A thickening of the pancreas can be detected during an ultrasound examination and indicates changes in the tissues of the organ that have developed as a result of pathology. The detected compaction of the structure is not a symptom of the disease - it is only an objective confirmation of a previous or currently existing disease. Therefore, such a phenomenon has no diagnostic significance. In most cases, deviations from the norm in tissue density on ultrasound are visualized not at the first consultation, when the patient complained of a worsening condition, but much later, after treatment.
Diffuse changes in the pancreatic parenchyma
The pancreas is a large organ of internal and external secretion. It is located on the posterior abdominal wall in the retroperitoneal zone, consists of a head, body, tail, and is partially covered in front by the stomach. In the thickness of the pancreas there is a duct directed from the tail to the head. The gland produces pancreatic juice, which contains enzymes that help digest proteins, fats and carbohydrates.
The pancreas tissue contains endocrine glands that produce insulin for the absorption of glucose. A healthy pancreas has homogeneous tissue and large contours. The cause of diffuse changes in the parenchyma of the pancreas, according to doctors, is acute and chronic pancreatitis and elevated blood sugar levels.
Often, diffuse changes in the pancreatic parenchyma are diagnosed in elderly people with various problems of the cardiovascular system, diseases of the liver and biliary tract, and digestive tract organs. The cause of changes in the parenchyma of the pancreas can also be infectious and inflammatory diseases of internal organs that contribute to metabolic disorders.
What will the transcript of an abdominal ultrasound show?
July 24, 2016 Ultrasound examination
First, let's look at what this ultrasound shows.
Behind the anterior wall of the abdomen there is a large space - the abdominal cavity. There are quite a few organs located in it, which an ultrasound of the abdominal cavity will show. This:
- stomach
- intestines
- pancreas
- liver
- bile ducts: intra- and extrahepatic
- spleen
- gallbladder
- kidneys
- adrenal glands
- abdominal part of the aorta and its branches
- lymph nodes
- lymphatic trunks and vessels
- division of the autonomic nervous system
- nerve plexuses.
The abdominal cavity is lined with two layers of a thin membrane - the peritoneum. It is this inflammation that is called peritonitis and is a life-threatening condition. The organs are covered in different ways by the peritoneum: some are wrapped in it, some do not even touch it, but are located within the boundaries outlined by it. Conventionally, the cavity is divided into the abdominal cavity itself and the retroperitoneal space. The latter includes the bottom of the list of organs, starting with the kidneys.
All these organs - both the abdominal cavity and the space behind the peritoneum - are examined during an ultrasound examination of the abdominal cavity. This study can detect the presence of structural damage, inflammation, pathological formations, enlargement or reduction of the organ, and disruption of its blood supply. Ultrasound does not see how a sick or healthy organ copes with its functional responsibilities.
What does ultrasound give? The study helps to find the cause of the disease in such cases:
- pain or discomfort in the abdomen
- bitterness in the mouth
- feeling of a full stomach
- intolerance to fatty foods
- increased formation of gases
- frequent bouts of hiccups
- feeling of heaviness in the right or left hypochondrium
- jaundice
- high blood pressure
- lower back pain
- fever not due to a cold
- weight loss not related to diets
- belly enlargement
- as control over the effectiveness of treatment of pathologies of the digestive system
- and also as a routine examination, including for existing anomalies of organ development, cholelithiasis.
Pathology determined by ultrasound
What does abdominal ultrasound diagnose? Using this study, the following diseases can be identified:
1. From the gallbladder side:
- acute and chronic cholecystitis
- empyema of the bladder
- gallstone pathology
- during a choleretic breakfast, the motor function of the bladder can be assessed
- developmental anomalies (kinks, septa).
2. From the liver:
- cirrhosis
- hepatitis
- abscesses
- tumors, including metastases
- hepatosis
- "stagnation" in the liver due to cardiopulmonary diseases
- fatty liver change.
3. From the kidneys and urinary system:
- kidney tumors
- "wrinkled bud"
- pyelonephritis
- narrowing of the ureters
- stones and “sand” in the kidneys.
4. From the side of the spleen, ultrasound of the abdominal cavity reveals:
- cysts
- tumors
- abscesses
- heart attacks
- organ enlargement in infectious and parasitic diseases
5. From the pancreas:
- cysts
- tumors
- abscesses
- stones in the ducts
- signs of acute and chronic pancreatitis.
6. Ultrasound reveals free fluid in the abdominal cavity
7. From the abdominal part of the aorta or its branches, an aneurysm and its dissection, vasoconstriction may be visible
8. From the side of the retroperitoneal lymph nodes, their enlargement and homogeneity of structure are visible
How to understand the research results
To do this, consider the ultrasound form (protocol). It indicates points that relate to each organ separately.
Liver
Interpretation of abdominal ultrasound in relation to this organ includes:
| Parameter | What is written on the form | Normal ultrasound findings in adults |
| Dimensions of the entire organ | Normal, decreased, increased (underline as appropriate) | Norm |
| right | The numbers are indicated in cm for each item | Up to 12.5 |
| left | Up to 7 | |
| caudate | 30-35 | |
| Oblique-vertical dimension (OVR) of the right lobe | Numbers in mm | Up to 150 mm |
| Outlines | It is emphasized whether they are even or not | Smooth |
| Capsule | It is emphasized whether it is differentiated or not, thickened or not | Differentiated, not thickened |
| Left lobe thickness | Number in mm | 50-60 |
| Right lobe thickness | 120-125 | |
| Echostructure of parenchyma | Emphasized, normal, increased or decreased | Norm |
| Focal formations | Yes or no | Must not be |
| Portal vein | Size in mm | Up to 14 mm |
| Vascular pattern | Depleted, normal or enhanced | Ordinary |
| Inferior vena cava | Size in mm | Anechoic, diameter 20 mm |
| Hepatic veins of the first order | Size in mm | Up to 1 mm |
Decoding the results
- Fatty hepatosis is indicated by an increase in the echo density of the organ in the form of small foci. The edge of the liver is rounded. In the final stages, due to compaction of the organ, it is impossible to see the portal vessels.
- With cirrhosis of the liver, its enlargement and dilation of the portal and splenic veins are visible. The lower edge of the organ will also be rounded, the contours will be uneven. The increase in echo density in this case will be large-focal. Free fluid in the abdominal cavity (ascites) is also determined.
- If an increase in size, rounding of the edges, as well as expansion of the vena cava and the absence of narrowing during inspiration are described, this indicates congestion in the liver due to cardiac or pulmonary disease.
- If lesions are described in which there is a violation of the normal echostructure, this may indicate malignant or benign tumors, cysts or abscesses.
In the video, a specialist talks about errors that occur during ultrasound examination of the abdominal organs.
Gallbladder
Ultrasound norm based on the results of examination of this organ:
- Shape: various – pear-shaped, cylindrical.
- Dimensions: width 3-5 cm, length 6-10 cm.
- Volume: 30-70 cubic meters cm.
- Walls: up to 4 mm thick.
- Formations in the lumen: normally there are none.
- Acoustic shadow from formations: this applies to stones and bladder tumors. Based on the presence of this shadow, the types of stones are deciphered (they come in different compositions).
- Whether they move or not: the stones are usually movable, but can be soldered to the wall or be large in size. Based on this and some other signs, one can judge whether the formation is a tumor.
Signs of gallbladder pathology
- In acute cholecystitis, thickening of the organ wall is noted, and the dimensions can be normal, reduced or enlarged. The wall may also be described as a "double contour" and the presence of fluid around the bladder indicates that local peritonitis has already developed and urgent surgery is needed.
- Thickening of the wall will also occur with chronic cholecystitis. The contour in this case is clear and dense.
- In conclusion, various deformations of the organ can be described. This is not a disease, but a structural feature.
- If echo-negative objects are described that leave an acoustic shadow, while the wall of the bladder is thickened and the contour is uneven, we are talking about calculous cholecystitis. In this case, the expansion of the bile ducts indicates that the stone is blocking the exit of bile.
Interpretation of ultrasound of the bile ducts
Normally, on ultrasound, the bile ducts have the following characteristics:
- common bile duct: diameter 6-8 mm
- intrahepatic ducts: should not be dilated
Norms of the pancreas on ultrasound
- There should be no additional education.
- head: up to 35 mm
- body: up to 25 mm
- tail: about 30mm
- contour: smooth
- echostructure: homogeneous
- echogenicity: neither reduced nor increased
- Wirsung duct: 1.5-2 mm
- education: normally there are none.
A decrease in the echo density of the gland indicates acute pancreatitis, an increase in it indicates chronic pancreatitis or cancer. The expansion of the Wirsung duct also indicates chronic inflammation. The “favor” of cancer is indicated by a segmental increase in size and unevenness of the contour of the gland, depression on the surface of the liver, as well as displacement or compression of the inferior vena cava or aorta.
Interpretation of ultrasound of the spleen
- Dimensions: length – up to 11 cm, thickness – up to 5 cm, longitudinal section – up to 40 sq. cm
- splenic index: no more than 20 cm2
- structure: normally – homogeneous
- splenic vein at the hilum.
- You can see an increase in the size of the organ. This is associated with both certain blood diseases and liver diseases (such as cirrhosis) or infectious diseases.
- Densified (less often, less dense) tissue indicates a splenic infarction, that is, that as a result of thrombosis or injury, the death of some part of the organ occurred.
- Ultrasound also allows you to see a rupture of the spleen, which usually occurs either with a severe injury or with a minor bruise, but in the case of an enlarged organ.
Ultrasound of hollow organs (stomach, small, large and rectal intestines)
It only indicates whether there is a symptom of an “affected organ” (there should not be one) and whether there is fluid deposition in the intestinal lumen (this should not happen either).
If an ultrasound scan of the kidneys was also performed, then a description of this organ is also included in the conclusion of the study. The results of an ultrasound examination of the kidneys are normal:
- width: 5-6 cm
- length – about 11 cm
- organ thickness: 4-5 cm
- kidney parenchyma - no more than 23 mm thick
- the pelvis should not be dilated
- There should be no structures in the lumen of the pelvis and ureters.
Lymphatic structures with ultrasound imaging
Ultrasound of the retroperitoneal lymph nodes normally suggests the following conclusion: “Lymph nodes are not visualized.” That is, if they are of normal size, ultrasound “does not see” them. An increase in these immune organs indicates either an infectious disease present in the abdominal cavity or a malignant formation. In the latter case, they can increase due to the fact that cancer cells of the hematopoietic system “live” in them, as well as with metastases of any nearby organ tumor.
Sonologist's conclusions
At the conclusion of the ultrasound, the sonologist (ultrasound doctor) indicates the presence of pathology: he describes what the echo signs look like. If in the referral the doctor indicates that it is necessary to conduct an examination for some disease, but the ultrasound did not visualize it (for example, calculous cholecystitis), then there may be the phrase “Echo signs of the disease were not identified.” The final diagnosis is made only by the doctor who refers you for examination.
Who needs to undergo Doppler ultrasound of the abdominal vessels
This examination, which is also called Doppler ultrasound (Doppler ultrasound) of the abdominal vessels, is often performed together with ultrasound. The patient's sensations are not differentiated and are not more harmful than ultrasound. It allows you to evaluate the anatomy and characteristics of blood circulation in vessels such as:
- abdominal aorta
- common hepatic artery
- iliac arteries
- celiac trunk
- splenic artery
- superior mesenteric artery
- portal vein of the liver and its branches
- inferior vena cava.
Ultrasound of the vessels of the abdominal cavity makes it possible to timely identify early abnormalities in the vessels, identify and evaluate the degree of increase in pressure in the portal vein (with cirrhosis, “congestive” liver), and evaluate the result of implantation of a vena cava filter.
Ultrasound of the abdominal aorta and its branches helps in the diagnosis of:
- fainting states
- frequent headaches
- epileptic seizures
- high blood pressure
- repeated strokes (sometimes blood clots can “fly off” from this large vessel)
- leg pain
- potency disorders
- aortic aneurysm
- atherosclerotic lesions
- vasoconstriction
- anomalies in the development of large vessels.
Duplex scanning
Vascular examination during ultrasound using modern equipment almost always includes duplex angioscanning. This is the “gold standard” in assessing blood circulation in the venous vessels. It allows you to identify pathological blood flow, obstructions to blood flow, assess their location, extent and severity.
With this type of study, the sonologist receives a color two-dimensional image of the abdominal vessels, where red indicates the movement of blood towards the sensor, and blue, on the contrary, away from the sensor. Based on the intensity of the red and blue colors, the doctor draws conclusions about the speed of blood flow in any part of the vascular system.
Additional Study Details
Reviews about ultrasound are mostly positive: the study is painless, harmless, and very informative. The negative point is that before the procedure you need to carefully prepare so that gases in the intestines (“flatulence phenomena”) do not interfere with the correct diagnosis.
How much does it cost to conduct this research? A complete examination of all organs (including the kidneys and urinary system) with duplex angioscanning is estimated by clinics at an average of 2000-2500 rubles. An examination of individual organs with an assessment of the blood flow in them costs about 800-1000 rubles.
Thus, interpretation of abdominal ultrasound should be carried out by a specialist, taking into account not only the “norm” numbers, but also based on clinical manifestations. The above values will help you understand a little about the pathology identified in you, but the final assessment should be given by a specialist therapist or gastroenterologist.
We also looked here: ultrasound of the abdominal cavity, interpretation is normal, they don’t see fluid on ultrasound, form for ultrasound of gastrointestinal organs, splenic vein is normal in adults
← All articles
Increased echogenicity of the pancreatic parenchyma
When performing ultrasound diagnostics, you can find out the density of internal organs. If decreased or increased echogenicity of the pancreas is detected, then this is a serious reason to undergo an extensive examination, providing an accurate diagnosis and determining methods for eliminating problems.
Increased echogenicity of the pancreatic parenchyma is detected during inflammation with the formation of fibrosis, which develops against the background of metabolic disorders, when healthy parenchyma tissue is replaced by fat, during acute pancreatitis and relapse of chronic inflammation that changes the density of the parenchyma.
The absorption coefficient of ultrasonic radiation depends on the increased echogenicity of the parenchyma. Malignant tumors that form in the parenchyma have a higher absorption coefficient of ultrasonic energy than benign tumors.
Methods for eliminating seals
Seals discovered during examination during the period of remission of the inflammatory process, when the patient does not complain and there are no changes in biochemical tests of blood and urine, do not require treatment. No methods have been found for restoring pancreatic cells that died during necrosis and were replaced by connective tissue. All changes in the pancreatic parenchyma that arose as a result of pathology, especially if it is associated with the disintegration of normal pancreatic cells, are irreversible.
When densified areas are identified, treatment should be aimed at preventing the further spread of these processes and maximizing the restoration of lost functions if this occurs. For this purpose, conservative treatment methods are used.
If compactions are detected that indicate the presence of neoplasms, surgical intervention may be necessary in severe cases.
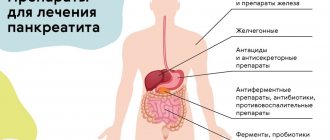
Therefore, comprehensive treatment includes:
- lifestyle modification;
- dietary nutrition;
- drug therapy;
- surgical methods (in severe cases).
Conservative treatment
Conservative therapy includes the use of medications and dietary nutrition. If food restrictions can be prescribed for a long period, sometimes for life, then drug therapy is used during the period of exacerbation. After suffering acute pancreatitis with massive necrosis or with frequent exacerbations of chronic inflammation in the gland, the patient may need constant enzyme replacement therapy. In such cases, the dose, frequency and duration of administration are prescribed by a gastroenterologist: he also monitors and adjusts the treatment.
Antihyperglycemic drugs are also prescribed for continuous use if diabetes mellitus develops due to the death of the islets of Langerhans, the beta cells of which produce insulin. The patient is observed by an endocrinologist, prescribes a diet and medications, which only he can stop or reduce the dose after the next examination.
There is no etiological and pathogenetic treatment for pancreatic diseases. Symptomatic therapy is prescribed. It is carried out taking into account complaints and biochemical studies. Such treatment, in addition to enzymes and glucose-lowering drugs, includes:
- Antispasmodics, anticholinergics, analgesics in the presence of a pain symptom and its severity.
- Antisecretory agents with different mechanisms of action.
From the group of antisecretory drugs the following are used:
- PPIs (proton pump inhibitors);
- H2-histamine receptor blockers;
- antacids.
Therapy for the underlying pathology is also prescribed, which is identified by clarifying complaints, anamnesis, objective examination and functional methods.
In case of acute pancreatitis or exacerbation of chronic pancreatitis, treatment is carried out in a hospital, starting in the intensive care unit, where additional infusion solutions, antienzyme agents, and narcotic analgesics are used.
Operating methods
In cases of compactions identified during sonography of the pancreas, surgical methods of treatment of the pancreas are indicated in the presence of:
- neoplasms;
- stones;
- huge cysts.
They compress organ tissues and cause changes in their structure. Therefore, radical treatment is also indicated if conservative therapy for these changes is ineffective at the previous stages.
Surgical methods stabilize the pathological process - slow down the progression of chronic pancreatitis. According to statistics, 40% of patients with chronic pancreatitis (CP) become patients in the surgical department of a hospital due to refractoriness to therapeutic treatment and developing complications. Taking into account that there are no clinical manifestations of diffuse transformations of pancreatic tissue at the time of their visualization on sonography, treatment is limited to diet and the elimination of harmful factors and habits.
Consolidation of the pancreatic parenchyma
Methods for studying the parenchyma of the pancreas include questioning and examination of the patient, laboratory, instrumental and radiological methods. Compaction of the parenchyma can be a consequence of various diseases of the pancreas.
Symptoms include pain in the epigastric region and left hypochondrium, disorders of the digestive system that cause a person to feel discomfort, general weakness, and severe weight loss. The appearance of compaction of the parenchyma of an organ has a certain influence on the diet and nature of nutrition, the presence of cholelithiasis, cholecystitis, and cystic fibrosis.
What types of cancer can occur in the head of the pancreas?
In 60–70% of cases, pancreatic cancer occurs in the head of the pancreas. More than 80% of tumors are adenocarcinomas . They develop from cells that line the ducts of the gland.
Less common are cystic tumors . In most cases, pancreatic cysts are benign, but in some cases they contain cancer cells. A biopsy helps establish an accurate diagnosis.
If the tumor originates from cells that produce the enzyme, it is called acinar cell carcinoma . It is usually diagnosed at a younger age, grows slowly and has a better prognosis.
Tumors of endocrine cells are rare: insulinomas, glucagonomas, gastrinomas, somatostatinomas.
Heterogeneous structure of the pancreatic parenchyma
The pancreas of a healthy person has a homogeneous structure, equal echogenicity, clearly visible contours, an uncinate process, correct position and normal dimensions of the head and tail. Deviation from the norm is determined by an increase in the size of individual parts of the pancreas and the heterogeneity of the structure of its tissues.
Heterogeneity of the pancreas is evidence of the presence of various diseases, including pancreatitis and diabetes mellitus. This pathology can be found in any part of this organ. Diffuse heterogeneous changes can be caused by edema, inflammation and the formation of pseudocysts.
Reactive changes in the pancreatic parenchyma
Reactive changes in the parenchyma are a consequence of inflammation of the pancreas due to the aggressive effect of the liver and gallbladder on it. This causes pain, dyspepsia and increased blood sugar and occurs because the glandular tissue of the parenchyma with a reactive pancreas produces pancreatic juice and hormones in insufficient quantities. One of the most common causes of reactive changes in the parenchyma can be an allergic reaction.
Diffuse changes in an important organ contribute to a reactive change that spreads evenly throughout the pancreas without the presence of local foci indicating neoplasms or stone formation. Treatment of this pathology is one of the pressing issues of modern gastroenterology.
The combination of medications prescribed by the attending physician and properly organized nutrition can prevent the development of various complications. It must be remembered that timely contacting a doctor and carefully following the instructions can be a guarantee of successful treatment.
Author of the article:
Mochalov Pavel Alexandrovich |
Doctor of Medical Sciences therapist Education: Moscow Medical Institute named after. I. M. Sechenov, specialty - “General Medicine” in 1991, in 1993 “Occupational diseases”, in 1996 “Therapy”. Our authors
Diet and prevention of seals
In order to prevent further development of pathological tissue compaction, atrophy of the gland and the final decline in its functions, dietary nutrition is prescribed, which is an important part of therapy. Sometimes, when not all parenchyma has undergone changes, a strict diet prescribed by a doctor can stabilize the condition and improve well-being. Gross violations, and sometimes minor errors in nutritional therapy can lead to another relapse.
If a specialist considers following a diet mandatory, these recommendations cannot be neglected!
If pancreatitis is detected with concomitant pathology of other digestive organs, dietary table No. 5p according to Pevzner is used. There are several of its varieties, which are developed taking into account the stage of the disease, the activity of the process, the severity of the patient’s condition, and concomitant diseases. The general principles of therapeutic nutrition for changes in the pancreas boil down to a categorical prohibition of fried, fatty, spicy, smoked, salty, various seasonings and flavor enhancers. Must be observed:
- fragmentation and frequency of meals: small portions 5-6 times a day during an exacerbation, during remission - 4-5 times a day;
- mandatory full lunch with first course and light late dinner;
- cooking food by stewing, boiling, baking, steaming;
- food must be crushed to reduce the functional load on the pancreas;
- comfortable temperature - excessively hot or cold food is not recommended, it should be warm so as not to irritate the mucous membranes;
- compliance with the prescribed caloric intake - when drawing up a menu and preparing food, use special tables indicating the energy value of products (meals must be complete, using a sufficient amount of proteins and include vegetables and fruits in chopped and processed form), as well as a list of prohibited and partially restricted use .
Prevention of pathological transformation of pancreatic tissue is lifestyle changes:
- complete abstinence from alcohol;
- to give up smoking;
- reduction of chronic stress and fatigue;
- active lifestyle;
- healthy nutritious diet with the exception of harmful foods.