The female body is fraught with many mysteries. Both pleasant and not so pleasant. The latter, perhaps, includes menstruation, which “give” several days of discomfort to the fair sex. Menstruation is not limited only to pain in the stomach and joints, sudden changes in mood, and acne on the face. It can also be accompanied by diarrhea, which affects about a third of women of childbearing age.
Menstrual irregularities as a cause of loose stools
Menstruation is accompanied by complex biochemical processes that affect the functioning of the nervous system, internal organs and the condition of the body as a whole. Failure in these processes leads to painful menstruation (dysmenorrhea)1,2 and often causes diarrhea during menstruation.
According to some data, up to 80% of women experience dysmenorrhea to one degree or another at different periods of life1. Some of them may experience diarrhea during menstruation. In 30% of cases, painful symptoms lead to disability within 1-5 days1.
The development of painful manifestations of dysmenorrhea is facilitated by:
- heavy physical activity1;
- sedentary lifestyle2;
- complicated heredity (every third woman with dysmenorrhea suffered from the same menstrual cycle disorder)1;
- smoking, regardless of the number of cigarettes smoked2;
- adverse effects of the external environment (hypothermia, overheating)2;
- infections2;
- stressful situations1,2.
Up to contents
Constipation after menstruation
If menstruation has ended and stool retention persists, this may be due to residual effects of a lack of sex hormones. During this period, the pressure of the pelvic organs on the intestines is minimal, the uterus takes on normal dimensions. However, peristalsis may remain insufficient, and the situation is aggravated by a lack of fluid. In the first days of the menstrual cycle, retained fluid begins to be eliminated from the body. If you do not replenish the water deficit, the contents of the intestines become denser, and feces have difficulty moving through the intestines - this is how constipation appears after menstruation.
Why does diarrhea occur with dysmenorrhea?
The mechanisms that trigger the development of diarrhea may be different in each case and largely depend on the type of dysmenorrhea.
Primary dysmenorrhea develops as an independent disease, and its causes are not fully understood. Currently, most researchers associate the development of primary dysmenorrhea with high levels of prostaglandins.
Problems arise at the biochemical and functional level:
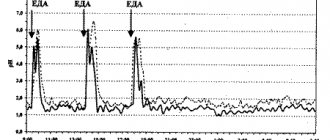
- In the menstrual endometrium, the synthesis of prostaglandins, which trigger an inflammatory response, increases1,2. They increase the contractile activity of the uterus (2-2.5 times1), which, in turn, leads to the appearance of spasms in the lower abdomen1,2.
- Prostaglandins extend their influence throughout the body, including the intestines1. Its contractions lead to accelerated movement of intestinal contents and slower reabsorption of water and electrolytes from the intestines into the blood. As a result, diarrhea occurs during menstruation1,2.
The cause of secondary dysmenorrhea is various female diseases. Most often it is 1,2:
- endometriosis;
- ovarian dysfunction, manifested by hormonal imbalance and menstrual irregularities;
- inflammatory diseases of the internal genital organs;
- fibroids (with the growth of nodes towards the uterine cavity);
- polyps of the inner lining of the uterus (endometrium) or cervical canal;
- abnormalities of the uterus (saddle-shaped, bicornuate uterus);
- intrauterine synechiae (adhesions in the uterine cavity);
- varicose veins of the pelvic veins and other diseases1,2.
All these diseases are accompanied by difficulty in emptying the uterus of menstrual blood, a sharp increase in the level of prostaglandins2, which provokes not only cyclic pain, but also the occurrence of diarrhea during menstruation2,3.
Up to contents
What symptoms accompany diarrhea with dysmenorrhea?
Symptoms of dysmenorrhea can develop 1-2 days before the start of menstruation1, so diarrhea may begin before, rather than during, your period.
With the onset of menstrual bleeding, discomfort usually intensifies, and at the end of menstruation it weakens or disappears completely1,2.
In addition to diarrhea, during “critical” days the following may be observed:
| Drawing, aching, bursting or cramping pain in the lower abdomen, radiating to the rectum, lower back, groin | They usually appear 12 hours before menstrual bleeding and subside within the first 2-42 hours after it begins3. When dysmenorrhea is combined with irritable bowel syndrome (IBS), abdominal cramps typical for this condition are added along the colon3,4 |
| Changes in the emotional and mental sphere | Drowsiness during the day and insomnia at night, decreased mood, increased or decreased appetite, up to bulimia or anorexia. Pain and diarrhea during menstruation aggravate emotional discomfort, enhance each other’s symptoms and thereby close a vicious circle2,3,4 |
| Autonomic and vegetative-vascular reactions | Dry mouth, nausea, belching, headaches, dizziness, hot flashes, sweating, chills, increased heart rate and urination, bloating and rumbling in the stomach1,2 |
| Metabolic-endocrine symptoms | Severe muscle weakness, feeling of “woolly” legs, itchy skin, aching joints and swelling associated with impaired electrolyte metabolism1 |
Up to contents
Irritable bowel syndrome and dysmenorrhea
Stress, mental and physical overload, which disrupt the adaptation of the nervous system to cyclical changes in the reproductive and endocrine systems, lead not only to dysmenorrhea, but also to an exacerbation of irritable bowel syndrome (IBS)2,3,4.
Women prone to hypochondria, depressive and anxiety disorders often suffer from menstrual irregularities in combination with IBS4, which means they are more likely to experience diarrhea before and during menstruation.
IBS is a functional intestinal disorder, manifested by diarrhea, constipation, or a combination of both3,4. On critical days, when strong contractions of the uterus provoke increased intestinal motility, manifestations of diarrhea prevail over stool retention4.
Symptoms of IBS during menstruation:
- abdominal pain (mandatory sign)4, from “spread” dull to acute spastic;
- stool more than 3 times a day, mainly in the morning and afternoon;
- thin, watery stool;
- an admixture of mucus in the stool (possibly);
- uncontrollable urge to defecate4.
In some women, dysmenorrhea may be an additional manifestation of IBS4.
Up to contents
Constipation before menstruation
Premenstrual syndrome, familiar to every fifth woman under the age of 29, as well as every second woman over 30 years old, is characterized by a whole complex of symptoms. From the gastrointestinal tract, constipation and flatulence are most often observed. Such manifestations are caused not only by a decrease in diuresis (fluid stagnation in the tissues), but also by changes in muscle activity. Most women notice increased appetite and thirst 3 days - 14 days before the onset of menstruation, so there is a high probability of a diet violation.
Eating large amounts of food or foods that are not part of the usual diet, disrupting the usual diet may be additional risk factors for constipation. It is important to keep your appetite under control and adhere to the principles of a healthy diet and eat healthy sweets.
Get rid of intestinal problems
The natural British drug is not addictive and works immediately
Find Fitomucil with benefits
Diagnostics
IBS may be suspected if bowel problems occur for at least 12 weeks in the past 12 months3. Since diarrhea can be a manifestation of other diseases, if symptoms recur, you should consult a doctor and undergo an examination, including ultrasound of the abdominal organs, colonoscopy, sigmoidoscopy and irrigography.
To understand why diarrhea during menstruation is accompanied by disruption of the reproductive system, you need to consult a gynecologist. Identifying the causes will help you choose the right treatment and cope with the problem.
Urgent consultation with a doctor is required in the following cases:
- Severe abdominal pain, accompanied by tension in the anterior abdominal wall (possibility of acute surgical illness, for example, peritonitis).
- Frequent watery stools, which are accompanied by nausea, vomiting, thirst, dry visible mucous membranes, and fever (possible signs of an intestinal infection).
- The appearance of scarlet and dark blood in the stool (a symptom of intestinal bleeding).
Up to contents
How to choose a laxative
Constipation can be managed before, during or after menstruation with mild laxatives. It is better to avoid enemas and senna-based medications - these measures can have a bad effect on the gastrointestinal tract, cause dysbiosis or chronic constipation. Be sure to consult your doctor and tell us about your problem. The specialist will select mild medications for the prevention and treatment of constipation.
An excellent drug for the prevention and treatment of constipation is the English remedy “Fitomucil Norm”. It includes natural ingredients - plant fiber. Insoluble dietary fiber promotes normal intestinal motility, while soluble fiber becomes a soft gel that facilitates the passage of stool. This remedy does not cause painful cramps and bloating, which is important during menstruation. The drug is not addictive and can be used as a preventive measure. The remedy can be taken even before constipation occurs.
Bibliography
- Yakovleva E. B., Babenko O. M., Pilipenko O. N. Premenstrual syndrome.
- Tumarenko A.V., Skvortsov V.V. Modern approaches to pharmacotherapy of constipation.
- Minushkin O. N., Elizavetina G. A., Ardatskaya M. D., Kolkhir V. K., Voskoboynikova I. V., Shindina T. S. Functional constipation: ideas, therapeutic approaches.
What to do if you regularly have diarrhea during menstruation
Considering the large role of psycho-emotional factors in the development of dysmenorrhea and IBS, doctors recommend:
- Normalize your work and rest schedule, sleep at least 7-9 hours a day.
- Learn relaxation techniques and meditation.
- Avoid heavy physical activity before menstruation, stick to light exercises, yoga, and gymnastics.
- On the eve of menstruation, exclude from the diet foods that irritate the intestines and cause increased gas formation: products made from yeast dough and whole milk products, fresh vegetables and fruits, eggs and legumes, coffee and carbonated drinks, spicy, fatty, fried and spicy foods, canned food, smoked and marinades3,4.
- As one of the methods for treating recurring diarrhea during menstruation, doctors use physiotherapeutic procedures: climatotherapy, hydrotherapy, balneotherapy, light and electrotherapy, hyperbaric oxygenation, massage, acupuncture, acupressure and others5.
- To normalize stool during diarrhea, you can use the drug IMODIUM® Express based on loperamide6. Loperamide reduces intestinal motility, slows down the movement of intestinal contents, promotes the reabsorption of water and electrolytes from the intestine into the blood, and fecal retention7.
The information in this article is for reference only and does not replace professional advice from a doctor. To make a diagnosis and prescribe treatment, consult a qualified specialist.
Literature
- Prilepskaya V.N., Mezhevitinova E.A. Dysmenorrhea. Regular issues of "RMZh" No. 3 dated 02/04/1999, p. 6.
- Jobava E.M., Mandrykina Zh.A. Dysmenorrhea. Etiopathogenesis, differential diagnosis and therapy in the practice of a modern obstetrician-gynecologist. RMJ. “Mother and Child” No. 1 from 01/19/2012, p. 28.
- Zhikhareva N. S. Irritable bowel syndrome. Regular issues of "RMZh" No. 18 dated September 23, 2005, P. 1219.
- Petrov D.P. Irritable bowel syndrome. Consilium Medicum. 2009; No. 8, pp. 40-43.
- Kachalina O.V. Treatment of dysmenorrhea and premenstrual syndrome in an outpatient setting - modern possibilities. Difficult patient. 2015; 01-02: pp. 12-19.
- Instructions for use of the drug IMODIUM® Express
- Register of medicines in Russia. Active ingredients. Loperamide. https://www.rlsnet.ru/mnn_index_id_637.htm.
Find out more about IMODIUM® Express