1B with a mild limitation of all types of aggression on the stomach, the average treatment time is up to two weeks;
- №1 with moderate sparing of the stomach.
The timing of these diets depends on the patient’s condition and the severity of pain and dyspeptic syndrome. The sequential assignment of tables with a gradual expansion of products and different methods of preparing them prepares the gastrointestinal tract for the transition to a common table.
What diet is used during exacerbation of the disease? It depends on the severity of the exacerbation. For severe pain, Diet 1A , which maximally limits all factors of influence (mechanical, chemical and thermal). The diet includes warm, pureed dishes, the consistency of which is liquid, but as the process subsides, it becomes mushy. Products that have a weak juice effect are consumed (milk, eggs, pureed cereals with milk, boiled fish and meat in various forms of preparation). This dietary food is prescribed for the period of severe exacerbation - 7-10 days.
- It is recommended to eat six meals a day with limited portion sizes.
- Food is prepared in liquid or jelly form, which spares the mucous membrane as much as possible and promotes ulcer repair.
- Only slimy soups (with water or milk), prepared from oatmeal, semolina or rice. Mucus soups are decoctions obtained by cooking cereals, which are filtered and the cereals are removed. You can add a little salt to the finished soup and add butter to it. This type of soup can be prepared from ground cereal flour.
- Meat, chicken and fish dishes in the form of puree or steam soufflé. For cooking, choose lean varieties of meat and fish, peeled from skin and tendons and passed through a meat grinder several times.
- Porridge made from buckwheat, rice and oatmeal. They are well boiled, rubbed and diluted to a liquid state with water (milk). A small amount of butter is added to the finished porridge.
- Milk, calcined cottage cheese, milk jelly and cream (in soups). Whole milk - 4 glasses per day.
- Soft-boiled eggs or steam omelet. The patient can eat 2 eggs daily.
- Kissels and jellies from sweet berries, berry and fruit juices, diluted with boiled water with the addition of sugar or honey. You can drink weak tea (with milk, cream), rosehip infusions and a decoction of wheat bran.
Table No. 1A provides for the exclusion of secretion agents and mucosal irritants from the diet: any broths, sour drinks and juices, fermented milk drinks, any vegetables, coarse cereals and bread.
Food should be light and easily digestible, so mushrooms, tough meat with tendons, poultry and fish skin are not allowed. Eating excessively cold and hot foods is not allowed. Because sharp food temperatures have an adverse effect on the mucous membrane and slow down the regeneration processes of the mucous membrane.
After a week, as the condition improves, the patient can be transferred to Table No. 1B . This table is less restrictive and gradually increases the content of nutrients and calories. The cooking methods and the main list of products remain the same, but dried wheat bread, vegetable and fruit purees are added (can be used for baby food). Instead of slimy soups, pureed soups are used, and meat and fish can be used to make quenelles, purees and cutlets.
During the recovery period after an exacerbation, as well as during mild exacerbation, patients are prescribed moderately gentle and physiologically nutritious nutrition - Table No. 1 . Previously, there were recommendations for a patient to remain on this therapeutic diet for a long time (up to six months). However, if you feel well, the time spent on Diet No. 1 is reduced to 2-3 months.
The absence of strong irritants in food (meat, mushroom broth, fish soup, strong tea, fried foods, coffee, carbonated drinks, marinades, mustard, alcohol) creates conditions for successful treatment and a long relapse-free period.
The diet is expanded by not pureed food and raw vegetables and fruits are added (sweet plums, apples, apricots, peaches, nectarines, and tomatoes). When carrying out anti-relapse treatment in the autumn-spring periods, you should again switch to gentle nutrition for 2-4 weeks (first Table No. 1B , and then No. 1 ).
A perforated ulcer (the formation of a through defect in the wall of the duodenum) is one of the most dangerous complications, since the contents of the intestine enter the abdominal cavity and cause peritonitis . This condition is considered urgent and surgical intervention is indicated. In most cases, the perforated ulcer is sutured.
After surgery for a perforated ulcer, the diet is very gentle; dishes are steamed without oil or salt. Dishes high in carbohydrates are kept to a minimum, liquid intake and portion sizes are limited.
- the first two or three days - hunger;
- from the fourth day, rosehip decoction, weak tea, fruit jelly with a small amount of sugar are allowed;
- from the fifth day, pureed liquid rice or oatmeal, pureed vegetable soup, soft-boiled eggs are introduced;
- from the seventh day - vegetable puree, soufflé and chicken cutlets and boiled chopped fish.
Actually, this is the diet of Tables No. 1A and No. 1B , the timing of which is strictly individual and depends on the condition of the postoperative patient. After 10-14 days, the patient is transferred to dietary Table No. 1 , which will be discussed below. Food should only be consumed warm, as cold foods take a long time to digest, and hot foods irritate the mucous membranes. The amount of food consumed decreases. Frequent meals up to 5-6 times a day are recommended. Basic cooking techniques - boiling, stewing.
Since stomach and duodenal ulcers tend to worsen seasonally, special attention should be paid to nutrition in the spring and autumn. During this period, it is better to abandon foods that provoke exacerbation (spicy, smoked, deep-fried) and switch to light foods that do not irritate the mucous membranes. It is important to follow a diet and avoid long breaks between meals.
The diet for stomach and duodenal ulcers is based on the same principles. The most suitable diets in the autumn-spring periods, depending on the severity of the exacerbation, are No. 1B or No. 1 . Perhaps during this period the doctor will prescribe you to take medications, although preventive anti-relapse treatment is now being abandoned. It is better for patients to keep an observation diary and note the factors that provoke exacerbations (stress at work, exams, dietary errors, etc.).
Diet for ulcers after exacerbation is eliminated
Patients with peptic ulcer disease have to get used to constant restrictions and preferential nutrition according to table No. 1. Some gastroenterologists believe that the period of its use can be reduced to two months after the next exacerbation. But experience shows that the transition to everyday nutrition again leads to an exacerbation of the process. Therefore, it is better to monitor your health based on pain and adhere to the established exceptions.
The diet for peptic ulcer disease during remission should remain easily digestible, without strong irritants. Therefore, the following dishes are not allowed in the diet:
- from fatty meat and fish (rich broths, cabbage soup, fish soup);
- tough smoked meat and poultry with bones, cartilage, skin;
- mushrooms;
- strong tea and coffee;
- alcohol, beer, kvass, carbonated drinks;
- seasonings (mustard, pepper).
The cleaning of food stops. The porridges are prepared viscous and thick; buckwheat is allowed. Instead of jelly, you can gradually eat salads made from raw vegetables (tomatoes, cucumbers), sweet fruits (apples, apricots, nectarines, peaches). It is advisable to pre-clean the skin.
Doctors recommend that patients with peptic ulcers undergo anti-relapse treatment in the spring and autumn. Nutritionists advise for this period to switch first to table 1b, then table No. 1. Gentle nutrition for a month can support the body and prevent another exacerbation.
You will have to forget about your favorite fried foods
Authorized Products
Diet for duodenal ulcer includes:
- Soups that are prepared with potato broth or a decoction of prefabricated vegetables. At first they add pureed vegetables and cereals (semolina, buckwheat, rolled oats, rice), and then switch to non- pureed ones. The first courses add pureed meat, an egg-milk mixture and a little butter. Milk cereal soups and noodle soups are allowed.
- Use lean dietary meat (beef, veal, young lamb, chicken, rabbit and turkey). Prepare steamed and boiled dishes (cutlets, dumplings, puree, soufflé, meatballs, zrazy). A month after an exacerbation or surgery, meat baked in the oven is allowed.
- Lean fish is steamed or baked without crust. The skin is removed, the fish can be cooked in pieces or chopped (cutlets, meatballs, meatballs, zrazy).
- Porridges are cooked in milk or water from rice, semolina, buckwheat or oatmeal; you can also use vermicelli. The porridge needs to be boiled well and kneaded a little, the buckwheat should be rubbed first. You can make puddings and casseroles from cereals with the addition of cottage cheese.
- Vegetables with low fiber content (potatoes, beets, pumpkin, zucchini, carrots, green peas, cauliflower). They are steamed and served pureed. By adding whipped whites and semolina to the puree and steaming the mixture in molds, you get a vegetable soufflé.
- Pumpkin and zucchini can be eaten ungrated, as they are the most delicate vegetables. To improve the taste, chopped dill can be added to vegetable purees and soups.
- Small amounts of butter and vegetable oils are used to season ready-made dishes.
- Wheat bread (stale or dried). The diet can be expanded by introducing low-fat biscuits and dry cookies. It is not often possible to eat baked savory pies with different fillings (apples, jam, cottage cheese, meat, fish).
- Milk and cream, non-acidic yogurt and kefir are added. Non-acidic fresh cottage cheese can be eaten in its natural form or made into cheesecakes, puddings, and lazy dumplings. Mild cheese can be introduced infrequently.
- Two eggs, eaten every other day, cooked as a steam omelet or soft-boiled.
- Expanding the diet allows you to switch to an untreated table, on which you are allowed to eat a salad of boiled vegetables with meat or fish, jellied fish, herring and sturgeon caviar.
- Desserts steamed from pureed berries, purees, jelly, jelly, sambuca, compotes. Sweet berries and fruits can be consumed baked or boiled. You can eat milk jelly, non-sour jam, meringues, marshmallows, marshmallows and honey. Drinks allowed are fruit juices, rosehip infusion, weak coffee with milk, tea with milk/cream.
Table of permitted products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| zucchini | 0,6 | 0,3 | 4,6 | 24 |
| cauliflower | 2,5 | 0,3 | 5,4 | 30 |
| potato | 2,0 | 0,4 | 18,1 | 80 |
| carrot | 1,3 | 0,1 | 6,9 | 32 |
| beet | 1,5 | 0,1 | 8,8 | 40 |
| pumpkin | 1,3 | 0,3 | 7,7 | 28 |
Fruits | ||||
| apricots | 0,9 | 0,1 | 10,8 | 41 |
| watermelon | 0,6 | 0,1 | 5,8 | 25 |
| bananas | 1,5 | 0,2 | 21,8 | 95 |
| melon | 0,6 | 0,3 | 7,4 | 33 |
| nectarine | 0,9 | 0,2 | 11,8 | 48 |
| peaches | 0,9 | 0,1 | 11,3 | 46 |
| apples | 0,4 | 0,4 | 9,8 | 47 |
Berries | ||||
| strawberry | 0,8 | 0,4 | 7,5 | 41 |
| raspberries | 0,8 | 0,5 | 8,3 | 46 |
Cereals and porridges | ||||
| buckwheat (kernel) | 12,6 | 3,3 | 62,1 | 313 |
| semolina | 10,3 | 1,0 | 73,3 | 328 |
| cereals | 11,9 | 7,2 | 69,3 | 366 |
| white rice | 6,7 | 0,7 | 78,9 | 344 |
Flour and pasta | ||||
| noodles | 12,0 | 3,7 | 60,1 | 322 |
Bakery products | ||||
| white bread crackers | 11,2 | 1,4 | 72,2 | 331 |
Confectionery | ||||
| jam | 0,3 | 0,2 | 63,0 | 263 |
| jelly | 2,7 | 0,0 | 17,9 | 79 |
| marshmallows | 0,8 | 0,0 | 78,5 | 304 |
| meringues | 2,6 | 20,8 | 60,5 | 440 |
| paste | 0,5 | 0,0 | 80,8 | 310 |
| Maria cookies | 8,7 | 8,8 | 70,9 | 400 |
Raw materials and seasonings | ||||
| honey | 0,8 | 0,0 | 81,5 | 329 |
| sugar | 0,0 | 0,0 | 99,7 | 398 |
| milk sauce | 2,0 | 7,1 | 5,2 | 84 |
Dairy | ||||
| milk | 3,2 | 3,6 | 4,8 | 64 |
| kefir | 3,4 | 2,0 | 4,7 | 51 |
| cream | 2,8 | 20,0 | 3,7 | 205 |
| sour cream | 2,8 | 20,0 | 3,2 | 206 |
| curdled milk | 2,9 | 2,5 | 4,1 | 53 |
Cheeses and cottage cheese | ||||
| cottage cheese | 17,2 | 5,0 | 1,8 | 121 |
Meat products | ||||
| boiled beef | 25,8 | 16,8 | 0,0 | 254 |
| beef liver | 17,4 | 3,1 | 0,0 | 98 |
| boiled beef tongue | 23,9 | 15,0 | 0,0 | 231 |
| boiled veal | 30,7 | 0,9 | 0,0 | 131 |
| rabbit | 21,0 | 8,0 | 0,0 | 156 |
Bird | ||||
| boiled chicken | 25,2 | 7,4 | 0,0 | 170 |
| turkey | 19,2 | 0,7 | 0,0 | 84 |
Eggs | ||||
| chicken eggs | 12,7 | 10,9 | 0,7 | 157 |
Fish and seafood | ||||
| black caviar | 28,0 | 9,7 | 0,0 | 203 |
| salmon caviar granular | 32,0 | 15,0 | 0,0 | 263 |
Oils and fats | ||||
| butter | 0,5 | 82,5 | 0,8 | 748 |
| ghee | 0,2 | 99,0 | 0,0 | 892 |
Non-alcoholic drinks | ||||
| mineral water | 0,0 | 0,0 | 0,0 | — |
| coffee with milk and sugar | 0,7 | 1,0 | 11,2 | 58 |
| black tea with milk and sugar | 0,7 | 0,8 | 8,2 | 43 |
Juices and compotes | ||||
| apricot juice | 0,9 | 0,1 | 9,0 | 38 |
| carrot juice | 1,1 | 0,1 | 6,4 | 28 |
| pumpkin juice | 0,0 | 0,0 | 9,0 | 38 |
| * data is per 100 g of product | ||||
Fully or partially limited products
- Products that increase secretion (broths, pickled vegetables, smoked and fried foods, alcoholic drinks, strong coffee and tea, carbonated drinks, spicy dishes, high-acid dairy products, sour fruits).
- Shchi, okroshka and borscht are excluded from the first courses.
- It is envisaged to exclude vegetables with coarse fiber (radish, turnip, cabbage, rutabaga, beans, peas), fruits with peel, and mushrooms, as a difficult-to-digest product. It is not allowed to consume sorrel, fresh dill, parsley and onions, as well as spinach due to the high content of organic acids and irritating essential oils.
- Products with connective tissue (skin, cartilage, veins).
- Irritating foods and dishes (cranberries, citrus juices and sour fruits, tomatoes, onions, peppers, garlic, ginger, chocolate, horseradish, mustard, meat sauces, tomato sauce, pepper).
- Pickled and pickled vegetables, canned vegetables - these products cause an increase in secretion.
- For a long time, difficult-to-digest cereals are excluded: millet, pearl barley, barley and corn.
- Legumes, fresh bread, kvass, yeast baked goods, which increase gas formation.
- Prohibited: fatty pork, animal fats, fatty fish, duck, lamb, goose, canned meat, canned fish and smoked meats.
- Fried and hard-boiled eggs, as they are difficult to digest and absorb.
- Any fresh bread, butter and puff pastry.
- Dried fruits and ice cream.
Table of prohibited products
| Proteins, g | Fats, g | Carbohydrates, g | Calories, kcal | |
Vegetables and greens | ||||
| vegetables legumes | 9,1 | 1,6 | 27,0 | 168 |
| swede | 1,2 | 0,1 | 7,7 | 37 |
| cabbage | 1,8 | 0,1 | 4,7 | 27 |
| sauerkraut | 1,8 | 0,1 | 4,4 | 19 |
| green onion | 1,3 | 0,0 | 4,6 | 19 |
| bulb onions | 1,4 | 0,0 | 10,4 | 41 |
| cucumbers | 0,8 | 0,1 | 2,8 | 15 |
| canned cucumbers | 2,8 | 0,0 | 1,3 | 16 |
| white radish | 1,4 | 0,0 | 4,1 | 21 |
| turnip | 1,5 | 0,1 | 6,2 | 30 |
| canned tomatoes | 1,1 | 0,1 | 3,5 | 20 |
| horseradish | 3,2 | 0,4 | 10,5 | 56 |
| spinach | 2,9 | 0,3 | 2,0 | 22 |
| sorrel | 1,5 | 0,3 | 2,9 | 19 |
Mushrooms | ||||
| mushrooms | 3,5 | 2,0 | 2,5 | 30 |
Cereals and porridges | ||||
| corn grits | 8,3 | 1,2 | 75,0 | 337 |
| pearl barley | 9,3 | 1,1 | 73,7 | 320 |
| millet cereal | 11,5 | 3,3 | 69,3 | 348 |
| barley grits | 10,4 | 1,3 | 66,3 | 324 |
Confectionery | ||||
| candies | 4,3 | 19,8 | 67,5 | 453 |
Ice cream | ||||
| ice cream | 3,7 | 6,9 | 22,1 | 189 |
Cakes | ||||
| cake | 4,4 | 23,4 | 45,2 | 407 |
Raw materials and seasonings | ||||
| mustard | 5,7 | 6,4 | 22,0 | 162 |
| ginger | 1,8 | 0,8 | 15,8 | 80 |
| ketchup | 1,8 | 1,0 | 22,2 | 93 |
| mayonnaise | 2,4 | 67,0 | 3,9 | 627 |
| ground black pepper | 10,4 | 3,3 | 38,7 | 251 |
| chilli | 2,0 | 0,2 | 9,5 | 40 |
Meat products | ||||
| pork | 16,0 | 21,6 | 0,0 | 259 |
| ham | 22,6 | 20,9 | 0,0 | 279 |
Sausages | ||||
| dry-cured sausage | 24,1 | 38,3 | 1,0 | 455 |
| sausages | 10,1 | 31,6 | 1,9 | 332 |
| sausages | 12,3 | 25,3 | 0,0 | 277 |
Bird | ||||
| smoked chicken | 27,5 | 8,2 | 0,0 | 184 |
| duck | 16,5 | 61,2 | 0,0 | 346 |
| smoked duck | 19,0 | 28,4 | 0,0 | 337 |
| goose | 16,1 | 33,3 | 0,0 | 364 |
Fish and seafood | ||||
| dried fish | 17,5 | 4,6 | 0,0 | 139 |
| smoked fish | 26,8 | 9,9 | 0,0 | 196 |
| canned fish | 17,5 | 2,0 | 0,0 | 88 |
Oils and fats | ||||
| animal fat | 0,0 | 99,7 | 0,0 | 897 |
| cooking fat | 0,0 | 99,7 | 0,0 | 897 |
Non-alcoholic drinks | ||||
| bread kvass | 0,2 | 0,0 | 5,2 | 27 |
| * data is per 100 g of product | ||||
Menu (Power Mode)
As indicated, nutrition for duodenal ulcers depends on the stage of the process. The longest diet during the period of recovery and remission, therefore the menu of Table No. 1 .
The physiologically complete composition of the diet (90-100 g of proteins, 100 g of fats and 420 g of carbohydrates) allows you to adhere to it constantly. In general, this is a healthy diet with sufficient vitamin and mineral composition, moderately sparing the gastrointestinal tract. Depending on the patient’s condition and the time that has passed since the exacerbation, dishes can be pureed or not pureed. This question should be clarified by the doctor.
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
| Breakfast |
|
| Lunch |
|
| Dinner |
|
| Afternoon snack |
|
| Dinner |
|
| For the night |
|
Completeness of the diet
On a note
When prescribing a diet, it is extremely important to take into account the nature and stage of the disease, the condition of other organs and systems.
If the diet is used for a long time, it is necessary to take care of the completeness of the diet. And with this, “Diso®” “Nutrimune” will provide invaluable assistance, which compensates for the protein component of the diet without overloading the gastrointestinal tract.
"Diso®" "Nutrimune" helps to compensate for protein deficiency in dietary nutrition and does not put additional stress on the digestive system.
The product is odorless and does not affect the usual taste and consistency of dishes. It can be added to soups, porridges, jelly and other dishes at any stage of preparation.
Diet recipes
During different periods of the disease, the cooking technology differs. If mucous soups are recommended for severe inflammation (they are used in Diets 1A and 1B ), then pureed soups are the basis of Table No. 1 and are recommended during the recovery period.
Mucus soups are the most gentle and are strained decoctions of cereals (without the cereals themselves), which are salted and butter is added (sometimes seasoned with an egg-milk mixture). When preparing pureed soups, all ingredients are pureed, the soup is salted and oil is added while it is warm. Cereal milk soups are prepared in the same way (the ratio of water and milk is 1:1, the cereal is pureed). Below are the recipes for the first table dishes.
First meal
Milk soup with turkey meat and croutons
Boiled turkey meat is passed through a meat grinder and further pureed to a puree. The broth (oatmeal or rice) is mixed with puree, salted to taste and boiled. After cooling to 80°C, season with milk and cream (1:1). Additionally, you can add a beaten egg and bring to a boil.
Pumpkin and cauliflower soup
Place the vegetables in a saucepan, add a small amount of water and boil. When warm, rub together with the broth. Prepare a white sauce based on milk, flour and eggs. White sauce is added to the vegetable puree, salted, diluted with milk or vegetable broth to the desired consistency and brought to a boil. You can add a piece of butter to the finished soup.
Second courses
Fish pudding with green peas
The fish fillets are boiled and wiped. Add butter, egg yolks, mix well and salt. Add whipped whites to the prepared fish mixture in several additions, stirring gently. The mass is poured into a mold and steamed.
Beef soufflé
The boiled beef is minced several times. Milk sauce, butter, egg yolks and salt are added to the finished meat puree. Beaten egg whites are added to the resulting mass. Place in a mold and steam.
Dessert
Apple and carrot pudding
Sliced carrots are simmered in a saucepan with a small amount of water. After 10-15 minutes, add chopped apples and simmer until everything is ready. The mass is rubbed, milk and semolina are added, and boiled for 1-2 minutes. Separately beaten yolks and whites are added to the cooled mass. Place in a mold and bake in a slow cooker or oven without forming a rough crust.
How to choose kefir for stomach or intestinal ulcers
For gastrointestinal diseases, it is important to drink the product fresh, 1-2 days after production.
This drink contains a maximum of useful substances, without alcohols or fermentation components. When choosing in a store, it is important to take into account the release date and the number of lactic acid bacteria (at least 107 CFU per 1 g). A quality product contains only milk and sourdough. A shelf life of more than 7 days indicates the presence of preservatives. It is advisable to choose kefir in glass containers or tetrapacks. When packaged in plastic packaging, many useful substances are lost. Recommended fat content of the product is 2.5%. A low-fat drink contains fewer beneficial elements. It may contain components undesirable for ulcers. Products with a higher percentage complicate the digestion process.
At home, kefir can be made according to this recipe:
- Boil skim milk (1 l) and cool to 40 ºC.
- Strain into a sterilized enamel container.
- Add 1 g of starter or 1 tsp. sour cream (5-10%).
- Stir with a small plastic or wooden spatula.
- Close the bowl, wrap it in a blanket and place it in a warm place.
- In a day the product is ready.
- Store the drink in the refrigerator and consume within 1-2 days.
Reviews and results
This dietary food is prescribed for a long period, since it is balanced, and the diet is significantly expanded compared to Diets No. 1A and 1B . This allows you to eat a varied diet without feeling deprived. Reviews from patients indicate the positive impact of such nutrition on the gastrointestinal tract: pain, belching, heartburn , bitterness in the mouth disappear, and intestinal bloating does not bother you. For some, pain in the pancreas and bowel disorders associated with pancreatitis disappear.
- “...I have had duodenal ulcer for many years. When it was first detected, I was treated well in the hospital, after which there were no exacerbations, and if there were, they were not severe and without the formation of a “new ulcer.” It’s just that in the fall or after nervous stress, sucking pain appears in the stomach area. This is a signal that you need to drink De-nol, Lansoprozole for 2 weeks and switch to proper nutrition. In such cases, I manage without a hospital. I maintain the diet well for 3-4 weeks, and then I switch to regular food, but without spicy, smoked or fried foods. I like steamed cutlets made from different types of meat and poultry - they are not completely tasteless, since my wife adds a little grated onion and dried dill to them (this does not cause pain or other discomfort). I eat soups in water without spices or frying. These are mainly cereal soups with well-cooked or crushed cereals. I eat all the cereals, mashed potatoes, and pureed vegetable supplements. Already in the second week the stomach calms down. In a month of eating this way, I lose a little weight”;
- “... Several years ago there was a perforated ulcer, but it was not very complex, so we operated on it using the endoscopic method. I recovered quickly after this operation, but I had to follow the diet for a long time, and I also took medication for about a month. At first I ate everything pureed for a month, and then I switched to the first table that was not pureed. I adhered to it very strictly for six months, although after a month nothing bothered me, and only 3 scars reminded me of the operation. During these six months, I got used to cooking dishes in a double boiler and a slow cooker, added new recipes to the list, and the food did not seem monotonous and boring. The dietary restrictions affected my weight—I lost 5 kg. I hope to continue to adhere to a healthy diet - the perforation really scared me”;
- “...Frequent exacerbations of ulcers occur once every two years. I think this is due to smoking, irregular meals (and even dry food) and business trips. It is clear that far from home there is no opportunity to eat properly. So it turns out that I periodically end up in the hospital. There they immediately assign Table 1B, and after 2 weeks - the main table for stomach patients.”