Drug-induced liver injuries are various types of liver damage caused by pharmacological agents. About 1000 drugs can allegedly cause drug-induced liver damage, and this effect has been proven in 40 drugs.
Drug-induced liver damage accounts for 9.5–15% of all adverse drug reactions. The incidence of drug-induced liver damage is 1 in 10–100 thousand people:
- 10% - acute hepatitis,
- 40% of acute hepatitis in patients over 50 years of age,
- death rate – 12% (international statistics).
A side effect of drugs is an unintended and unpredictable effect that develops when taking adequate doses of drugs for the purpose of treating or preventing various diseases.
The role of the liver in the human body
The role of the liver in the metabolism of chemicals entering the human body is extremely large. The liver is a multifunctional organ that performs a variety of functions.
- One of the most important is the detoxification function - the neutralization of toxic substances of endogenous and exogenous origin, the formation and elimination of non-toxic substances.
- The liver is involved in protein, carbohydrate, fat, vitamin and mineral metabolism, hormone synthesis, and hematopoiesis.
- The liver performs a function related to the formation of bile, which is involved in digestion.
- The liver is one of the most important organs in the human body.
Fatty steatosis
Under the influence of alcohol dehydrogenase, ethyl alcohol in hepatocytes is first broken down to form acetaldehyde, which is subsequently transformed in the reactions of the Krebs cycle to completely safe compounds: water and carbon dioxide. Therefore, irregular consumption of alcohol in reasonable quantities has virtually no effect on the condition of the hepatobiliary system.
But if ethanol regularly enters the body, the sequence of metabolic breakdown reactions is disrupted, resulting in the formation of excess amounts of cholesterol, lactate, palmate and other compounds that provoke the development of atherosclerotic disorders and fatty degeneration. Other toxic substances are also synthesized, which contribute to further necrosis of hepatocytes, and as a consequence, the progression of alcohol intoxication of the liver.
Clinical picture
In the vast majority of cases, steatosis is asymptomatic. As a rule, clinical signs are noticeable during an examination by a gastroenterologist or surgeon (pay attention to hepatomegaly). Only sometimes, especially after consuming fatty foods and alcohol, may the following occur:
- nausea;
- general discomfort, weakness;
- flatulence;
- diarrhea;
- dull, aching pain in the upper abdomen.
The role of drugs in human life
Modern medicines are a great achievement of scientific and technological progress. Thanks to the success of drug therapy in combination with other methods and means of treatment and prevention, mortality from infectious diseases (scarlet fever, diphtheria, tuberculosis, pneumonia, etc.), including especially dangerous ones (plague, cholera, smallpox), has significantly decreased. Practical medicine has highly effective drugs for diseases that were previously incurable or almost incurable (tuberculous meningitis, blood poisoning, cancer, etc.).
But at the same time, we must not forget about the other side of the coin - the complications and undesirable side effects of drugs, the frequency of which has been increasing over the past decades. This is a consequence of the imperfection of our knowledge of the intimate processes of the human body and medications, especially if there are several of them, insufficient knowledge of the properties and mechanisms of action of individual medications and their interaction in the body. Patients' access to medicines is of great importance; many medicines are dispensed without prescriptions; methods, doses and regimens for taking the drug are not followed; self-medication and trust in drug advertising are widespread among the population.
The importance of drinking regime in cleansing the liver after alcohol
When cleansing the liver of toxic substances, you need to drink a lot. Ethyl alcohol is a powerful diuretic. And when urinating, potassium, magnesium, and phosphorus, necessary for the restoration of hepatocytes, are excreted along with the liquid. Not only proper nutrition will help replenish the reserves of microelements, but also the use of compotes , jelly, fruit drinks from berries and fruits. The following drinks are especially useful:
- mineral and table waters;
- lightly brewed black or green tea;
- chamomile tea;
- kefir, fermented baked milk, Varenets, yogurt;
- juice from celery, carrots, beets, cabbage.
Rosehip decoction is a storehouse of substances needed by the liver. To prepare it, pour a handful of berries with 2 cups of boiling water, simmer for 10-15 minutes, cool and drink throughout the day. The diet should not contain carbonated drinks , which excessively irritate the mucous membranes, as well as coffee, strong tea and, of course, alcohol of any strength. Every day the body requires at least 2.5 liters of fluid (in the absence of contraindications).
Drug-induced liver damage and risk factors for their occurrence and development
- The dose of the drug and the duration of treatment, the concentration of the drug in the blood and the condition of the body itself.
- Patient's age. Drug-induced liver damage often develops in children under 3 years of age and increases after 40 years; with age after 60 years, the frequency and severity of liver damage increases.
- Floor. Women are more susceptible to developing drug-induced liver damage.
- Taking more than 6 drugs at the same time often leads to liver damage.
- Genetic characteristics of the liver, in which drug-induced damage is manifested by stagnation of bile in the liver (cholestasis).
- Alcohol leads to the fact that liver pathological reactions occur at lower doses of drugs; alcohol intake increases the severity of drug-induced liver damage.
- Background liver disease – any chronic liver disease is a risk factor for the development of drug-induced hepatitis.
Drug-induced liver damage occurs at different times when taking the drug, ranging from 1 week to 3 months from the start of treatment. The severity of drug-induced liver injury may be minimal and reversible before the development of non-alcoholic fatty liver disease, chronic hepatitis, cirrhosis and liver failure.
Cirrhosis
With cirrhosis, all the symptoms that previously arose due to hepatitis are aggravated. This:
- flatulence, stool disorders;
- stomach ache;
- jaundice;
- lack of appetite, weight loss;
- general weakness;
- manifestation of the vascular network on the skin (this is especially noticeable near the nose and eyes), multiple vascular “stars” on the body;
- skin itching;
- enlargement of the postauricular lymph nodes;
- gynecomastia, testicular atrophy in men;
- atrophy of the muscles of the shoulder girdle;
- fever with severe chills;
- nose and stomach bleeding.
Severe and persistent pain in the right side of the abdomen may indicate malignant hepatocellular carcinoma.
Mechanisms of action of drugs on the liver
The mechanisms of action of drugs on the liver are:
- direct effect of the drug on the liver cell (hepatocyte), this often depends on the dose of the drug and its toxic effect.
- There is also an indirect toxic effect of drug transformation products (metabolites) in the body, which no longer depends on the dose of the drug.
- The third type of liver damage includes direct and indirect effects of the drug (mixed damage).
Example. The drugs Roaccutane, Acnecutane (isotretionine is an isomer of vitamin A) are used to treat acne on the face (acne) and are prescribed for a long period of up to 4-6 months. During treatment, regular monitoring of liver function is required - before treatment, after the first month of treatment, then after 3 months. During treatment, there is often an increase in the level of liver enzymes (transaminases), in rare cases, acute hepatitis, which requires either a reduction in the dose of the drug or discontinuation of the drug, the prescription of drugs that restore liver function.
Basic methods of therapy
The main condition for successful treatment is a categorical refusal to drink alcohol. But doctors warn that restoration of liver function is only possible with steatosis. In other cases, you will have to take long-term (with a high degree of probability, lifelong) medication and a strict diet.
The course of therapy directly depends on the degree of damage to the hepatobiliary system and concomitant diseases. For steatosis the following is prescribed:
- preparations containing essential phospholipids;
- products based on ursodeoxycholic acid;
- medications based on ademetionine, an amino acid with a wide range of therapeutic effects: hepatoprotective, antidepressant, antioxidant, etc.
For hepatitis, in addition to the listed medications, corticosteroids, drugs to relieve the symptoms of hepatic encephalopathy, and parenteral replacement nutrition are sometimes used. Treatment of cirrhosis is usually symptomatic, since restoration of full liver activity at this stage of alcoholic illness is almost impossible. Often in such cases, organ transplant surgery can save a person’s life.
Fighting alcohol addiction
Overcoming the craving for alcohol is the key point in the treatment of alcohol intoxication of the liver. If a patient does not drink alcohol at all for six months, he will most likely be given a quota for a liver transplant (for cirrhosis or hepatitis that does not respond to drug therapy).
Only a few manage to cope with alcoholism on their own, and only in the early stages of addiction. Therefore, specialized medical narcologists recommend seeking professional help as soon as possible. In the treatment of alcoholism, we use the most modern techniques:
- drug and hypnotic coding;
- hardware detoxification procedures;
- courses of individual and group psychotherapy;
- physiotherapy;
- hardware effects on the central nervous system, etc.
The clinic operates a hospital with comfortable wards, and provides a service of calling a doctor to your home for detoxification or coding.
Only with the timely initiation of addiction treatment can the severe, incurable consequences of alcohol intoxication of the liver be avoided. It is important not to delay the start of treatment “for later” - it will only get worse, because various psycho-emotional disorders can be added to physiological disorders.
The text was checked by medical experts: Head of the socio-psychological service of the Alkoklinik MC, psychiatrist-narcologist L.A. Serova.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
Various drug-induced liver damage
Liver damage can develop with the use of various groups of drugs, here are some of them:
- antibiotics (tetracycline, erythromycin)
- antihelminthic drugs (mebendazole),
- antifungal agents (ketoconazole, fluconazole),
- non-steroidal anti-inflammatory drugs - NSAIDs (Diclofenac, the most used drug worldwide, causes side effects in 5 cases per 100 thousand people after 1-11 months of use),
- acetisalicylic acid,
- paracetamol,
- ibuprofen,
- allopurinol,
- quinidine,
- a nicotinic acid,
- hormonal drugs (oral contraceptives),
- statins (simvastatin, atorvastatin),
- antihypertensive drugs (nifedipine, enalapril),
- drugs affecting the nervous system, antidepressants (amitriptyline), tranquilizers (diazepam), antipsychotics (chlorpromazine),
- diuretics (furosemide, hydrochlorothiazide),
- iron supplements,
- medicinal herbs recommended as safe (valerian, chaparrel leaves, Dubrovnik, Chinese herbal preparations), etc.
Drug-induced liver injury, characterized by liver cell death (hepatocyte necrosis), can occur from the following drugs:
- paracetamol,
- methyldopa,
- isoniazid,
- ketoconazole,
- sulfonamides,
- quinidine,
- allopurinol,
- methotrescat,
- vitamin A,
- antibiotics, etc.
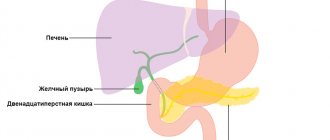
Stagnation of bile in the biliary system of the liver (cholestasis) can be caused by:
- sex hormones,
- erythromycin,
- nitrofurantoin,
- azathioprine,
- antithyroid hormones,
- antiarrhythmic drugs,
- antibiotics,
- oral contraceptives, etc.
Mixed forms of hepatitis, accompanied by cholestasis and necrosis of liver cells, can develop when using:
- hormonal drugs,
- antibiotics,
- antibacterial agents,
- antisecretory drugs (anti-acid H2 histamine blockers, etc.).
Drug-induced liver damage. Clinical manifestations
Most often, patients complain about:
- weakness, loss of appetite, nausea,
- yellowness of the sclera and skin,
- itchy skin.
With stagnation of bile (cholestatic hepatitis), the first symptom is jaundice, accompanied by itching, fever, dyspeptic symptoms (nausea, bitterness in the mouth, heaviness in the right hypochondrium), weakness, and decreased ability to work.
Upon inspection, the following is revealed:
- yellowness of the sclera,
- moderate enlargement of the liver,
- discolored stool and dark urine.
With a mixed type of acute drug-induced hepatitis, development begins with jaundice with a short pre-icteric period with the manifestation of dyspeptic disorders. Jaundice can last up to 2-4 weeks.
Acute drug-induced hepatitis is relatively rare and develops 5-7 days after starting medication. It is more common when you use the same drug multiple times or take multiple medications.
Drug-induced liver damage can initially occur covertly without a phase of acute hepatitis with general weakness, malaise, and decreased ability to work (asthenia). Liver damage in these cases is detected as an incidental finding in blood tests (blood biochemistry). All biochemical changes in the blood normalize after 2 weeks when the drug that caused the liver damage is completely discontinued. This form of liver damage can be caused by antibiotics, hormonal agents, anti-tuberculosis drugs, etc.
Hepatitis
The development period is individual, but on average it is about 7 years from the moment of the final formation of a stable addiction to strong drinks. It can occur in two forms:
- Persistent. It is considered more favorable, since inflammatory changes in the liver parenchyma can be dealt with, but only if one completely gets rid of the addiction and selects the right treatment.
- Progressive. It is accompanied by necrotic damage to organ tissue; in the absence of therapy, there is a high probability of cirrhosis. At this stage of alcohol intoxication of the liver, only partial restoration of its functions is possible, and in the future constant use of maintenance medications is required.
If, despite the worsening condition, a person continues to drink, an exacerbation of hepatitis is possible. However, the risk of death cannot be excluded.
Clinical signs
Depending on the symptoms, course and prognosis, pathology is divided into several types:
- Latent is the most favorable option, practically not accompanied by severe symptoms, and is often diagnosed only with instrumental or laboratory examination.
- Cholestatic - occurs in approximately 10-13% of cases. Characteristic changes in the color of the skin and whites of the eyes, and jaundice is accompanied by severe itching. The feces lighten, become almost white, the urine, on the contrary, becomes brownish.
- Jaundice - occurs more often than others. Worries include lack of appetite, digestive disorders, nausea with bouts of vomiting, yellowing of the sclera, skin and mucous membranes, pain in the projection of the liver. A non-critical increase in temperature is possible.
- Fulminant is the most dangerous variety. The disease progresses extremely quickly with the development of liver failure and coma. Even timely medical assistance may not bring results.
In addition, at the stage of hepatitis with alcoholic liver intoxication, the following are possible:
- arrhythmia, chest pain, shortness of breath and other symptoms of cardiomyopathy;
- excessive excitement or, conversely, lethargy;
- behavioral disorders;
- tremor of the limbs, eyelids, tongue;
- manifestations of pancreatitis, gastritis or gastric ulcer.
Alcohol poisoning of the liver significantly increases the likelihood of severe course and complications of various infections, pyelonephritis, and hormonal disorders.
Drug-induced liver damage. Diagnostics
The diagnosis of drug-induced liver damage is a diagnosis of exclusion, i.e., its diagnosis requires a thorough examination to identify other possible causes of symptoms and changes in liver parameters.
- Exclusion of viral, alcoholic and other liver damage.
- Medical history, diagnosis, analysis of medications taken.
- Laboratory diagnostics: ALT-alanine transferase, alkaline phosphatase, bilirubin with fractions (liver tests),
- Changes in clinical and laboratory parameters after discontinuation of the drug.
- Relapse of the disease when taking the drug again.
- Ultrasound of the gallbladder to rule out gallstones.
Diagnostic methods
- Anamnesis collection. It is important for the doctor to know about the duration of alcohol dependence, the approximate amount of alcohol consumed regularly, hereditary predisposition to cancer, diabetes, and atherosclerosis.
- Assessment of laboratory parameters. The patient is required to undergo a general and biochemical blood test, liver tests, lipid profile, and coagulogram. Pathology is indicated by a change in ESR, an increase in individual lipoproteins, triglycerides, cholesterol, liver enzymes, and C-reactive protein. To diagnose concomitant pathologies, tests for markers of viral hepatitis, urine examination, and detection of antibodies to parasites are important (for example, echinococcosis primarily affects the liver).
- Instrumental examination. First of all, an ultrasound is done. This diagnostic method is absolutely safe, has no contraindications and allows you to assess the size, echo structure of the liver, the presence of pathological neoplasms, and quickly examine surrounding tissues and organs. Elastography (FibroScan) is becoming increasingly popular - a method of non-invasive assessment of the condition of the liver; it is usually done simultaneously with an ultrasound examination. According to indications, a biopsy and computed tomography are performed.
Some of the listed studies are repeated during treatment to evaluate its effectiveness.
Treatment of drug-induced liver damage
Treatment of drug-induced liver injuries mainly involves discontinuation of the hepatotoxic drug with regular repetition of biochemical tests. Improvement occurs 1-2 weeks after discontinuation of the drug. Stagnation of bile (cholestasis) resolves more slowly. Patients often do not require a hospital stay.
But to eliminate liver dysfunction, it is recommended to prescribe hepatoprotectors:
- flavonoids (milk thistle fruit extract),
- antioxidants (ademetionine),
- derivatives of ursodeoxycholic acid (Ursofalk, Ursosan, etc.),
- essential phospholipids, phospholipid preparations, lipoic acid.
In addition to them, therapeutic nutrition is prescribed, sorbents are introduced, and symptomatic treatment is carried out. Doses and duration of treatment are adjusted by the doctor.
What causes pain after a feast?
If the normal functioning of the liver is disrupted, pain occurs after drinking alcohol. If the pain is not particularly severe, then doctors recommend completely stopping drinking alcohol and starting to eat properly (a gentle diet is recommended). If these conditions are met, hepatocytes will begin to recover on their own. Alcohol is only one of the factors that increases the likelihood of organ damage.
Pain due to alcoholism is caused by the following diseases:
- Fibrous liver disease
- Fatty infiltration of alcoholic type
- The alcoholic form of hepatosis at the primary stage occurs without any symptoms, but over time the hangover will be accompanied by pain and other symptoms - fever, severe nausea, vomiting, flatulence.
People who abuse alcohol for a long time begin to suffer from cirrhosis. With this disease, hepatomegaly occurs, which causes pain.
Prevention of drug-induced liver damage
Tips for minimizing side effects caused by medications:
- you should not take medications without a doctor’s prescription, based on, say, advertising, medications should be taken only according to indications,
- follow the recommendations for taking the drug: dose, regimen, duration of treatment,
- Avoid taking alcohol at the same time as taking medication,
- every person needs to know the medications to which adverse reactions have previously been observed, if any,
- avoid taking multiple medications at the same time, coordinating their use with your doctor, do not self-medicate,
- When purchasing a drug at a pharmacy, you need to look at the expiration date,
- the patient in 100% of cases must be aware of possible adverse reactions of the drug, the need for laboratory monitoring and subjective clinical manifestations during treatment,
- you need to read the annotations for the drugs and, together with the doctor, be an accomplice in your treatment, showing a responsible attitude towards your health, improving your medical culture.
Diet for poor liver condition
The goal of a gentle diet is to reduce the load on all digestive organs. Correcting the diet provides rest to the organs of the gastrointestinal tract, and especially the liver. Nutritionists recommend minimizing the consumption of salt, spices, and herbs that irritate hepatocytes and provoke the formation of edema. It is necessary to exclude semi-finished products, fast food, smoked meats, fatty meats, rich soups and broths from the diet. How to restore the liver after alcohol with the help of products:
- replenish the daily menu with fresh vegetables (in the form of salads), fruits, berries - broccoli, avocado, cucumbers, zucchini, apples, plums, figs, cranberries, raspberries, black and red currants;
- 2-3 times a week eat 100-150 g of fatty sea fish (salmon, herring, sardines) - the main source of polyunsaturated fatty acids valuable for the liver;
- start the day by eating a slice of dried white bread with a thin layer of butter to stimulate bile secretion;
- during breakfast or dinner, eat a bowl of buckwheat, oatmeal or millet porridge containing all B vitamins and complex carbohydrates;
- include vegetable puree soups in your diet, which are well digestible and quickly replenish energy reserves.
Do not boil or fry foods. They need to be baked, simmered in a small amount of water, stewed, or steamed. Meals should be fractional - 5-6 times, but in small portions. If you feel hungry before going to bed, it is better to snack on an apple or drink a glass of kefir. This will help not put a strain on the liver at night, when recovery processes are especially intense.