Gastritis is considered the most intractable disease among diseases of the gastrointestinal tract; it requires a lot of effort from the patient and a specialized approach to getting rid of the disease. Long-term treatment of gastritis and low rates of improvement in the patient’s condition from drug therapy often force one to turn to non-standard or non-traditional remedies that are practiced in folk medicine.
The healing properties of kombucha are legendary.
One of the components of the treatment of many diseases, including problems with the gastrointestinal tract, is kombucha, the healing properties of which have long been legendary. Many patients diagnosed with gastritis are interested in the question of whether it is possible to drink kombucha with gastritis, since curing the disease requires a careful approach to the selection of components included in the patient’s diet. In this article we will tell you how kombucha affects the organs of the digestive tract, what are the possibilities of its use depending on the etiology and evolution of the disease, and how to use this ingredient in alternative medicine.
The healing properties of kombucha
Humanity began using kombucha to treat diseases so long ago that today it is impossible to even name the sources of origin of this natural ingredient. It is known from unreliable sources that its origins occurred in Ceylon, after which it spread throughout foreign countries, and only at the beginning of the twentieth century came to Russia. This is a unique creature that cannot be classified either as a plant or as a community of the animal world, since its natural origin is based on an amazing symbiosis of living microorganisms, its structure is very similar to a mushroom. In addition to positive consumer reviews, there are many books written about the unique properties of kombucha, and there are also a considerable number of legends.
The healing properties of this component of therapeutic therapy include the following characteristics:
- Provides a preventive effect against cardiovascular diseases.
- It has a tonic effect on the human body.
- Reduces cholesterol levels.
- It has antibacterial properties that can inhibit the growth of pathogens and bacteria.
In addition, the use of mushroom kvass has a positive effect on the organs of the digestive system, namely:
- Stimulation of digestive processes by normalizing the secretory functions of the stomach with increasing acid levels. Helps improve metabolism and facilitate the digestion of ingredients entering the esophagus.
- Acids of organic origin contribute to the production of necessary digestive enzymes.
- Helps relieve constipation due to its ability to break down food.
- Reduces the level of inflammatory processes in the stomach and other organs of the human digestive system.
- It has regenerative properties, helping to restore damaged gastric epithelium from gastritis, and reduces the growth of pathogenic microorganisms.
- Reduces painful symptoms due to the presence of caffeine in the composition.
Drinking kombucha has a positive effect on the human nervous system, which helps increase its resistance to stressful situations. As you know, nervous tension is also often the cause of the development of gastritis or a provocateur of its exacerbation. Taking the mushroom significantly increases the patient’s chances of recovery.
Using kombucha for gastritis speeds up recovery
The use of kombucha in complex therapy of gastritis
Despite the many positive characteristics of kombucha, its use for diseases of the digestive system is not always possible. People diagnosed with gastritis know that the disease has significant differences, consisting in the peculiarities of the course of the disease, its origin, as well as the stage of development, as a result of which the direction of therapy and the lists of ingredients approved for use vary. The level of acid in the stomach has a significant impact on treatment, which directly affects the prescription of medications and the patient’s diet. Only a qualified gastroenterology specialist can determine this indicator based on analyzes and research results. It is important to discuss the possibility of using mushroom kvass as an auxiliary ingredient in therapy directly with the doctor, so that its use does not cause the progression of the disease.
Most often, doctors are not opponents of alternative medicine; they recognize its positive effects on the human body while the patient simultaneously complies with basic treatment instructions. Doctors allow drinking kombucha for gastritis with reduced gastric secretion, unless there are additional contraindications for this.
For gastritis with high acidity, the use of kombucha in its pure form is strictly prohibited, since taking it increases gastric secretion with the concomitant production of digestive enzymes, which may not only not improve the patient’s condition, but also contribute to the exacerbation or progression of the disease to more serious stages of its development .
We will tell you further how to prepare and consume kombucha for diseases of the gastrointestinal tract, so that its intake contributes to the patient’s recovery.
Let's sum it up
To the question of whether it is possible to drink kombucha for gastritis, we answer unequivocally in the affirmative. However, depending on the stage of development of the disease, its etiology, the dosage and method of preparing the potion differ.
A categorical ban on taking kvass is only during the period of exacerbation of the disease; during the period of remission, it is allowed even for gastritis with high acidity, only the intake must be agreed with the doctor, and the preparation must comply with the recipe.
Medusomycete or kombucha is a colony of microorganisms in symbiosis - acetic bacteria and yeast fungi. When infused, it turns the nutrient solution of sugar and tea leaves into a pleasant, refreshing drink, kombucha, which is used to treat many diseases. Most doctors strictly prohibit taking kombucha for stomach ulcers, although they recognize its beneficial effect on the gastrointestinal tract.
Doctors strictly do not recommend drinking kombucha if you have stomach ulcers.
Features of preparing and drinking kombucha for gastritis
You can prepare a healing drink yourself by buying a mushroom or growing it at home. To grow it, rosehip tea or black tea is most often used.
For the first recipe for growing a mushroom, you will need ten tablespoons of large-leaf tea and a liter of boiling water. The mixture is left to cool completely, after which it is filtered and poured into a glass container, or into a jar, fourteen tablespoons of sugar are added, covered with several layers of gauze and left to ferment in a dark and warm place for about a month and a half.
Growing a mushroom using rosehip decoction is done in a similar way, however, the recipe for preparing the mixture in which it will grow is slightly different. First, you need to steep the rose hips in a thermos for five days. To prepare the decoction you will need four tablespoons of rose hips per half liter of boiling water. The finished potion is poured into a glass container, a decoction of black tea is added to it, at the rate of one tablespoon per two hundred milliliters of boiling water, and left to ferment in the same way as in the previous case.
Ready-made kombucha needs regular care and rinsing for the healing drink to have a positive effect on the human body. It can be propagated by separation or infusion.
If gastric secretion is reduced, you can consume the mushroom about two hours before meals. It is recommended to drink one glass of infusion every day for a month, after which a break is taken. By increasing the level of pepsin in the stomach, its digestive functions are activated and acidity is normalized. When consuming kombucha, you should not abandon traditional methods of therapy; you must follow doctor’s orders, as well as comply with special nutritional requirements. In addition, it is not recommended to take the infusion during an exacerbation of the disease, as it can harm the stomach and contribute to the progression of the disease. To enhance the effectiveness of kvass, it is often combined with various healing herbal infusions. A very popular combination is a mushroom drink with an infusion of mint and centaury. For medicinal purposes, it can be taken for four months, with intervals of about a week between doses.
For increased gastric secretion, honey is added to kombucha
If the secretion of the stomach is increased, then kombucha is consumed with the preliminary addition of honey, which can neutralize the acid level in the potion, thereby reducing its provocation of the production of gastric juice. To prepare a healing drink, you will need a spoonful of honey per two hundred milliliters of drink. It is recommended to take this potion for medicinal purposes for a month, two hundred milliliters three times a day according to the following system: in the morning - half an hour before meals, in the afternoon - two hours before lunch, in the evening - three hours before meals. The patient will feel improvements in the digestive system already on the second day of taking this potion; the drink will help reduce pain symptoms in the epigastric region, and also relieve the feeling of heaviness in the stomach after eating. Such a drink is allowed to be taken only after the patient has ruled out allergic reactions to bee products.
Helicobacter pylori and Candida fungi: what do they have in common in a gastroenterological patient?
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– Now we give the floor to Professor Yuri Pavlovich Uspensky. Yuri Pavlovich will talk about Helicobacter pylori and fungi of the genus Candida, what they have in common in a gastroenterological patient.
Yuri Pavlovich Uspensky , professor, doctor of medical sciences:
– Dear colleagues, we know very well that thanks to the epoch-making discovery of the colossal role of Helicobacter pyloricus in the development of chronic gastritis, peptic ulcers, stomach cancer, by the end of the 90s it became obvious that the number of newly identified cases of peptic ulcers was decreasing, that even made it possible for gastroenterologists to declare that the 20th century is the century of disappearing peptic ulcer disease, and the 21st century is the century of emerging gastroesophageal reflux disease.
However, unfortunately, recent trends have turned out to be not so optimistic and the main problems are still associated with the decreasing effectiveness of eradication therapy. The reasons for this lie in the increasing resistance of Helicobacter pylori to antibacterial drugs that are part of traditional eradication therapy regimens.
Thus, one of the patriarchs, Professor F. Megraud, noted that resistance to clarithromycin, according to molecular genetic methods, in Europe reaches 46%. What happens then? In this case, there is a dramatic decrease in the effectiveness of eradication therapy, which does not exceed 18%. As for the Russian Federation, the range of variations in clarithromycin resistance is very wide. For some reason, in our northwestern region, resistance to clarithromycin is highest in St. Petersburg. Moreover, these were completely independent studies: the pediatric enclave of Professor E.A. Kornienko, our research of Dr. N.V. Baryshnikova, research from the Pasteur Institute. Moreover, there were different methods, and they all gave extremely high (more than 30%) figures of resistance to clarithromycin.
Colleagues, speaking about new antibacterial drugs as an option to overcome antibiotic resistance and increase the effectiveness of eradication therapy, I would like to say that this path is still quite dangerous, and maybe even a dead end, because by doing so we contribute to the development of multiresistant strains to antibiotics Helicobacter pylori.
And in fact, the uncontrolled consumption of antibiotics is a global problem for humanity. Not so long ago, on November 18, 2012, the European Day of Awareness of the problem of resistance and consumption of antibiotics was held, when a global strategy was proposed to combat the spread of resistant forms of microorganisms.
What to do in these conditions? In these conditions, one must be guided by the considerations that, as the great Spanish playwright Lope de Vega wrote: “Progress is the best, and not just the new.” Tatyana Lvovna has already mentioned today that there is now a certain renaissance of eradication schemes based on bismuth preparations in both the first and second line therapy of Helicobacter pyloric eradication. Indeed, bismuth preparations have a number of advantages associated with both their own anti-Helicobacter action and the cytoprotective effect, a positive effect on the quality of the formed post-ulcer scar. There is no primary resistance to bismuth and no secondary resistance is formed; it does not have a negative effect on the composition of the intestinal microflora. And according to Professor A.I. Parfenova in some cases acts as an intestinal antiseptic, inhibiting the growth of opportunistic pathogens, and it does not cause the development of antibiotic-associated diarrhea.
The direct effect of bismuth preparations on Helicobacter pylori has been demonstrated in a number of well-organized studies, and these actions were associated with blocking the adhesion of Helicobacter with direct inhibition of the enzymes and urease of this microorganism.
In addition, in recent years, the concept of the actively developed school of Professor Kononov in Omsk has been established that even in the case of successful eradication therapy, an inflammatory infiltrate is formed (due to the production of cytokines, due to the production of reactive oxygen species), and it persists for quite a long time – from 1 to 12 months. Therefore, in this regard, the inclusion of bismuth preparations in the complex of eradication therapy is justified from a clinical point of view, because this suppresses associated inflammation due to a decrease in the production of cytokines, an increase in the production of cytoprotective prostaglandins, and, accordingly, an increase in epidermal growth factor.
Such a classic of Helicobacteriology as P. Malfertheiner in one of his works stated that the addition of bismuth to first-line therapy can maintain high eradication efficiency even with resistant strains. In this case, monitoring of growing resistance to Clarithromycin is not required.
Which bismuth-containing eradication scheme is preferable? The regimen that we just talked about, when bismuth is added to standard therapy, and the 10-day regimen that Tatyana Lvovna spoke about (bismuth, metronidazole, tetracycline and a proton pump inhibitor) have a right to exist. All of them provide a fairly high and effective level of eradication.
What is the connection between Helicobacter pyloricus and Candida fungi? According to our studies, it turned out that the same patients express genes that encode both pathogenicity factors of Helicobacter pylori and factors of adhesion and invasion of fungi of the genus Candida. And fungi of the genus Candida albicans do have virulence factors, adhesion factors, and invasion factors. The connection between the concentration of Candida fungi in the colon and the degree of Helicobacter pylori contamination in the antrum of the stomach is quite clearly expressed and was demonstrated 10 years ago in the works of M.M. Zakharchenko.
What happens under the influence of antibacterial therapy with fungi of the genus Candida? Their population is steadily growing as a result of a direct stimulating effect (there is evidence that patients with candidemia, that is, with candidosepsis, received 4 or more antibiotics), as well as due to the inhibitory effect on antagonistic bacteria of fungi of the genus Candida.
What are fungi of the genus Candida? Look, these data show that, it turns out, these are transient microorganisms; they are found in ice cream and other fermented milk and dairy products. That is, at first glance, there is nothing terrible in their presence; they pass through the human body in transit. But this happens only when the immunological reactivity of the macroorganism is sufficiently high. And if it is low, if this is a person suffering from immunodeficiency, receiving hormonal therapy, if this is a weakened patient, then there is a real risk of invasion of fungi of the genus Candida in the mucous membrane, the development of candidiasis of the esophagus, colon, translocation of the microbe through the intestinal wall, up to the development of candidemia and candidosepsis .
In some cases, with reduced immune resistance of the macroorganism, invasive candidiasis does not develop, but non-invasive candidiasis may develop when the concentration of Candida fungi in the intestinal lumen increases. But even at the same time, the situation is far from favorable, because under these conditions there is sensitization, intoxication of the body, the formation of secondary immunodeficiency and the addition of a mixed infection. Because fungi of the genus Candida have a number of enzymatic, polysaccharide and other factors of aggression and pathogenicity.
The criterion for diagnosing non-invasive intestinal candidiasis and increased proliferation of fungi of the genus Candida is a decrease in the number of normobiota below 100 million colony-forming units per gram of feces and the growth of fungi of the genus Candida ssp. when stool cultures are greater than 1000 colony-forming units per gram of feces.
The presence of a close pathogenetic relationship between fungi and Helicobacter is confirmed by the fact that Helicobacter pylori is detected in 98% of samples of fungi of the genus Candida isolated from the mucosa. And most samples contain the cag A pathogenicity island gene.
Another study showed that the presence of Helicobacter pylori genes is also identified from fungi isolated from the oral cavity, and in almost 100% of cases homology is observed between the fungal genes and the genes of the control Helicobacter population.
According to domestic work, in children with HP-associated gastroduodenitis, the number of highly pathogenic strains of the microorganism Helicobacter pylori increases with age. But at the same time, the growth of such strains is associated with an increase in the sap2 gene. This is a gene that encodes the synthesis of the virulence factor of fungi of the genus Candida from 41.2% to 100% in children over 17-18 years of age.
Thus, in recent years, the concept has emerged that yeast-like micromycetes are a natural biological reservoir for fungi of the genus Candida. That is, what happens in this case? Tatyana Lvovna has already spoken today about survival strategies for Helicobacter pyloricus. But they are not limited to urease activity alone. The fact is that Helicobacter is generally a very vulnerable organism, extremely sensitive to temperature conditions and to food and bile detergents. Therefore, for its survival, it is able to penetrate the capsule and cell wall of the fungus of the genus Candida, adhere to the plasma membrane of the fungus to form a vacuole and be located inside this organism, acquiring resistance to changing environmental conditions, including temperature, food and bile detergents.
Here is a very interesting job that was completed 10 years ago. It shows that the relationship between fungi and Helicobacter is, in fact, equipotential. This combination also increases the virulence of fungi of the genus Candida. And the eradication therapy, even if successful, significantly reduces the frequency of detection of Helicobacter in the stomach, but increases the frequency of detection of Candida fungi.
What to do in this situation? Apparently, it is necessary to search for innovative approaches to the diagnosis and correction of candidiasis in these types of patients. And the difficulty lies in the fact that among the treatment methods traditionally accepted in gastroenterology, methods aimed at preventing the expansion of Candida spp. are essentially absent. As well as there is no anti-candidal activity in all antibacterial agents included in classical eradication therapy. Meanwhile, such ways must be sought, because fungi, as we have already said, are capable of populating other anatomical and ecological niches of the body in addition to the intestines and fully exhibiting their pathogenic properties.
Ways to minimize the risk of development and progression of candidiasis of the digestive organs when using eradication therapy include excluding antibiotics with potentially high resistance to them from the eradication complex and including bismuth drugs in first-line therapy. In addition, some patients require additional prescription of non-resorbable antimycotic drugs.
Older drugs of this generation included and still include, for example, Nystatin. However, this drug still cannot be considered a drug of choice in modern conditions, because it has a wide range of side effects and has a number of contraindications, including peptic ulcer disease, pancreatitis, pregnancy and lactation.
And a worthy alternative, which has all the advantages and is devoid of all the disadvantages of drugs in this group, is Pimafucin (Natamycin) - an antimicrobial polyene antimycotic that acts only inside the lumen of the intestinal wall. Unlike Nystatin, resistance does not develop to Natamycin even with long-term use. This drug is produced in an enteric coating, therefore, it is protected from destruction in the acidic gastric environment. As already mentioned, it can be used during pregnancy, for children of any age, one tablet (100 mg) 4 times a day, usually for 5-10 days.
Gynecologists know this drug, Pimafucin, well and actively use it in their clinical practice. But since human ecological niches and endobiocenoses are essentially like communicating vessels, there is a need in the presence of candidiasis, for example, thrush, to necessarily identify the presence of candidiasis of the digestive organs and apply appropriate efforts to correct this situation.
What are the categories of patients for whom additional inclusion of the antimycotic “Pimafucin” in the eradication therapy complex or its administration within 7-10 days after eradication is indicated? These are patients in whom clinical and laboratory criteria for candidiasis are determined; these are patients who have already undergone eradication therapy; who received a course of antibiotic therapy for various reasons; immunocompromised patients, patients receiving radiation or hormonal therapy; patients who show signs of candidiasis of other digestive organs.
Of course, “Pimafucin” (“Natamycin”) is absent from both international and Russian recommendations, but our medicine is not dogmatic, it develops according to the clinical needs of our patients. More recently, we did not talk about the fact that probiotics can be used in Helicobacteriology, and according to the IV Maastricht Agreement, probiotics can be used as adjuvant therapy to improve the safety of therapy.
For now, let me conclude that candidiasis of the digestive organs is an interdisciplinary problem and its solution requires integration of the efforts of gastroenterological and mycological services. The high representation of fungi of the genus Candida in the gastrointestinal microflora is associated with the density of bacterial contamination and the virulence of the microorganism Helicobacter pylori. A promising way to increase the effectiveness and safety of eradication therapy, as well as the elimination of fungi of the genus Candida and the prevention of the progression of candidiasis of the digestive organs, is the additional inclusion of bismuth preparations and non-resorbable antimycotics in the eradication therapy regimens for those groups of patients that we talked about above.
Thank you for your attention.
Contraindications for use
The presence of many useful components, vitamins and microelements in the mushroom does not make it a universal remedy for getting rid of any diseases. In addition to the positive effect on the human body, it can provoke a deterioration in health if the patient’s pathogenesis includes the following diseases:
- Ulcerative diseases of the digestive system, especially in the acute stage.
- The presence or prerequisites for the development of diabetes mellitus, since the drink contains a huge amount of sucrose.
- Fungal diseases in the body of different stages and locations.
- Allergic reactions to the constituent components of kombucha.
- Bronchial asthma.
- Overweight with a diagnosis of obesity, due to excessive amounts of nutrients and calories in the drink.
As you can see, the positive characteristics of drinking do not indicate its harmlessness to human health. Before drinking mushroom kvass, you must undergo an examination at a medical institution to determine an accurate diagnosis, and only after consulting with your doctor, include the drink in your diet.
Check with your doctor before drinking kombucha
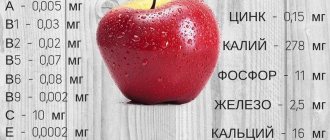
Kombucha composition
What is Kombucha? This product is formed as a result of the fermentation of ordinary tea. In its composition, several groups of microorganisms can be identified at once - bacteria and yeast, forming a symbiosis. There are a huge number of similar variations of their combination, because each such drink has its own unique chemical composition. As a result of their vital activity, microbes produce large amounts of useful substances and acetic acid. Kombucha tastes like kvass.