The text is presented for informational purposes only. We strongly urge you not to self-medicate. When the first symptoms appear, consult a doctor. We recommend reading: “Why you can’t self-medicate?”
One of the indicators of digestive disorders is the detection of starch in feces. In medicine, this condition is called amilorrhea. During normal digestion, starch must be broken down into simple substances.
In childhood, starch in feces does not always indicate pathology due to the general immaturity of the body and the digestive system in particular.
Medical products (drugs, medicines, vitamins, dietary supplements) are mentioned for informational purposes only. We strongly do not recommend using them without a doctor's prescription. We recommend reading: “Why can’t you take medications without a doctor’s prescription?”
Extracellular and intracellular starch
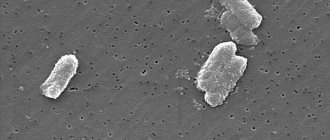
When deciphering the coprocytogram, the laboratory assistant indicates the type of starch that can be found in the stool:
- Intracellular starch. Contained inside a plant cell, which enters the digestive tract with plant foods. With normal peristalsis, the cell membrane has time to dissolve under the influence of gastric and intestinal juices, and starch should not normally be detected. If peristalsis is accelerated, then the chyme does not have time to be sufficiently processed and intracellular starch transits through the entire intestinal tube. Thus, the detection of this kind of starch indicates accelerated intestinal motility, while there may be no enzymatic deficiency.
- Extracellular starch. If the starch found in feces is not covered with a cell membrane, then it is called extracellular. Such starch is found when there is a deficiency of the enzyme amylase, which can break down complex carbohydrates. Thus, the presence of extracellular starch may indicate pancreatic insufficiency.
Causes
Depending on the age of the child, the appearance of starch in feces can be both a pathological and physiological indicator.
Non-pathological causes
Normally, it is possible to detect starch in the stool of:
- Child up to one year old. Extracellular and intracellular starch may be detected, since the digestive system is not yet mature, many foods are introduced for the first time. Enzymatic pancreatic insufficiency is a variant of the norm, in the absence of other clinical signs of pathology: fever, diarrhea, vomiting, and so on.
- Child under 2 years old. Intracellular starch may be detected in the presence of frequent bowel movements. At this age, the child switches from breastfeeding to general feeding and the motility of the gastrointestinal tube adapts to the changes. If milk or an adapted formula is digested quickly, then regular products should linger longer in the cavity of the gastrointestinal tube. This can lead to the fact that even the cell wall does not have time to dissolve.
If, along with the detection of starch in the stool, the mother notices other pathological signs (see below “Concomitant symptoms”), then a more in-depth examination should be carried out.
Pathological causes
- intestinal infections;
- pancreatitis of various etiologies;
- gastritis or gastropathy;
- helminthiases;
- inflammatory bowel diseases: enteritis, ulcerative colitis;
- fermentative dyspepsia and imbalance of intestinal microflora;
- irritable bowel syndrome.
Not only a colonoscopy: what will a stool test tell you?
Stool analysis is prescribed less frequently than other types of tests. However, in some cases you cannot do without it. Yulia Nikolaevna Okovitaya, a gastroenterologist at the Expert Clinic Smolensk, talks about why this analysis is important and how to properly prepare for it.
— Yulia Nikolaevna, what types of stool analysis exist?
— All studies are divided into two categories: general clinical and biochemical. General clinical tests include coprogram, stool analysis for eggs and larvae of helminths (worms), scraping for enterobiasis. A popular biochemical test is a stool test for occult blood.
— What parameters are paid attention to during analysis?
— Coprogram is a comprehensive study. First, organoleptic indicators are assessed: color, shape, consistency. This already provides a lot of information. Thus, black tarry stools (melena) indicate bleeding in the gastrointestinal tract. The so-called acholic stool (light-colored) is typical for patients with diseases of the hepatobiliary system.
Then the tissue composition is assessed. The presence of muscle fibers in the feces (creatorrhoea) indicates the accelerated passage of food through the gastrointestinal tract. Steatorrhea (presence of fat) indicates diseases of the pancreas or liver. Amilorrhea (excessive starch content) can also appear with enzymopathies and disruption of the pancreas.
A large number of intestinal epithelial cells, macrophages, erythrocytes, and leukocytes in the feces are a symptom of inflammation of the intestinal wall. The presence of Charcot-Leyden crystals makes one suspect helminthic infestations.
To diagnose parasitic diseases, stool is checked for the presence of helminths and protozoa. The occult blood test allows you to detect bleeding and suspect the presence of cysts and tumors.
— What types of stool analysis can be replaced with other studies?
— Testing for worm eggs can be easily replaced with a blood test. A blood test is even more reliable: it allows you to detect helminthiasis at any period, including before the parasite eggs enter the feces.
— What is more reliable when testing for Helicobacter pylori bacteria: stool analysis, rapid urease test or determination of antibody titer in the blood?
— The most effective method is histological examination of a fragment of the gastric mucosa obtained during gastroscopy. If for some reason this is not possible, it is better to combine the urease test with other methods.
Are you afraid to undergo gastroscopy? Perhaps our article will help you overcome your fear: “Where can you find the courage to make up your mind? Gastroscopy – without fear!”
— For what symptoms is this or that study prescribed?
— A coprogram is prescribed for signs of digestive disorders: abdominal pain, stool disorders, cramps, nausea, flatulence. Stool analysis is important for gastroenteritis. It is advisable to regularly test for occult blood in people after forty years of age in order to exclude cancer of the large intestine.
Today, the “gold standard” in identifying pathology of the large intestine is fibrocolonoscopy. Read more about this research method in our article
— Are there any contraindications to collecting stool samples?
— There are no contraindications as such. But there are situations in which stool analysis is not prescribed, as it will be useless. There is no point in testing women during menstruation. It is also not prescribed to people taking medications that change the color of the stool: barium, iron, etc. If the analysis is necessary, then, in agreement with the doctor who prescribed the drug, the use should be stopped two to three days before the collection of diagnostic material.
— What is the correct preparation for taking a stool test?
You must tell the doctor who ordered the test about all the medications you are taking. Those that may stain the stool should be discontinued two to three days before the test if possible. Please do not stop taking it without consulting your doctor. Also, two or three days before stool analysis, you should follow a certain diet: in particular, exclude foods that change the color of stool - beets, blueberries, black currants, bird cherry, food with food coloring.
Before the test, you should not take laxatives, use enemas or rectal suppositories.
The optimal volume of diagnostic material is two dosage spoons from a special container. But if stool is to be analyzed for helminth infections or for bacteriological culture, you need to take material from five or six different points.
It is important to use a special sterile container. Contact with other containers makes the diagnostic material less informative.
Remember that no more than five hours should pass from the moment of collecting the material for analysis to its delivery to the laboratory.
Interviewed by Daria Ushkova
The editors recommend:
Not always gastroscopy. Examination for abdominal pain
An insidious pain-mask. Does abdominal pain always indicate problems with the gastrointestinal tract?
MRI of the intestine and colonoscopy: complementary or alternative?
How to check the small intestine? We talk about CT enterography
For reference:
Okovitaya Yulia Nikolaevna
Graduate of the Faculty of Medicine of the Smolensk State Medical Academy in 2004.
From 2004 to 2006, she completed clinical residency in the specialty “General (family) medicine.”
Currently holds the position of general practitioner, gastroenterologist at Clinic Expert Smolensk. Receives at the address: st. 8 March, no. 20.
Associated symptoms
If the cause of the appearance of starch in the feces is pathological changes in the digestive system, then the mother should pay attention to the accompanying symptoms:
- abdominal pain;
- rumbling along the intestines;
- stool disorders in the form of diarrhea, increased stool volume;
- nausea;
- vomit;
- flatulence;
- intestinal colic;
- the presence of other pathological impurities in the stool: blood, mucus, undigested muscle fibers;
- temperature increase.
Method for detecting starchy compounds in feces in adults
Stool analysis to detect undigested starch is a coprogram. Here the entire digestive function is assessed. The coprogram includes the following indicators:
- consistency and color of stool;
- undigested food particles;
- fat;
- number of starch grains;
- muscle fibers;
- bacteria, protozoa, helminth eggs.
Using a coprogram, you can detect many pathologies that occur with damage to the gastrointestinal tract.
The presence of starchy compounds can be determined by the appearance of stool. They become abundant and soft. The color is yellowish-gray, the surface is shiny. The stool looks greasy and sticks to the walls of the toilet. A sharp unpleasant odor appears.
Treatment
Treatment of isolated amilorrhea should begin with diet therapy. If, upon repeated examination a month later, the results of the coprocytogram have not changed, then it is necessary to conduct an examination to identify the cause and initiate drug treatment of the underlying pathology.
Diet
The basic principles of diet therapy for a child who switches from breastfeeding to a common diet are:
- temporary restriction of plant foods;
- gradual introduction of new food products;
- mechanical and thermal processing of plant products.
In older age, it is necessary to direct nutrition to maximum unloading of the pancreas:
- limit the amount of sweets;
- avoid overeating (fractional meals in small portions 5-6 times a day);
- temporarily exclude fresh vegetables and fruits, fatty foods, and fried foods.
| Recommended Products | Not Recommended Products |
|
|
It is recommended to limit the consumption of cereals, as they contain a lot of starch and the load on the pancreas increases.
Drug therapy
If after a month of diet the tests have not improved, then after the examination the most often necessary groups of drugs are:
- Probiotics and prebiotics (Bifidumbacterin, Bifiform, Linex). Helps normalize microflora and improve peristalsis.
- Pancreatic enzymes (Creon, Pancreatin, Mikrasim). They are used as replacement therapy, allowing maximum relief of the pancreas for its restoration. The drugs are gradually withdrawn.
- Antidiarrheal drugs (Enterol, Bifiform). Allows you to normalize intestinal motility and improve digestion.
Specific treatment for the detected pathology is also prescribed: antibacterial therapy for intestinal infections, bacteriophages for dysbiosis, anthelmintic drugs for helminthiasis, and so on.